DSM-5 Diagnoses and ICD-9-CM and ICD-10-CM Codes, Numerical ICD-10-CM Listing
| ICD-9-CM | ICD-10-CM | Disorder, condition, or problem |
| 278.00 | E66.9 | Overweight or obesity |
| 290.40 | F01.50 | Major vascular neurocognitive disorder, ... |
| 290.40 | F01.51 | Major vascular neurocognitive disorder, ... |
| [331.19 +] 294.10 | [G31.09 +] F02.80 | [Frontotemporal disease +] Major frontot ... |
What are the DSM 5 codes?
DSM-5 Recommended ICD-10-CM Code for use beginning October 1, 2020; Alcohol withdrawal, ...
What are the DSM 5 disorders?
DSM-5 online. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition ( DSM-5 ), is the 2013 update to the Diagnostic and Statistical Manual of Mental Disorders, the taxonomic and diagnostic tool published by the American Psychiatric Association (APA). In the United States, the DSM serves as the principal authority for ...
What is mild cognitive disorder?
Mild cognitive impairment (MCI) is the stage between the expected cognitive decline of normal aging and the more serious decline of dementia. It's characterized by problems with memory, language, thinking or judgment.
What is the DSM 5 diagnosis for substance abuse?
The DSM-5 includes guidelines for clinicians to determine how severe a substance use disorder is depending on the number of symptoms. Two or three symptoms indicate a mild substance use disorder; four or five symptoms indicate a moderate substance use disorder, and six or more symptoms indicate a severe substance use disorder.
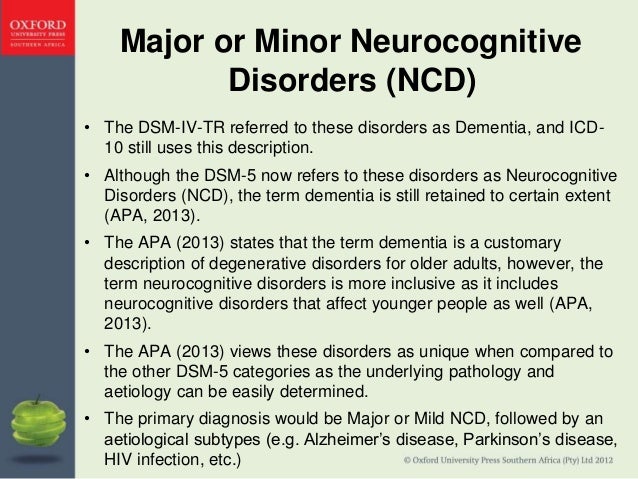
Is mild neurocognitive disorder in the DSM-5?
As noted earlier, DSM-5 has now classified acquired neurocognitive disorders of all age groups under three major headings: delirium, major NCD, and mild NCD.
What is the ICD-10 code for neurocognitive disorder?
ICD-10 code R41.
What is mild neurocognitive disorder?
Mild neurocognitive disorder goes beyond normal issues of aging. It describes a level of cognitive de- cline that requires compensatory strategies and accommodations to help maintain independence and perform activities of daily living.
How do you code a mild cognitive impairment?
ICD-10 Code for Mild cognitive impairment, so stated- G31. 84- Codify by AAPC.
Which of the following is the ICD 10 code for possible major neurocognitive disorder due to Alzheimer's disease?
Major Neurocognitive Disorder Due to Possible Alzheimer's Disease (Note: Code first 331.0 (G30. 9) Alzheimer's disease.) Major Neurocognitive Disorder Due to Possible Frontotemporal Lobar Degeneration (Note: Code first 331.19 (G31. 09) frontotemporal disease.)
What are the different types of neurocognitive disorders?
Alzheimer disease (also called senile dementia, Alzheimer type)Creutzfeldt-Jakob disease.Diffuse Lewy body disease.Huntington disease.Multiple sclerosis.Normal pressure hydrocephalus.Parkinson disease.Pick disease.
Is mild neurocognitive disorder the same as MCI?
Mild Neurocognitive Disorder (also known as Mild Cognitive Impairment, or MCI) is a condition in which individuals demonstrate cognitive impairment with minimal impairment of instrumental activities of daily living (IADLs).
What is an example of mild neurocognitive disorder?
Major and mild neurocognitive disorders can occur with Alzheimer's disease, degeneration of the brain's frontotemporal lobe, Lewy body disease, vascular disease, traumatic brain injury, HIV infection, prion diseases, Parkinson's disease, Huntington's disease, or another medical condition, or they can be caused by a ...
What are the neurocognitive disorders in the DSM-5?
The Diagnostic Statistical Manual-5 (DSM-5) has included a category named the neurocognitive disorder which was formally known in DSM-IV as 'dementia, delirium, amnestic, and other cognitive disorders'. The DSM-5 distinguishes between 'mild' and 'major' neurocognitive disorders.
What is the difference between dementia and mild cognitive impairment?
Both mild cognitive impairment and mild dementia are characterized by objective evidence of cognitive impairment. The main distinctions between mild cognitive impairment and mild dementia are that in the latter, more than one cognitive domain is involved and substantial interference with daily life is evident.
Is mild neurocognitive disorder a disability?
Neurocognitive disorders (also referred to as organic brain syndrome) can be mild or advanced at the time of application for disability benefits; in advanced cases, another person is needed to help with the disability application—usually a spouse or other family member.
What is the DSM code?
List of codes. The Diagnostic and Statistical Manual of Mental Disorders (DSM) is the official reference manual used to accurately diagnose mental health conditions. Our mental health affects every aspect of our lives, from our personal thoughts and feelings to our relationships, work life, and overall well-being.
When was the DSM 5 released?
In 2013, the American Psychiatric Association (APA) released the newest version of the DSM — the DSM-5. This involved the teamwork and input of more than 160 top researchers and clinicians from around the world, and it’s the product of over 10 years of work.
What is the DSM for mental health?
When a mental health symptom arises, getting the proper diagnosis is a vital step in the treatment process. This is where the DSM can help. It’s the go-to diagnostic manual for healthcare professionals in the United States. Clinicians often refer to these guidelines to help them make a correct diagnosis, and they use the accompanying codes ...
Why is it important to update the DSM-5?
Updates are essential, as mental health research frequently delivers new insights. In addition, each new version of the DSM can address and change any outdated information. As new scientific evidence emerges, updates to the DSM-5 can be posted online.
How many digits are in the ICD-10 code?
The newest version of the code — ICD-10, which was released on October 1, 2015 — contains more digits (3 to 7 digits) than the previous version (3 to 5 digits).
What is a major neurocognitive disorder?
Major or Mild Neurocognitive Disorder due to AD (Alzheimer’s Disease) also commonly referred to as Alzheimer's Dementia, is a DSM-5 ( Diagnostic and Statistical Manual of Mental Disorders, fifth edition), diagnosis assigned to individuals who are experiencing cognitive deficits directly related to the onset and progression of Alzheimer's Dementia.
What are the DSM 5 criteria for Alzheimer's?
There are diagnostic rule-outs for Alzheimer's Disease which the clinician must consider, In the DSM -5, disorders such as Major Depressive Disorder, and other medical conditions which impact cognitive clarity, such as thyroid dysfunction (American Psychiatric Association, 2013). Other differential diagnostic considerations according to the DSM-5 and other sources are: CBD (Cortical Basal Degeneration), CJD (Creutzfeldt-Jakob Disease), DLB, (Dementia with Lewy Bodies), FTD (Frontotemporal Dementia) MND, (Motor Neuron Disease), and PSP (Progressive Supranuclear Palsy) (American Psychiatric Association, 2013; Alzheimer's Association 2014a). Korsakoff's syndrome should be ruled out based on history of alcohol use. Poly-pharmacy, or more limited use of certain prescribed or illicit mediation or alcohol that can produce cognitive deficits, such as benzodiazepines can account for MCI ( The Regents of the University of California, 2014). Isolation, loneliness, and sensory deficits can all produce effects which may resemble early stage dementia.
What are the symptoms of Alzheimer's?
According to the DSM-5, there are three Criterion for Alzheimer's Disease: A. The diagnostic criteria for major or minor neurocognitive disorder is fulfilled, B. Insidious onset and gradual decline of cognitive function in one or more areas for mild neurocognitive disorder, or two or more areas for major ...
What are the three indicators of cognitive decline?
The following three indicators are present: 1. Decline in memory or learning, and one other cognitive area, based on history or trials of neuropsychological testing. 2. Steady cognitive decline, without periods of stability, and. 3.
Does DSM-5 treat Alzheimer's?
The DSM-5 does not specify treatment options for Alzheimer's Disease (American Psychiatric Association, 2013). Detection of Cognitive impairment can b detected by a protocol developed by the Alzheimer's association for Medicare annual wellness visits in a primary care setting, for possible early detection of AD (Cordell, et al, 2013) There are a number of cholinesterase inhibitors which are utilized to delay the progression of Alzheimer's Disease. There have also been clinical trials exploring the use of transdermal nicotine to treat MCI (Newhouse, et al, 2012), as it has been established that nicotine binds to nicotinic acetylcholine receptors, and is responsible for facilitating memory storage. There is currently no pharmacological intervention which can halt the progression. The delay of the progression of the disorder can give an individual with Alzheimer's Disease a longer period of cognitive functioning, and an opportunity to settle financial and business matters, to say goodbye to or make amends to family and friends, and to enjoy a fuller quality of life and retain independence as long as possible, as well as delay financial and emotional burdens on family The impact of Alzheimer's Disease on family members and caregivers is substantial, with financial and emotional considerations predominating. Family therapy may be useful, particularly if there has been a history of family strife, and supportive, solution focused counseling and psychoeducation may be useful for the person with Alzheimer's Disease as well as their family and caregivers, to learn how to best support the patient.
Is sleep disruption an early warning sign of Alzheimer's?
Disrupted sleep may be an early warning indicator of Alzheimer's Disease. Poorly maintained sleep, with daytime fatigue and the need for hypnotics is correlated with the onset of Alzheimer's Disease within two years according to a study involving n=14,600 age 50 and up.
Does nicotine help with memory?
There have also been clinical trials exploring the use of transdermal nicotine to treat MCI (Newhouse, et al, 2012), as it has been established that nicotine binds to nicotinic acetylcholine receptors, and is responsible for facilitating memory storage .
Introduction
Symptoms of Alzheimer's Disease
- According to the DSM-5, there are three Criterion for Alzheimer's Disease: A. The diagnostic criteria for major or minor neurocognitive disorder is fulfilled, B. Insidious onset and gradual decline of cognitive function in one or more areas for mild neurocognitive disorder, or two or more areas for major neurocognitive disorder, and C. The diagnost...
Onset
- The DSM-5 notes that early onset of Alzheimer's Disease can occur in the fifties and sixties, with onset of symptoms in the eighties and nineties (American Psychiatric Association, 2013).
Prevalence
- According to the DSM-5, the prevalence of Alzheimer's Disease is 5-10% in persons in their seventies, and 25% for those age 80 and over (American Psychiatric Association, 2013).
Risk Factors and Risk Markers
- The DSM-5 indicates that risk factors for Alzheimer's Disease are TBI (Traumatic Brain Injury) and old age (American Psychiatric Association, 2013). A correlation has been found between size of living space and incidence of Alzheimer's Disease. In an eight year longitudinal study of n=1300 elderly people with no indicators of dementia, subjects who did not venture outside their immedi…
Comorbidity
- The DSM-5 indicates that APD is comorbid with multiple medical problems (American Psychiatric Association, 2013). The comorbidity of Alzheimer's Disease with Down's Syndrome is 75% in individuals with Down Syndrome over age 65 (Alzheimer's Association, 2014a).
Treatment For Alzheimer's Disease
- The DSM-5 does not specify treatment options for Alzheimer's Disease (American Psychiatric Association, 2013). Detection of Cognitive impairment can b detected by a protocol developed by the Alzheimer's association for Medicare annual wellness visits in a primary care setting, for possible early detection of AD (Cordell, et al, 2013) There are a number of cholinesterase inhibit…
Impact on Functioning
- Alzheimer's Disease will have a progressive major impact on most areas of functioning. It is inexorable and terminal. (American Psychiatric Association, 2013). The degree of impact will depend on what stage the disease process is in: Stage 1: No impairment- no detectable cognitive impairment in an individual with risk factors for Alzheimer's Disease. Stage 2: Very mild decline- …
Differential Diagnosis
- There are diagnostic rule-outs for Alzheimer's Disease which the clinician must consider, In the DSM -5, disorders such as Major Depressive Disorder, and other medical conditions which impact cognitive clarity, such as thyroid dysfunction (American Psychiatric Association, 2013). Other differential diagnostic considerations according to the DSM-5 and other sources are: CBD (Corti…
Help Us Improve This Article
- Did you find an inaccuracy? We work hard to provide accurate and scientifically reliable information. If you have found an error of any kind, please let us know by sending an email to [email protected], please reference the article title and the issue you found.
Popular Posts:
- 1. icd 9 code for polyuria
- 2. icd 10 code for chronic osteomyelitis of jaw
- 3. icd 10 code for primary osteoarthritis involving multiple joints
- 4. icd 10 code for history of diverticulitis of colon
- 5. icd 10 code for preterm labor with delivery third trimester
- 6. icd 10 code for stomatocytosis
- 7. icd 10 code for unspecified psychosis
- 8. icd 10 code for hemorrhagic brain metastases
- 9. icd 10 code for calcifoed lesion of iliac artery
- 10. icd 10 code for type 2 diabetes with neurological manifestation