What is the ICD 10 code for kyphoscoliosis?
M40.209 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM M40.209 became effective on October 1, 2021. This is the American ICD-10-CM version of M40.209 - other international versions of ICD-10 M40.209 may differ. kyphoscoliosis ( M41.-)
What is the ICD 10 code for balloon kyphoplasty?
ICD-10-CM1 Diagnosis Codes Diagnosis codes are used by both physicians and hospitals to document the indication for the procedure. Balloon kyphoplasty is performed for pathological fractures of the vertebrae due to osteoporosis and other underlying conditions as labeled.
Are kyphoplasty procedures being denied due to s codes?
Our Medicare billing rep is saying our kyphoplasty procedures are being denied when used with the compression fracture dx (S codes), that we have to use the osteoporosis or malignant related fractures. This change to the LCD was effective in July. I guess I have been living under a rock! Is this true?? Your wires are crossed.
What is the LCD for vertebroplasty/kyphoplasty?
The information in this article contains billing, coding or other guidelines that complement the Local Coverage Determination (LCD) for Vertebroplasty/Kyphoplasty L33473. Procedure codes may be subject to National Correct Coding Initiative (NCCI) edits or OPPS packaging edits.
What is the ICD-10 PCS code for kyphoplasty?
I n code M84. 58XA, “other specified site” includes vertebrae per ICD-10-CM inclusion notes.
How do you code kyphoplasty?
Since there is no regular CPT code for the procedure being performed at a cervical level, use the unlisted CPT code 22899 for a cervical kyphoplasty procedure.
What type of surgery is kyphoplasty?
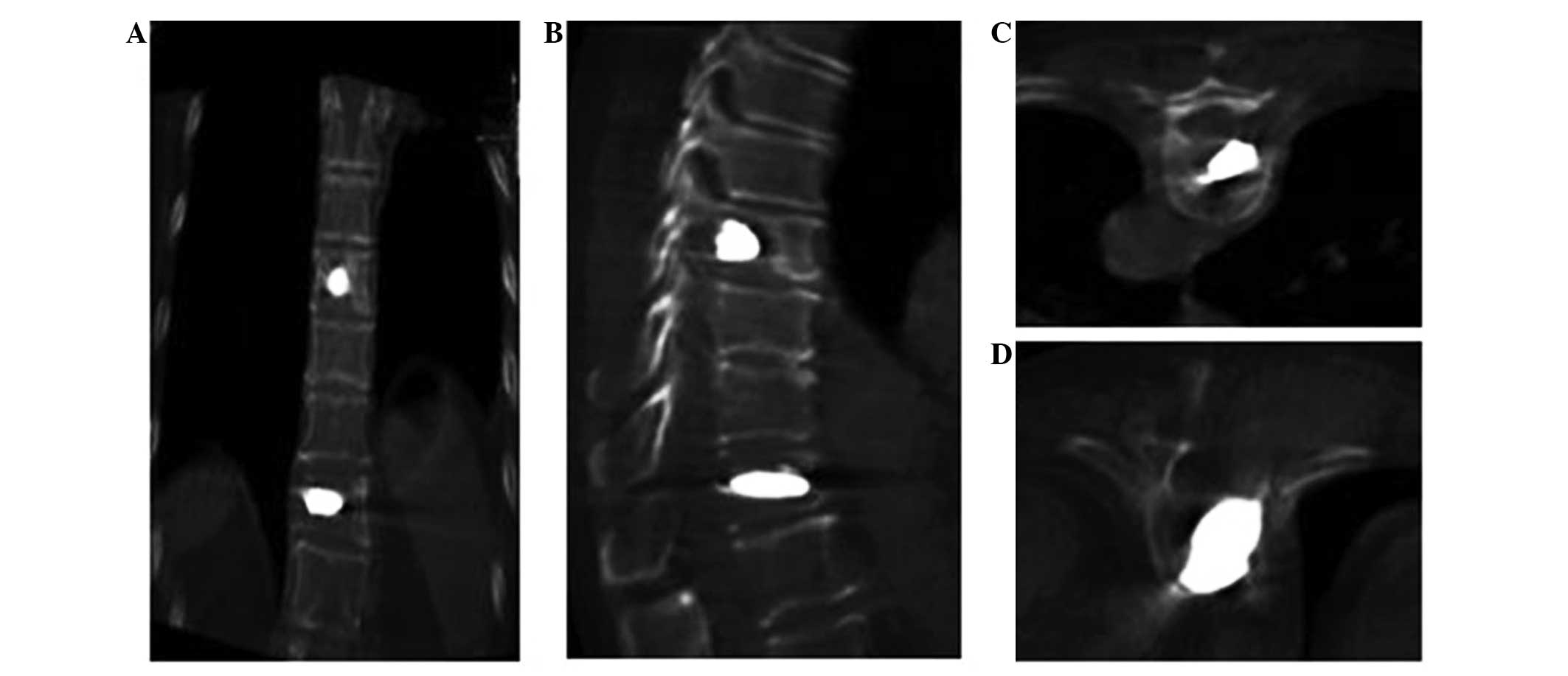
kyphoplasty: a minimally invasive procedure used to treat vertebral compression fractures by inflating a balloon to restore bone height then injecting bone cement into the vertebral body.
Is a kyphoplasty a fusion?
The most common surgical procedures for spinal compression fractures are lumbar fusion and vertebroplasty/kyphoplasty. In a lumbar fusion, the vertebrae are connected with rods. Minimally invasive lumbar fusion joins the bones of the spine in the lower back together so that there is no longer any motion between them.
What is the ICD 10 code for compression fracture?
000A for Wedge compression fracture of unspecified thoracic vertebra, initial encounter for closed fracture is a medical classification as listed by WHO under the range - Injury, poisoning and certain other consequences of external causes .
What is the ICD 10 code for lumbar compression fracture?
Wedge compression fracture of first lumbar vertebra, initial encounter for closed fracture. S32. 010A is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM S32.
What is kyphoplasty medical term?
Kyphoplasty is a surgical procedure that expands and stabilizes compression fractures of the spine. It is a type of vertebral augmentation surgery.
What is the meaning of kyphoplasty?
Kyphoplasty is used to treat painful compression fractures in the spine. In a compression fracture, all or part of a spine bone collapses. The procedure is also called balloon kyphoplasty.
Is kyphoplasty the same as vertebroplasty?
Vertebroplasty and kyphoplasty are relatively new techniques for the treatment of pain caused by vertebral body compression fractures. Kyphoplasty differs from vertebroplasty in that a balloon is first inflated in the vertebral body to create a cavity into which cement is then injected under lower pressure.
When is kyphoplasty indicated?
Kyphoplasty/vertebroplasty are generally reserved for people with painful progressive (increasing) back pain caused by osteoporotic or pathologic vertebral compression fractures. Candidates for these procedures often have a reduced ability to move and function because of the fractures.
Is a compression fracture a broken back?
A compression fracture occurs when the front of a vertebra breaks and loses a little of its height, but the back of that vertebra remains intact. Symptoms include pain in the back and sometimes in the arms or legs.
Is laminectomy the same as decompression?
Cervical laminectomy It usually involves removing a small piece of the back part (lamina) of the small bones of the spine (vertebrae). Laminectomy enlarges the spinal canal to relieve pressure on the spinal cord or nerves. Laminectomy is often done as part of a decompression surgery.
Can CPT 22513 and 22514 be billed together?
Percutaneous vertebral augmentation including cavity creation using mechanical device of one vertebral body must be reported with CPT codes 22513 (thoracic), 22514 (lumbar) and 22515 (each additional thoracic or lumbar vertebral body [list separately in addition to code for the primary procedure]).
What is procedure code 22511?
22511. PERCUTANEOUS VERTEBROPLASTY (BONE BIOPSY INCLUDED WHEN PERFORMED), 1 VERTEBRAL BODY, UNILATERAL OR BILATERAL INJECTION, INCLUSIVE OF ALL IMAGING GUIDANCE; LUMBOSACRAL.
What is the difference between kyphoplasty and vertebroplasty?
Vertebroplasty and kyphoplasty are relatively new techniques for the treatment of pain caused by vertebral body compression fractures. Kyphoplasty differs from vertebroplasty in that a balloon is first inflated in the vertebral body to create a cavity into which cement is then injected under lower pressure.
What is the CPT code 22513?
CPT® Code 22513 - Percutaneous Vertebroplasty and Vertebral Augmentation Procedures - Codify by AAPC. CPT. Surgical Procedures on the Spine (Vertebral Column) Percutaneous Vertebroplasty and Vertebral Augmentation Procedures.
What is the correct coding for bilateral percutaneous vertebroplasty?
For example, a surgeon documents bilateral percutaneous vertebroplasty at vertebral segments T12 and L1. Proper coding is 22510, 22512.
When reporting vertebroplasty, what is the code selection?
When reporting vertebroplasty, code selection depends on the location and number of vertebral bodies treated. Choose a single “initial level” code based on the location of the first vertebral body treated:
Can you code vertebroplasty and bone biopsy at the same time?
Percutaneous vertebroplasty codes include the two procedures most commonly performed during the same session—imaging guidance and bone biopsy (e.g., Biopsy, bone, trocark or needle; deep (eg, vertebral body, femur)—and therefore you may not code seperately for them at the same level.
Is modifier 50 for 22513-22515?
Code descriptor for 22513-22515 specify “unilateral and bilateral;” therefore, modifier 50 is not appropriate
Is kyphoplasty a plus?
Kyphoplasty Is Like Vertebroplasty “Plus”. Percutaneous vertebral augmentation (a.k.a., kyphoplasty or balloon-assisted percutaneous vertebroplasty ) is a similar to vertebroplasty, but includes the use of an inflatable balloon to “jack up” the damaged vertebra (e) prior to methylmethacrylate injection.
What is a Z40-Z53?
Categories Z40-Z53 are intended for use to indicate a reason for care. They may be used for patients who have already been treated for a disease or injury, but who are receiving aftercare or prophylactic care, or care to consolidate the treatment, or to deal with a residual state. Type 2 Excludes.
When will the ICD-10 Z48.89 be released?
The 2022 edition of ICD-10-CM Z48.89 became effective on October 1, 2021.
What is an ABN modifier?
Advance Beneficiary Notice of Non-coverage (ABN) Modifier Guidelines An ABN may be used for services which are likely to be non-covered, whether for medical necessity or for other reasons. Refer to CMS Publication 100-04, Medicare Claims Processing Manual, Chapter 30, for complete instructions.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS), the federal agency responsible for administration of the Medicare, Medicaid and the State Children's Health Insurance Programs, contracts with certain organizations to assist in the administration of the Medicare program. Medicare contractors are required to develop and disseminate Articles. CMS believes that the Internet is an effective method to share Articles that Medicare contractors develop. While every effort has been made to provide accurate and complete information, CMS does not guarantee that there are no errors in the information displayed on this web site. THE UNITED STATES GOVERNMENT AND ITS EMPLOYEES ARE NOT LIABLE FOR ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION, PRODUCT, OR PROCESSES DISCLOSED HEREIN. Neither the United States Government nor its employees represent that use of such information, product, or processes will not infringe on privately owned rights. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information, product, or process.
What modifier is used for non-covered services?
Effective from April 1, 2010, non-covered services should be billed with modifier –GA, -GX, -GY, or –GZ, as appropriate.
When to use modifier GX?
Modifier GX (“Notice of Liability Issued, Voluntary Under Payer Policy”) should be used when the beneficiary has signed an ABN, and a denial is anticipated based on provisions other than medical necessity, such as statutory exclusions of coverage or technical issues. An ABN is not required for these denials, but if non-covered services are reported with modifier GX, Part A MAC systems will automatically deny the services.
What does "you" mean when acting on behalf of an organization?
If you are acting on behalf of an organization, you represent that you are authorized to act on behalf of such organization and that your acceptance of the terms of this agreement creates a legally enforceable obligation of the organization. As used herein, “you” and “your” refer to you and any organization on behalf of which you are acting.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.

Popular Posts:
- 1. icd-9 code for diabetes with neurological manifestations
- 2. icd 9 code for poor fetal growth
- 3. icd 10 code for 244.9
- 4. icd 10 code for mercury randome urine
- 5. icd 10 code for left lateral ankle wound, stage ii
- 6. icd 10 code for post op pneumoperitoneum
- 7. icd 10 code for non family member perpatraitor
- 8. icd 10 code for mbd
- 9. icd 10 code for rheumatoid arthritis of foot
- 10. icd 9 code for diabetes with microalbuminuria