What is the CPT code for monoclonal antibody?
· Jan 13, 2022 - 12:53 PM. In addition to the seven new 2022 ICD-10 procedure codes announced in November, the Centers for Medicare & Medicaid Services on April 1 will implement two new ICD-10 procedure codes for reporting COVID-19 therapeutics. The new codes are for describing the infusion of tixagevimab and cilgavimab monoclonal antibody (code …
What is the ICD 10 code for monoclonal gammopathy?
· The 2 new ICD-10-PCS codes are: XW023X7 – Introduction of tixagevimab and cilgavimab monoclonal antibody into muscle, percutaneous approach, new technology group 7; XW023Y7 – Introduction of other new technology monoclonal antibody into muscle, percutaneous approach, new technology group 7; Source: U.S. Centers for Medicare & Medicaid Services (CMS)
What is the ICD 10 code for antibody response examination?
ICD 10 codes for monoclonal antibodies and ICD Code Y43.4 Y43.4 - monoclonal antibodies Font : A- A+ Drugs Canakinumab This medication is an interleukin-1 beta-blocker, prescribed for...
When can health care providers administer monoclonal antibody therapies?
· Monoclonal gammopathy. D47.2 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM …
What is a monoclonal antibody for COVID-19?
Monoclonal antibodies are laboratory-produced molecules that act as substitute antibodies that can restore, enhance or mimic the immune system's attack on cells. Monoclonal antibodies for COVID-19 may block the virus that causes COVID-19 from attaching to human cells, making it more difficult for the virus to reproduce and cause harm. Monoclonal antibodies may also neutralize a virus.
Is there a monoclonal antibody therapy for post COVID-19 exposure?
FDA authorizes bamlanivimab and etesevimab monoclonal antibody therapy for post-exposure prophylaxis (prevention) for COVID-19 | FDA.
How many types of monoclonal antibody COVID-19 treatments are there in the US?
In the United States, there are three anti-SARS-CoV-2 monoclonal antibody treatments with FDA Emergency Use Authorization (EUA) for the treatment of COVID-19: bamlanivimab plus etesevimab, casirivimab plus imdevimab,, and sotrovimab.
Should you still get the COVID-19 vaccine if you were treated with monoclonal antibodies?
If you were treated for COVID-19 with monoclonal antibodies or convalescent plasma, there is no need to delay getting a COVID-19 vaccine.
Is there an antibody cocktail for COVID-19?
The treatment, bamlanivimab and etesevimab administered together, was granted FDA emergency use authorization in February. Eli Lilly and the FDA stipulated that the antibody cocktail is authorized as a COVID-19 prophylaxis only for individuals who have been exposed to the virus.
Is it possible to develop immunity to COVID-19 after being exposed?
In addition, the hope is that people who've been exposed to COVID-19 also develop an immunity to it. When you have immunity, your body can recognize and fight off the virus. It's possible that people who've had COVID-19 can get sick again -- and maybe infect other people.
How many types of COVID-19 vaccines are available in the US?
Three COVID-19 vaccines are authorized or approved for use in the United States to prevent COVID-19. Pfizer-BioNTech or Moderna (COVID-19 mRNA vaccines) are preferred. You may get Johnson & Johnson's Janssen COVID-19 vaccine in some situations.
Are there different COVID-19 vaccine boosters?
The FDA has authorized three vaccine boosters — Pfizer-BioNTech, Moderna and Janssen-Johnson & Johnson — and determined that it is safe to get a COVID-19 vaccine booster or additional dose that is a different brand than your initial dose or doses.
What antiviral drugs are available for treatment of COVID-19?
Remdesivir is the only drug that is approved by the Food and Drug Administration (FDA) for the treatment of COVID-19. Ritonavir-boosted nirmatrelvir (Paxlovid), molnupiravir, and certain anti-SARS-CoV-2 monoclonal antibodies (mAbs) have received Emergency Use Authorizations from the FDA for the treatment of COVID-19.
Should you get the Covid vaccine if you have an autoimmune disease?
The American College of Rheumatology COVID-19 Vaccine Clinical Guidance recommends that people with autoimmune and inflammatory rheumatic disease (which includes lupus) get the vaccine unless they have an allergy to an ingredient in the vaccine.
Should I get the COVID-19 vaccine if I had COVID-19?
Yes, you should be vaccinated regardless of whether you already had COVID-19.
What medication is not recommended before vaccinations for COVID-19?
It is not recommended you take over-the-counter medicine – such as ibuprofen, aspirin, or acetaminophen – before vaccination for the purpose of trying to prevent vaccine-related side effects. It is not known how these medications might affect how well the vaccine works.
What is a monoclonal immunoglobulin test?
A laboratory test result indicating the presence of an abnormally high level of monoclonal immunoglobulins in the blood or urine.
What is the code for a primary malignant neoplasm?
A primary malignant neoplasm that overlaps two or more contiguous (next to each other) sites should be classified to the subcategory/code .8 ('overlapping lesion'), unless the combination is specifically indexed elsewhere.
What is the table of neoplasms used for?
The Table of Neoplasms should be used to identify the correct topography code. In a few cases, such as for malignant melanoma and certain neuroendocrine tumors, the morphology (histologic type) is included in the category and codes. Primary malignant neoplasms overlapping site boundaries.
When will the ICd 10 D47.2 be released?
The 2022 edition of ICD-10-CM D47.2 became effective on October 1, 2021.
Is hypogammaglobulinemia co-occurrent?
Hypogammaglobulinemia co-occurrent and due to monoclonal gammopathy of undetermined significance
What is the code for mAb infusion?
CMS developed two procedure codes, M0239 and M0243. When coverage criteria were established by CMS for these codes, no professional component was “split out” to allow both professional and institutions to billed for the same code as other outpatient procedure codes. In the situation described, the physician attending to the patient care should bill the appropriate evaluation and management code and the hospital bills for the mAb infusion.
What modifier is used for E/M?
During the PHE, we would anticipate this circumstance to be a common occurrence, and physicians and non-physician practitioners furnishing these services on the same day should add modifier “25” to the E/M code to identify it as a medically necessary E/M service furnished on the same day that another service is furnished by the same physician or other supplier. Similarly, hospital outpatient departments furnishing separately identifiable office visits on the same day a vaccine or mAb infusion is administered should also add modifier “25” to identify a medically necessary E/M service furnished on the same day as another service.
Can mAB be administered in emergency settings?
mAB may only be administered in settings in which health care providers have immediate access to medications to treat a severe infusion reaction, such as anaphylaxis, and the ability to activate the emergency medical system, as necessary. Reference: Monoclonal Antibody COVID-19 Infusion. 6.
Is DR condition code required?
The DR condition code is not required.
Is mAb on NCCI?
At this time the mAb infusions currently are not on the NCCI edit files and should not impact claims when the patient is receiving other infusions. The NCCI edit files are updated quarterly so be sure to review the current files.
When will the ICd 10-CM Z01.84 be released?
The 2022 edition of ICD-10-CM Z01.84 became effective on October 1, 2021.
What is a Z00-Z99?
Categories Z00-Z99 are provided for occasions when circumstances other than a disease, injury or external cause classifiable to categories A00 -Y89 are recorded as 'diagnoses' or 'problems'. This can arise in two main ways:
COVID-19 VEKLURYTM (remdesivir)
Following the recent statement from the National Institutes of Health (NIH) COVID-19 Treatment Guidelines Panel about therapies for the COVID-19 Omicron variant, CMS created HCPCS code J0248 for VEKLURY™ (remdesivir) antiviral medication when administered in an outpatient setting.
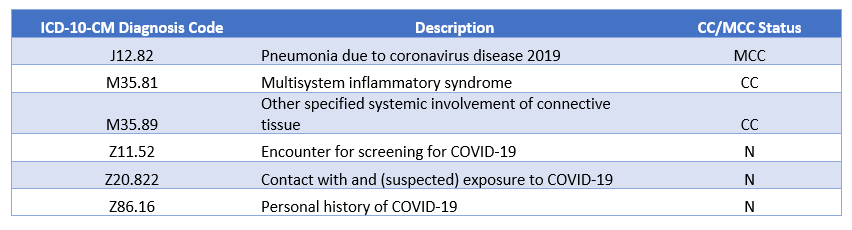
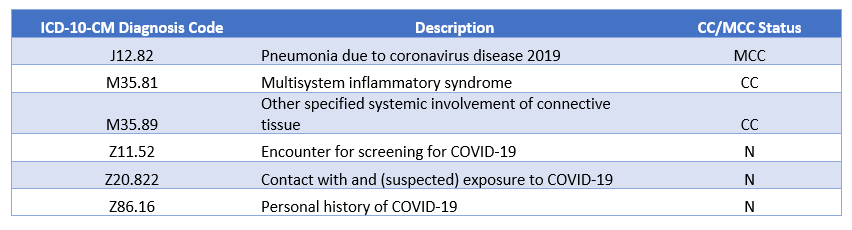
COVID-19 Monoclonal Antibody Products
The FDA authorized the following investigational monoclonal antibody product under EUA for pre-exposure prophylaxis of COVID-19:
Important Update about Viral Variants
On April 16, 2021, the FDA revoked the EUA for bamlanivimab, when administered alone , due to a sustained increase in COVID-19 viral variants in the U.S. that are resistant to the solo product.
Medicare Coverage for COVID-19 Monoclonal Antibody Products
During the COVID-19 public health emergency (PHE), Medicare will cover and pay for these infusions (when furnished consistent with their respective EUAs) the same way it covers and pays for COVID-19 vaccines.
Coding for the Administration of COVID-19 Monoclonal Antibody Products
CMS identified specific code (s) for each COVID-19 monoclonal antibody product and specific administration code (s) for Medicare payment:
Medicare Payment for Administering COVID-19 Monoclonal Antibody Products
To ensure immediate access during the COVID-19 PHE, Medicare covers and pays for these infusions and injections in accordance with Section 3713 of the Coronavirus Aid, Relief, and Economic Security Act (CARES Act) .
Billing for Administering COVID-19 Monoclonal Antibody Products
Health care providers can bill on a single claim for administering COVID-19 monoclonal antibody products, or submit claims on a roster bill.
Medicare reminds healthcare providers of an important coverage change through claims denials
Ever since a public health emergency (PHE) for COVID-19 was declared on Jan. 27, 2020, there has been several new HCPCS Level II codes created for monoclonal antibody (mAb) products and administration.
mAb Product and Administration Codes
Here are the most current codes for investigational monoclonal antibody therapies with emergency use authorization (EUA) and applicable administration codes:
Billing Monoclonal Antibody Therapeutics
Medicare will pay for COVID-19 mAb under the Medicare Part B vaccine benefit through the end of the calendar year that the PHE ends — so at least Dec. 31, 2022. Medicare payment is typically at reasonable cost or at 95 percent of the average sales price (ASP). See payment allowance limits for Medicare Part B drugs, effective Jan.
Popular Posts:
- 1. icd-10 code for total hip replacement unspecified
- 2. icd code for intertrochanteric bursitis
- 3. icd 10 code for copd with emphysema and is benign
- 4. icd 10 cm code for cholelithiasis
- 5. icd 10 code for work release
- 6. icd code for chronic pelvic peritonitis abscess.
- 7. icd 9 code for forefoot pain
- 8. what is the icd 10 cm code for l71.9
- 9. icd 10 cm code for episiotomy pain
- 10. icd 10 code for left forearm sprain