What is the ICD 10 version of myelodysplastic syndrome?
Myelodysplastic syndrome, unspecified. This is the American ICD-10-CM version of D46.9 - other international versions of ICD-10 D46.9 may differ.
What is the ICD 10 code for neoplasm?
This is the American ICD-10-CM version of D46.9 - other international versions of ICD-10 D46.9 may differ. All neoplasms are classified in this chapter, whether they are functionally active or not.
What is the ICD 10 code for lactic acidosis?
This is the American ICD-10-CM version of E88.41 - other international versions of ICD-10 E88.41 may differ. Applicable To. Mitochondrial myopathy, encephalopathy, lactic acidosis and stroke-like episodes. The following code (s) above E88.41 contain annotation back-references. Annotation Back-References.
What is a diagnosis of MELAS?
Diagnosis. Diagnosis of MELAS usually begins with a physical exam and a review of the patient's medical history and symptoms. The only way to positively diagnose MELAS is through genetic testing. Clinical tests to help diagnose the condition may include imaging, muscle biopsies, or measuring lactic acid in the muscles.
What causes Melas syndrome?
Causes. MELAS is caused by mutations in mitochondrial DNA (mtDNA). Mutations affecting the genes for mtDNA are inherited from the mother. MtDNA that is found in sperm cells is typically lost during fertilization and as a result, all human mtDNA comes from the mother.
How is Melas syndrome inherited?
The genes associated with MELAS are located in mitochondrial DNA and therefore follow a maternal inheritance pattern (also called mitochondrial inheritance). MELAS can be inherited from the mother only, because only females pass mitochondrial DNA to their children.
What does Melas syndrome do to the mitochondria?
Mutations in a particular transfer RNA gene, MT-TL1, cause more than 80 percent of all cases of MELAS. These mutations impair the ability of mitochondria to make proteins, use oxygen, and produce energy.
Is Melas syndrome fatal?
Although the syndrome was initially described as relentlessly progressive and usually fatal in early life, patients carrying this mutation may have lesser symptoms and a normal life span [9]. Regular assessment for other organ involvement, such as for cardiomyopathy, proteinuria or myopathy, is recommended.
How long do you live with MELAS?
MELAS typically presents during childhood, although symptoms can appear as early as before age 2 or as late as after age 40. Over time, it results in neurological impairment and is often fatal. Most individuals survive ~17 years following the onset of seizures or other problems of the nervous system.
How many people have Melas syndrome?
MELAS is one of the most common mitochondrial diseases, with an estimated incidence of 1 in 4000. Both genders are equally affected, but only women can pass the condition on as mitochondria are carried in the tails of sperm cells and therefore shed outside the zygote during fertilization.
How many people affect MELAS?
According to the USDA, more than 38 million people, including 12 million children, in the United States are food insecure.
What causes lactic acidosis?
Lactic acidosis occurs when lactic acid production exceeds lactic acid clearance. The increase in lactate production is usually caused by impaired tissue oxygenation, either from decreased oxygen delivery or a defect in mitochondrial oxygen utilization.
What is the life expectancy for mitochondrial disease?
A small study in children with mitochondrial disease examined the patient records of 221 children with mitochondrial disease. Of these, 14% died three to nine years after diagnosis. Five patients lived less than three years, and three patients lived longer than nine years.
How many people affect MELAS?
According to the USDA, more than 38 million people, including 12 million children, in the United States are food insecure.
Why is lactic acidosis a common symptom in mitochondrial diseases?
The most recognized laboratory abnormality in patients with mitochondrial disorders is lactic acidosis. Dysfunction in the electron transport chain causes decreased production of adenosine triphosphate. Low adenosine triphosphate levels result in an up-regulation of glycolysis, leading to an overproduction of pyruvate.
Tabular List of Diseases and Injuries
The Tabular List of Diseases and Injuries is a list of ICD-10 codes, organized "head to toe" into chapters and sections with coding notes and guidance for inclusions, exclusions, descriptions and more. The following references are applicable to the code E88.41:
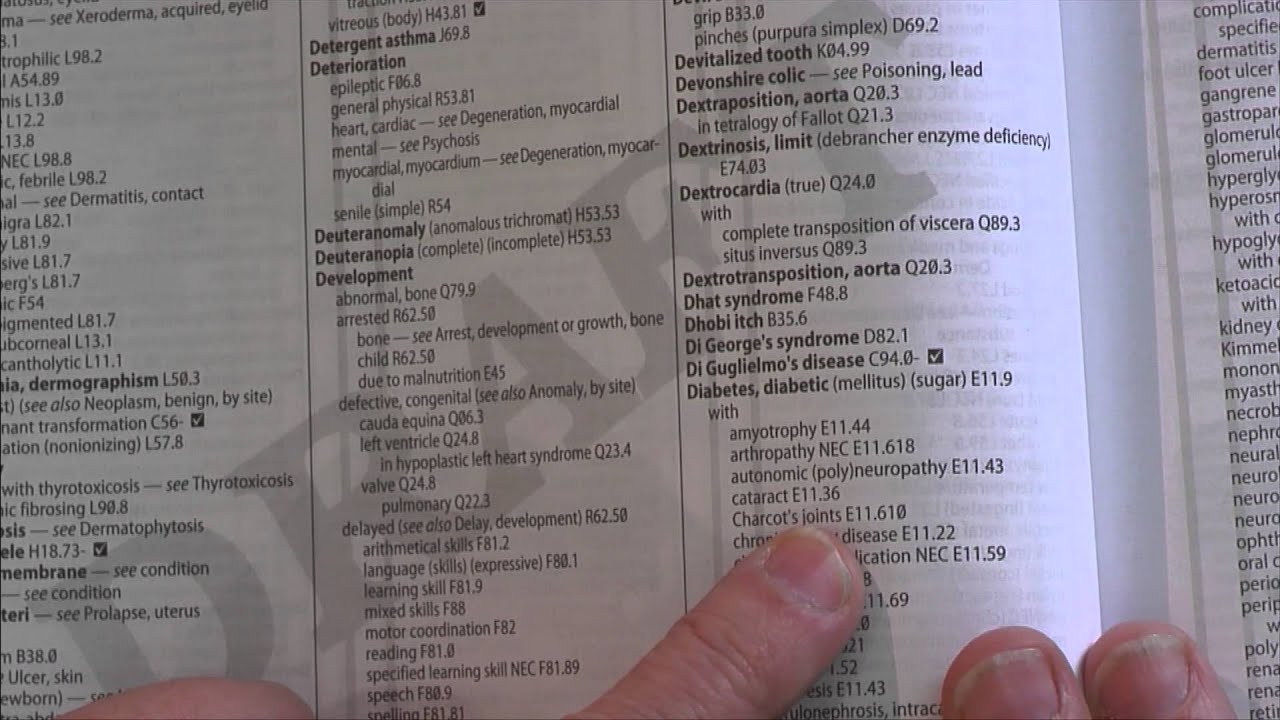
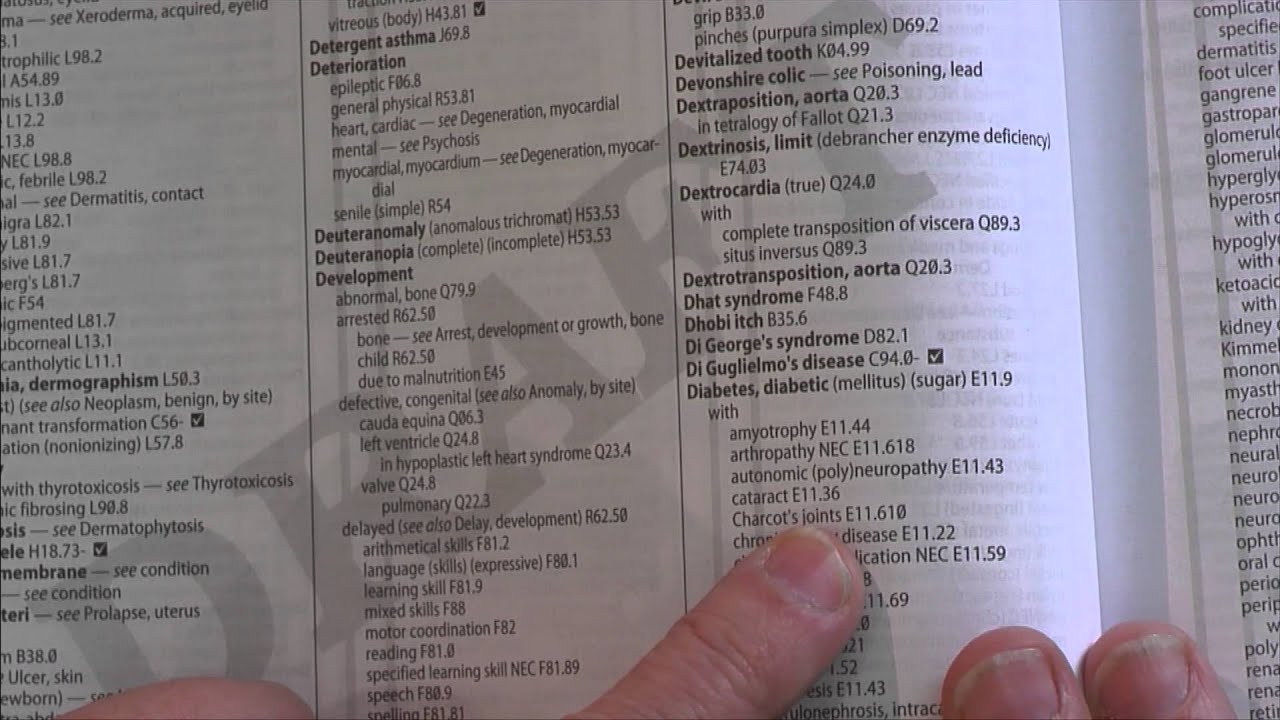
Index to Diseases and Injuries
The Index to Diseases and Injuries is an alphabetical listing of medical terms, with each term mapped to one or more ICD-10 code (s). The following references for the code E88.41 are found in the index:
Approximate Synonyms
The following clinical terms are approximate synonyms or lay terms that might be used to identify the correct diagnosis code:
Clinical Information
MELAS SYNDROME-. a mitochondrial disorder characterized by focal or generalized seizures episodes of transient or persistent neurologic dysfunction resembling strokes and ragged red fibers on muscle biopsy.
Convert E88.41 to ICD-9 Code
The General Equivalency Mapping (GEM) crosswalk indicates an approximate mapping between the ICD-10 code E88.41 its ICD-9 equivalent. The approximate mapping means there is not an exact match between the ICD-10 code and the ICD-9 code and the mapped code is not a precise representation of the original code.
Information for Patients
Metabolism is the process your body uses to get or make energy from the food you eat. Food is made up of proteins, carbohydrates, and fats. Chemicals in your digestive system break the food parts down into sugars and acids, your body's fuel.
What is myelodysplastic syndrome?
Myelodysplastic syndrome (clinical) Clinical Information. (mye-eh-lo-dis-plas-tik sin-drome) disease in which the bone marrow does not function normally. A clonal hematopoietic disorder characterized by dysplasia and ineffective hematopoiesis in one or more of the hematopoietic cell lines.
What is the code for a primary malignant neoplasm?
A primary malignant neoplasm that overlaps two or more contiguous (next to each other) sites should be classified to the subcategory/code .8 ('overlapping lesion'), unless the combination is specifically indexed elsewhere.
What chapter is neoplasms classified in?
All neoplasms are classified in this chapter, whether they are functionally active or not. An additional code from Chapter 4 may be used, to identify functional activity associated with any neoplasm. Morphology [Histology] Chapter 2 classifies neoplasms primarily by site (topography), with broad groupings for behavior, malignant, in situ, benign, ...
Attention
Only comments seeking to improve the quality and accuracy of information on the Orphanet website are accepted. For all other comments, please send your remarks via contact us. Only comments written in English can be processed.
Epidemiology
Precise prevalence and incidence data are not available. Estimated prevalence has been reported about 0.2/100,000 in Japan. It is one of the most frequent mitochondrial disorders, which are estimated to affect 1/10,000 people. Males and females are affected equally.
Clinical description
MELAS is a multi-organ disease with protean manifestations. MELAS symptoms usually occur before 20 years, but can develop at any age. The hallmark feature is stroke-like episodes causing vomiting, headache, or epilepsy followed by loss of consciousness, frequently hemiparesis, hemianopia, and cortical blindness.
Etiology
The exact pathogenesis has not been fully elucidated. Energy depletion due to mitochondrial dysfunction underlies the clinical manifestations. Among mutations in 19 mitochondrial genes so far identified , the 3243G>A mutation in the mitochondrial tRNA Leu (UUR) gene ( MT-TL1) is most frequent (approximately 80%).
Diagnostic methods
Diagnosis of MELAS is made based on a combination of the characteristic clinical features, laboratory findings indicative of mitochondrial dysfunction, and genetic testing.
Differential diagnosis
Various diseases causing juvenile-onset acute ischemic stroke need to be distinguished. In patients with migraine, epilepsy, or encephalitis MELAS should be ruled out. Further differential diagnoses are other mitochondrial disorders that share clinical manifestations with MELAS.
Antenatal diagnosis
Prenatal diagnosis, though possible, is difficult due to heterogeneity in the proportion of mutations between tissues.
Popular Posts:
- 1. icd 10 code for elbow olecranon soft tissue swelling
- 2. icd 10 code for right knee prosthesis instability
- 3. icd 10 dx code for staphylococcuus gn
- 4. what is the icd 10 code for basal cell carcinoma of eyelid
- 5. icd 10 code for brvo right eye
- 6. icd 10 code for right hip synovitis
- 7. icd 10 code for pain related neoplasm
- 8. icd-10 code for nicotine dependence vaping
- 9. icd-10 code for prenancy
- 10. icd 10 code for trauma lower extremity