Full Answer
Why is ICD-10 needed for your medical facility?
Why ICD-10 codes are important
- The ICD-10 code system offers accurate and up-to-date procedure codes to improve health care cost and ensure fair reimbursement policies. ...
- ICD-10-CM has been adopted internationally to facilitate implementation of quality health care as well as its comparison on a global scale.
- Compared to the previous version (i.e. ...
What are the common ICD 10 codes?
ICD-10-CM CODES (commonly used) These commonly used ICD-10 diagnosis codes are intended to assist physicians and other authorized ordering parties in providing correct ICD-10 codes as required by Medicare and other insurers. The codes are based on ICD-10-CM 2018, Medicare Regulations and Manuals authorized by the Centers for
What does ICD - 10 stand for?
The International Classification of Diseases, Tenth Edition (ICD-10), is a clinical cataloging system that went into effect for the U.S. healthcare industry on Oct. 1, 2015, after a series of lengthy delays.
Can you ever use an unspecified ICD-10 code?
In both ICD-9 and ICD-10, signs/symptoms and unspecified codes are acceptable and may even be necessary. In some cases, there may not be enough information to describe the patient's condition or no other code is available to use. Although you should report specific diagnosis codes when they are supported by the available documentation and clinical knowledge of the patient's health condition, in some cases, signs/symptoms or unspecified codes are the best choice to accurately reflect the ...
Do ICD-10 codes demonstrate medical necessity in claims?
ICD-10-CM codes should support medical necessity for any services reported. Diagnosis codes identify the medical necessity of services provided by describing the circumstances of the patient's condition.
What is diagnosis code Z71 89?
Other specified counselingICD-10 code Z71. 89 for Other specified counseling is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is the ICD 10 code for paperwork completion?
ICD-10-CM Code for Encounter for other administrative examinations Z02. 89.
What is the ICD 10 code for medical clearance for work?
ICD-10 Code for Encounter for issue of other medical certificate- Z02. 79- Codify by AAPC.
What is diagnosis code Z51 81?
ICD-10 code Z51. 81 for Encounter for therapeutic drug level monitoring is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
Can Z76 89 be used as a primary diagnosis?
The patient's primary diagnostic code is the most important. Assuming the patient's primary diagnostic code is Z76. 89, look in the list below to see which MDC's "Assignment of Diagnosis Codes" is first. That is the MDC that the patient will be grouped into.
What type of code is assigned when the provider documents a reason for a patient seeking healthcare that is not an injury or disease?
10 Cards in this SetWhat is the meaning of “provider” in the ICD-9-CM guidelines?the physicianWhat type of code is assigned when the provider documents a reason for a patient seeking health care that is not an injury or disease?V code (V01.0-V91.99)8 more rows
What is the ICD 10 code for annual physical exam?
Z00.00ICD-10 Code for Encounter for general adult medical examination without abnormal findings- Z00. 00- Codify by AAPC.
What does CPT code 99080 mean?
"Code 99080 is intended to be used when a physician fills out something other than a standard reporting form, such as paperwork related to the Family and Medical Leave Act. This code does not apply to the completion of routine forms, such as hospital-discharge summaries.
What is the ICD-10 code for pre op clearance?
A preoperative examination to clear the patient for surgery is part of the global surgical package, and should not be reported separately. You should report the appropriate ICD-10 code for preoperative clearance (i.e., Z01. 810 – Z01.
What is the ICD-10 code for ASHD?
10 for Atherosclerotic heart disease of native coronary artery without angina pectoris is a medical classification as listed by WHO under the range - Diseases of the circulatory system .
What is the ICD-10 code for pre employment screening?
Z02.1ICD-10 Code for Encounter for pre-employment examination- Z02. 1- Codify by AAPC.
Is Z03 89 a billable code?
Z03. 89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What does encounter for screening for other disorder mean?
Encounter for screening for other diseases and disorders Screening is the testing for disease or disease precursors in asymptomatic individuals so that early detection and treatment can be provided for those who test positive for the disease.
What is the ICD-10 code for nasal congestion?
ICD-10 code R09. 81 for Nasal congestion is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
What does CPT code 99401 mean?
Preventative medicine counselingCPT 99401: Preventative medicine counseling and/or risk factor reduction intervention(s) provided to an individual, up to 15 minutes may be used to counsel commercial members regarding the benefits of receiving the COVID-19 vaccine.
What is medical necessity?
(That’s right; medical necessity isn’t just for that pesky therapy cap .) “For a service to be considered medically necessary, it must be reasonable and necessary to diagnosis or treat a patient’s medical condition ,” explains this Physicians Practice article.
How long will it take for the US to switch to ICD-10?
In a little under two months, the entire US healthcare system will transition to ICD-10—and trust us,...
Why do doctors perform non stress tests?
The physician performs a nonstress test to check on the baby’s condition. If the coder reports a diagnosis code for just an office visit, the payer will likely deny the bill for the nonstress test for lack of medical necessity.”. Okay, you get it: coding for medical necessity has to happen when it comes to ICD-10.
Do not copy codes supplied in patient referral?
For that reason, do not copy the codes supplied in the patient referral. Use the physician diagnosis to inform you on the patient’s situation, sure; but then use your own clinical judgment and skills as a medical professional to diagnose the patient based on what you’re actually going to treat.
Can ICD-9 codes be used with CPT codes?
Furthermore, avoid the “cheat sheet” strategy. As most providers know, certain CPT codes are only payable when used in conjunction with certain ICD-9 codes. Thus, you may be tempted to quickly crosswalk those ICD-9 codes and tack up a new cheat sheet. Don’t. The rules aren’t the same, and crosswalks typically yield unspecified ICD-10 equivalents. As this ICD-10 for PT article explains, “…one of the main battle cries of the new code set is increased specificity, and the transition to ICD-10 represents a giant step away from the use of unspecified codes (unless one of those codes truly represents the most accurate description of a patient’s condition). Thus, if you submit an unspecified code when a more specific code is, in fact, available, you could put yourself at risk for claim denial.”
Can ICD-10 codes be used to justify a denial?
If you simply use whatever ICD-10 codes came from the referring physician, you likely won’t be using the codes most applicable to the services you performed. As a result, you may suffer a denial.
What is the ICd 10 code for diabetes mellitus?
There are five category codes for diabetes mellitus in ICD-10-CM. Diabetes due to underlying conditions, category E08, requires clear documentation of the underlying condition as follows. This includes hyperosmolarity, ketoacidosis, kidney complications, ophthalmic complications, neurological complications, circulatory complications, other specified complications, and unspecified complications and w/o complications.
What is the goal of medical necessity denial?
Ultimately, the goal is to prevent medical necessity denials before they occur, rather than chasing them down after claims rejections or denials. Consider the following eight steps to mitigate medical necessity denials in physician practices and medical groups.
What are the specific concerns of cardiology?
Specific concerns for cardiology include incorrect documentation for certain common conditions. To ensure accurate assignment of codes, documentation must support the specificity of each code category.
What is ischemic cardiomyopathy?
Ischemic cardiomyopathy: The diagnosis of ischemic cardiomyopathy must also state the type (dilated/congestive, obstructive or nonobstructive, hypertrophic), location (endocarditis, right ventricle), and the cause (congenital or alcohol).
When will the ICD-10 grace period end?
Second, the ICD-10 grace period for physician practices comes to a close as of Oct. 1, 2016. And finally, almost 6,000 new ICD-10 codes will be added that same day as the partial code freeze concludes. These factors will impact all providers, but they will be especially notable within physician practices and medical groups.
Is medical necessity greater in ICD-10?
Going forward, physician practices must devote ample time and resources to combat medical necessity denials. While it’s true that the potential for medical necessity denials is greater in ICD-10, consistent implementation of solid processes for denial mitigation across your physician practice or medical group is a smart strategy.
When will the ICd 10-CM Z02.89 be released?
The 2022 edition of ICD-10-CM Z02.89 became effective on October 1, 2021.
What is an encounter for medical or nursing care?
Applicable To. Encounter for medical or nursing care or supervision of healthy infant under circumstances such as adverse socioeconomic conditions at home. Encounter for medical or nursing care or supervision of healthy infant under circumstances such as awaiting foster or adoptive placement.
Pre-authorization
You’ve probably dealt with pre-authorization in your own life, with your own family. It’s usually fairly easy to contact the insurer by phone, explain the procedure and the date, and receive pre-authorization for treatment.
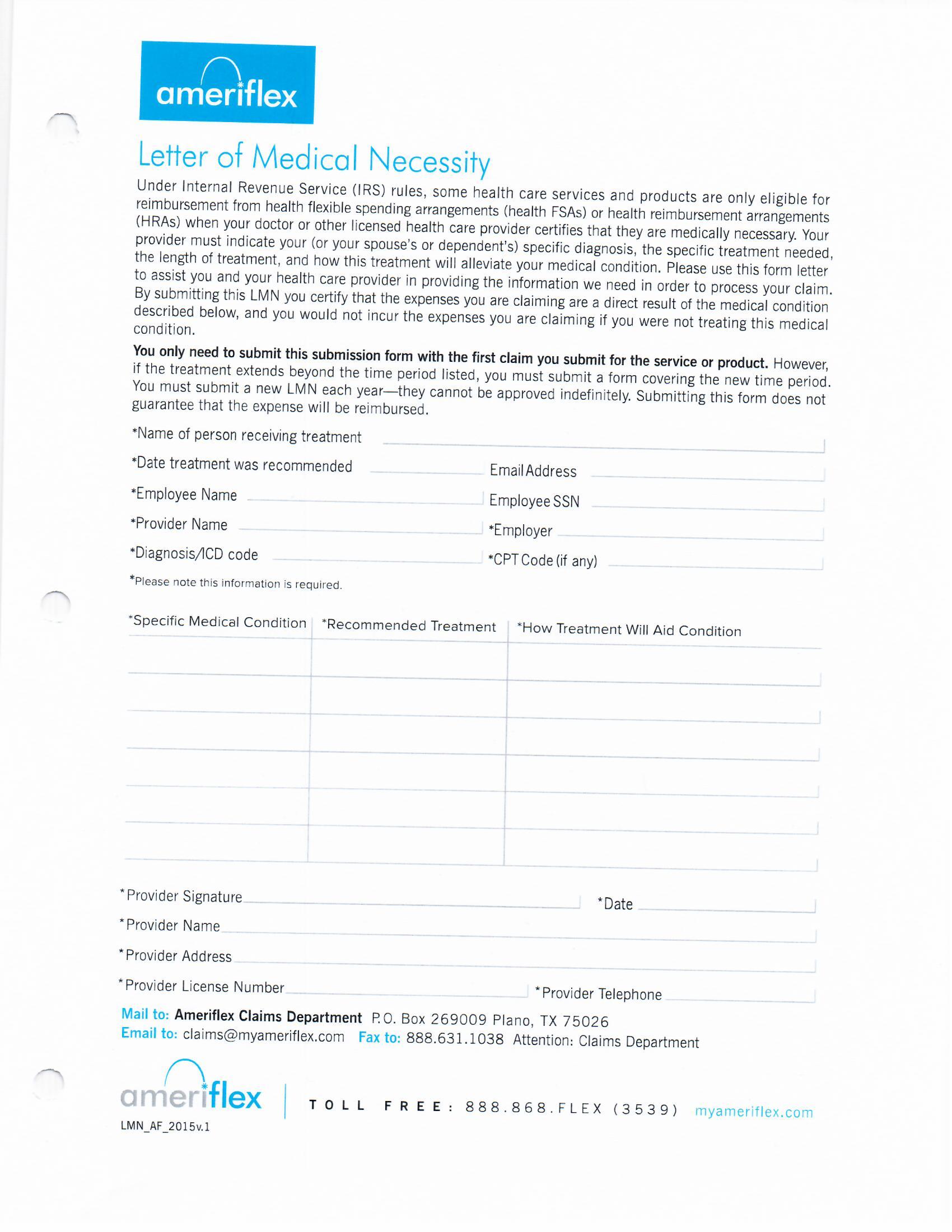
The Letter of Medical Necessity
In the Letter of Medical Necessity (LMN) you have a chance to outline your case for surgery. You must use ICD-10 codes properly in this letter, or the insurer won’t accept your reasoning and will not pay for the surgery. In general, you should limit yourself to 4 diagnostic codes in the letter.
Filling Out a Claim Form: Tricks of the Trade
When you reach the Medical Claim form, there’s a right way and a wrong way to fill it out, and it’s not covered in the form’s instructions. Insurers pay claims for procedures at a given surgical site in the order they’re listed on the form.
An Art, A Science, and A Learnable Skill
Finally, remember that Medical Billing is a both an art and science. Forms need to be filled out correctly, and you have to carefully follow each insurer’s rules and processes. On the other hand, within those rules, you need to learn how to paint a compelling picture of medical necessity.
What is medical necessity?
Medicare defines “medical necessity” as services or items reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member.
How to support medical necessity for services reported?
To better support medical necessity for services reported, you should apply the following principles: 1. List the principal diagnosis, condition, problem, or other reason for the medical service or procedure. 2.
What happens if a provider knows that a claim is not medically necessary?
If a pattern of such claims can be established, and the provider knows or should know that the services reported were not medically necessary, the provider may face monetary penalties, exclusion from Medicare program, and criminal prosecution.
Is coverage limited for medical services?
For all payors and insurance plans, even if a service is reasonable and necessary, coverage may be limited if the service is provided more frequently than allowed under a national coverage policy, a local medical policy, or a clinically accepted standard of practice.
Can a rule out statement be used for outpatient?
For office and/or outpatient services, never use a “rule-out” statement (a suspected but not confirmed diagnosis); a clerical error could permanently tag a patient with a condition that does not exist. Code symptoms, if no definitive diagnosis is yet determined, instead of using rule-out statements. 4.
Can you be denied if you are not medically necessary?
Claims for services deemed to be not medically necessary will be denied. Further, if Medicare (or any other payer) pay for services that they later determine to be not medically necessary, they may demand that those payments be refunded (with interest).
What are the requirements for medical services?
Services must be under accepted standards of medical practice and considered to be specific and effective treatment for the patient’s condition. The amount, frequency, and duration of the services planned and provided must be reasonable. Services must be necessary for treatment of the patient’s condition: The medical record must clearly describe the patient’s condition before, during, and after the therapy episode to support that the patient significantly benefited from ongoing therapy services and that the progress was sustainable and of practical value when measured against the patient’s condition at the start of treatment. Documentation of comparable objective/functional measures plays a key role in demonstrating medical necessity.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Popular Posts:
- 1. icd 10 code for right lower leg wound
- 2. icd 10 code for rash groin
- 3. what is the icd 10 cm code for vesicoureteral reflux with nephropathy of the right kidney
- 4. icd 10 code for fungal tonails
- 5. icd 10 code for history of kawasaki disease
- 6. icd 10 code for medication reaction
- 7. icd 10 cm code for siadh
- 8. icd 10 code for artherosclerotic calcifications of abdominal aorta
- 9. icd 10 code for personal history of suicide attempt
- 10. icd 10 code for urinary incontinence male