What is the ICD 10 code for DJD?
ICD-10-CM Diagnosis Code K21.0 Gastro-esophageal reflux disease with esophagitis 2016 2017 2018 2019 2020 2021 - Converted to Parent Code 2022 Non-Billable/Non-Specific Code
What does ICD - 10 stand for?
· 2022 ICD-10-CM Diagnosis Code K20.9 2022 ICD-10-CM Diagnosis Code K20.9 Esophagitis, unspecified 2016 2017 2018 2019 2020 2021 - Converted to Parent Code 2022 Non-Billable/Non-Specific Code K20.9 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail.
What are ICD 10 codes?
· Esophagitis, unspecified without bleeding 2021 - New Code 2022 Billable/Specific Code K20.90 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM …
What is the ICD 10 diagnosis code for?
ICD-10 Index. Diseases of the digestive system (K00–K93) Diseases of esophagus, stomach and duodenum (K20-K31) Esophagitis (K20) K20 - Esophagitis NON-BILLABLE CODE; K20.0 - Eosinophilic esophagitis BILLABLE CODE; K20.8 - Other esophagitis NON-BILLABLE CODE; K20.80 - Other esophagitis without bleeding BILLABLE CODE
What is La Grade D esophagitis?
In contrast, LA-D esophagitis is defined as one or more mucosal breaks involving 75% or more of the esophageal circumference (Figure 2). LA-D is the most infrequently encountered grade of reflux esophagitis.
What does LA grade D mean?
LA grade D reflux disease is defined by one or more mucosal breaks that involve at least 75% of the esophageal circumference. 02:51. This is demonstrated in this patient who has ulceration in the mucosa involving the whole of the circumference of the esophagus.
What causes Grade D esophagitis?
Esophagitis is caused by an infection it is treated with medications to cure the infection. Esophagitis is caused by acid reflux or GERD, the condition is treated with medications to reduce or block acid production, for example, heartburn drugs such as H2 blockers or proton pump inhibitors (PPIs).
What does LA Grade C reflux esophagitis mean?
Severe reflux esophagitis – LA grade C + D LA grade C: erosion(s) extending over mucosal folds, but over less than three-quarters of the circumference. LA grade D: confluent erosions extending over more than three-quarters of the circumference (circular defects).
What are the different types of esophagitis?
The common forms of esophagitis include reflux esophagitis, infectious esophagitis, pill esophagitis, eosinophilic esophagitis, and radiation and chemoradiation esophagitis. Candida esophagitis (see the image below) is the most common type of infectious esophagitis.
Is Barrett's esophagus the same as erosive esophagitis?
Conclusions: Erosive esophagitis is often associated with Barrett's esophagus. The severity of inflammation is associated with an increased risk of harboring this condition. Patients with erosive esophagitis should have a second look endoscopy to evaluate for Barrett's esophagus.
What is the ICD 10 code for esophagitis?
Esophagitis, unspecified without bleeding K20. 90 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM K20. 90 became effective on October 1, 2021.
Is reflux esophagitis the same as GERD?
Reflux esophagitis is an esophageal mucosal injury that occurs secondary to retrograde flux of gastric contents into the esophagus. Clinically, this is referred to as gastroesophageal reflux disease (GERD).
What are the stages of esophagitis?
GERD is broken down into different stages based on how serious your symptoms are and how often they occur:Stage 1: Mild GERD. Minimal acid reflux occurs once or twice a month. ... Stage 2: Moderate GERD. ... Stage 3: Severe GERD. ... Stage 4: Precancer or cancer.
What is Grade 2 erosive esophagitis?
Grade II is defined as multiple erosive lesions, noncircum-ferential, affecting more than one longitudinal fold, with or without confluence [1].
How do you treat grade B esophagitis?
Depending on the type of esophagitis you have, you may lessen symptoms or avoid recurring problems by following these steps:Avoid foods that may increase reflux. ... Use good pill-taking habits. ... Lose weight. ... If you smoke, quit. ... Avoid certain medications. ... Avoid stooping or bending, especially soon after eating.More items...•
What is erosive reflux oesophagitis?
Erosive esophagitis is a type of esophagitis in which there is esophageal damage. Esophagitis is inflammation, irritation, or swelling of the lining of the esophagus, which is the tube that runs from the throat to the stomach.
How do you get esophagitis?
Esophagitis is caused by an infection or irritation in the esophagus. An infection can be caused by bacteria, viruses, fungi, or diseases that weaken the immune system. Infections that cause esophagitis include: Candida.
What infections cause esophagitis?
Infectious esophagitis is relatively rare and occurs most often in people with poor immune system function, such as people with HIV / AIDS or cancer. A fungus normally present in the mouth called Candida albicans is a common cause of infectious esophagitis.
What bacteria causes esophagitis?
These include Staphylococcus aureus, Staphylococcus epidermidis, Streptococcus viridans, and Bacillus species [8]. Although bacterial esophagitis has not been well characterized, Walsh et al.
Can esophagitis be caused by stress?
Reflux esophagitis is significantly associated with psychosocial stress, and the severity of reflux esophagitis correlates with the degree of stress.
What tests are used to diagnose eosinophilic esophagitis?
Doctors may use various tests to make a diagnosis. These include imaging tests, an upper endoscopy, and a biopsy.
What is the most common problem with the esophagus?
The most common problem with the esophagus is GERD (gastroesophageal reflux disease). With GERD , a muscle at the end of your esophagus does not close properly. This allows stomach contents to leak back, or reflux, into the esophagus and irritate it. Over time, GERD can cause damage to the esophagus.
When is the ICd 10 code for K20.90?
K20.90 is new to ICD-10 code set for the FY 2021, effective October 1, 2020. The National Center for Health Statistics (NCHS) has published an update to the ICD-10-CM diagnosis codes which became effective October 1, 2020. This is a new and revised code for the FY 2021 (October 1, 2020 - September 30, 2021).
What are the conditions that contribute to reflux esophagitis?
We recorded conditions potentially related to the development of reflux esophagitis including obesity (determined by body mass index [BMI]), history of GERD symptoms, gastroparesis, diabetes, and use of tobacco and alcohol. We also recorded other potentially pertinent data including a history of malignancy, immunosuppression, chest irradiation or treatment with a nasogastric tube. We recorded any history of cardiopulmonary diseases including coronary artery disease, congestive heart failure, peripheral vascular disease, obstructive sleep apnea and chronic obstructive pulmonary disease. We determined the hospitalization status of each study subject at the time of the diagnosis of LA-A or LA-D reflux esophagitis (outpatient, inpatient, or in the intensive care unit [ICU]). Finally, we reviewed pharmacy records to identify medications that might contribute to esophagitis, and we recorded the use of acid suppressive medications including proton pump inhibitors (PPIs) and histamine H2-receptor antagonists. Outpatients were considered to be using an acid-suppressive medication if the pharmacy record listed it as ‘active’ within the thirty days prior to endoscopy, whereas inpatients were considered to be using an acid-suppressive medication if the pharmacy record listed it as ‘active’ within the thirty days prior to hospital admission.
What is gastroesophageal reflux disease?
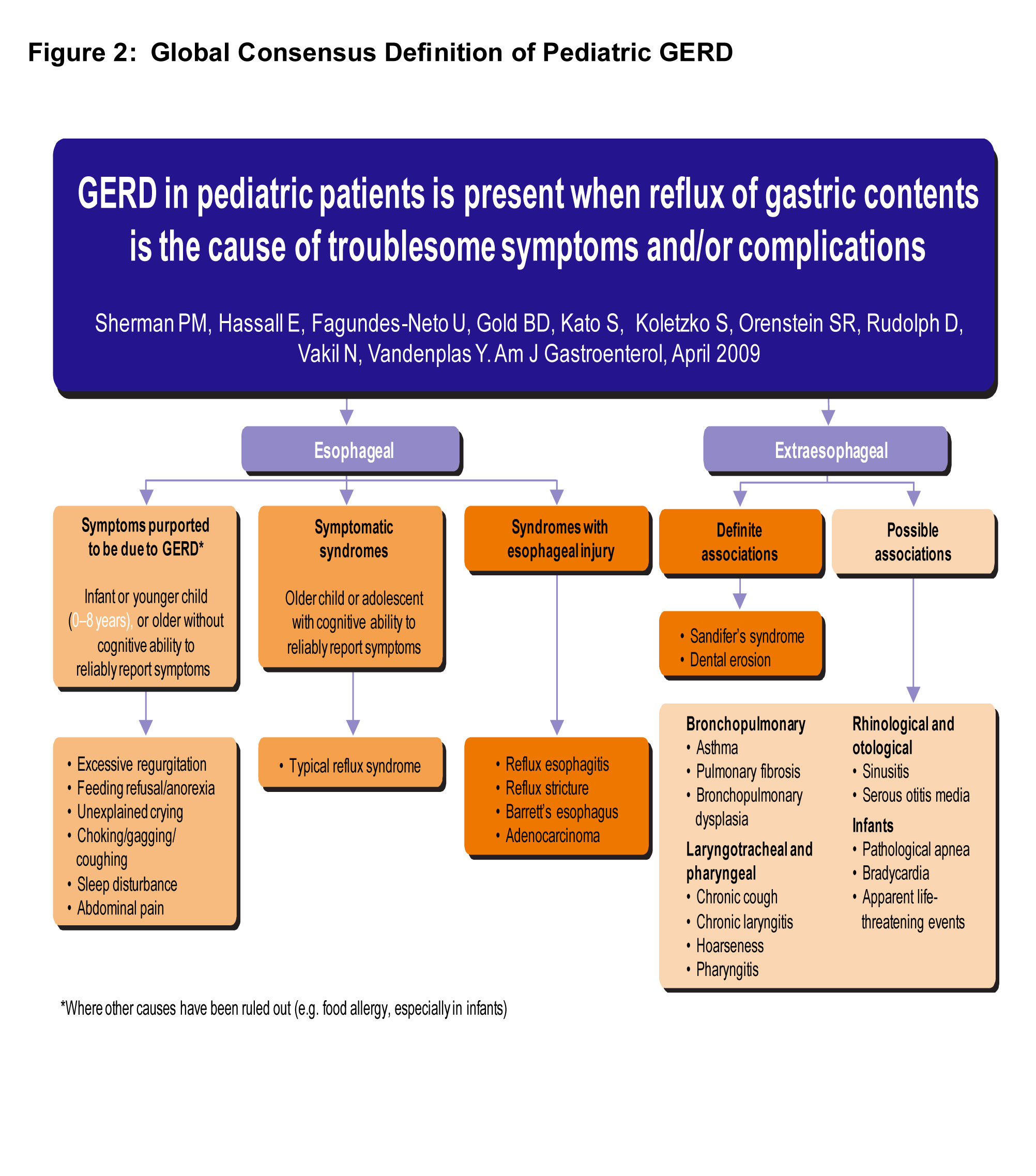
Gastroesophageal reflux disease (GERD) is an extremely common condition that affects up to 20% of the American adult population.1,2Al though GERD is primarily a clinical diagnosis, endoscopy is used to look for GERD complications such as Barrett’s esophagus, to rule out other upper gastrointestinal diseases in equivocal cases, and to determine if GERD has caused esophageal mucosal injury, i.e. reflux esophagitis. Only approximately 30% of patients with typical GERD symptoms have endoscopic evidence of erosive reflux esophagitis, a finding that has important diagnostic and therapeutic implications.3
What are the indications for endoscopy in LA-D?
The indications for endoscopy also differed between patients with LA-D and LA-A esophagitis (Table 3). Gastrointestinal bleeding was the most common indication for endoscopy in patients found to have LA-D esophagitis; it was the indication in 42% of LA-D patients, all of whom were hospitalized at the time of endoscopy. In contrast, only 2% of patients with LA-A esophagitis had endoscopy for evaluation of GI bleeding (p<.0001). GERD was the indication for endoscopy in only 7% of LA-D patients, while it was the most common indication for endoscopy in patients with LA-A esophagitis (30%, p<.0001). Other endoscopic indications such as dysphagia, abdominal pain, and iron deficiency anemia were similar between groups. Thirty-six of our 100 LA-D patients had prior endoscopies; these showed evidence of reflux esophagitis in 20 of the 36 cases (56%) and no erosive esophagitis in 16 cases (44%). Among the 20 LA-D patients with esophagitis found on prior endoscopy, that endoscopy was performed during a hospitalization in 12 cases.
What is the size of the mucosal break in the distal esophagus?
Endoscopic photo of the distal esophagus showing LA-A esophagitis. Note the small mucosal break (<5 mm in length, not extending between the tops of two mucosal folds) in the 10 o’clock position just proximal to the squamo-columnar junction.
What is LA grade?
Presently, the Los Angeles (LA) classification is the endoscopic scoring system most commonly used to grade the severity of reflux esophagitis.4The LA system divides reflux esophagitis into four categories (A-D) based on the extent of esophageal mucosal breaks. LA grade A (LA-A) esophagitis is defined as one or more mucosal breaks not longer than 5 mm, and not extending between the tops of two mucosal folds (Figure 1). In contrast, LA-D esophagitis is defined as one or more mucosal breaks involving 75% or more of the esophageal circumference (Figure 2). LA-D is the most infrequently encountered grade of reflux esophagitis.5
What is LA grade of reflux?
The Los Angeles (LA) grade of reflux esophagitis (A to D) is assumed to reflect severity of the underlying GERD. Thus, LA-D esophagitis patients might be expected to have the most conditions predisposing to GERD (e.g. obesity, hiatal hernia), and the highest frequency of GERD symptoms.
Where is the Department of Gastroenterology and Hepatology located?
4Department of Medicine, Division of Gastroenterology and Hepatology, Dallas VA Medical Center, Dallas, Texas
Popular Posts:
- 1. icd 10 code for paraspinal irritation
- 2. icd 9 code for migraines
- 3. icd-9 code for dvt
- 4. icd 9 code for brain damage
- 5. what is the icd-10 code for lab work
- 6. icd 10 cm code for hairdresser
- 7. 2016 icd 10 code for periureteritis
- 8. icd 9 code for psa
- 9. icd-10 code for osa
- 10. icd 9 code for v56.2