What is the diagnosis code for anemia?
Code D64. 9 is the diagnosis code used for Anemia, Unspecified, it falls under the category of diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism. Anemia specifically, is a condition in which the number of red blood cells is below normal.
What are symptoms of myelodysplastic syndrome?
They can include:
- weakness, tiredness and occasional breathlessness (because of the low number of red blood cells)
- frequent infections (because of the low number of white blood cells)
- bruising and easy bleeding, such as nosebleeds (because of the low number of platelets)
What are some causes of myelodysplastic syndromes?
Some of these substances are:
- tobacco smoke
- pesticides
- fertilizers
- solvents such as benzene
- heavy metals such as mercury and lead
How is sideroblastic anemia diagnosed?
- Analyzes confirming the presence of sidero-achestic anemia. ...
- Analyzes that specify the form of sidero-achestic anemia. ...
- Anamnesis of a child's life. ...
- Family history - the presence of sideroblastic anemia in relatives.
What is the ICD-10 code for myelodysplastic syndromes?
9.
Is myelodysplastic syndrome Normocytic anemia?
Most patients with myelodysplastic syndromes (MDS) have macrocytic or normocytic anemia as a result of ineffective erythropoiesis due to clonal hematopoiesis.
Is myelodysplastic syndrome the same as refractory anemia?
Refractory anemia is a component of each of the myelodysplastic syndromes (MDSs). MDSs are acquired pluripotent stem cell disorders leading to one or more peripheral blood cytopenias with dysplasia in the peripheral blood and bone marrow.
Is anemia integral to myelodysplastic syndrome?
Background: Anemia is an established negative prognostic factor in myelodysplastic syndromes but the relationship between its degree and clinical outcome is poorly defined. We, therefore, studied the relationship between severity of anemia and outcome in myelodysplastic syndrome patients.
What is myelodysplasia anemia?
Myelodysplastic syndrome (also called myelodysplasia) happens when your blood stem cells don't become healthy blood cells. Myelodysplasia can cause serious conditions like anemia, frequent infections and bleeding that won't stop.
What type of anemia is normocytic normochromic anemia?
Normocytic normochromic anemia is the type of anemia in which the circulating red blood cells (RBCs) are the same size (normocytic) and have a normal red color (normochromic). Most of the normochromic, normocytic anemias are a consequence of other diseases; a minority reflects a primary disorder of the blood.
What is the difference between aplastic anemia and myelodysplastic syndrome?
The main difference between the two disorders is that in aplastic anemia the major problem is almost complete absence of any blood-producing cells in the marrow while in MDS the marrow contains cells but they are defective and abnormal.
What is refractory Anaemia anemia?
Iron-refractory iron deficiency anemia (IRIDA) is a type of iron deficiency anemia that typically does not improve with oral iron treatment. Children with IRIDA have too little iron in their blood, which causes their red blood cells to be small (microcytic) and pale (hypochromic).
What are the types of myelodysplastic syndrome?
Based on these factors, the WHO system recognizes 6 main types of MDS:MDS with multilineage dysplasia (MDS-MLD)MDS with single lineage dysplasia (MDS-SLD)MDS with ring sideroblasts (MDS-RS)MDS with excess blasts (MDS-EB)MDS with isolated del(5q)MDS, unclassifiable (MDS-U)
What causes myelodysplastic syndrome?
This syndrome is caused by inherited changes in the RUNX1 gene. Normally, this gene helps control the development of blood cells. Changes in this gene can lead to blood cells not maturing like they normally would, which can increase the risk of developing MDS.
Is pancytopenia the same as MDS?
Myelodysplastic syndromes (MDS) are malignant stem-cell diseases that are usually diagnosed in elderly patients who present with anemia or, less commonly, bi- or pancytopenia. Their incidence in persons over age 80 is above 50 new cases per 100 000 persons per year.
Who myelodysplastic syndrome classification?
The WHO classification scheme for MDS was published in 1999. Updates to the scheme were published in 2008 and 2016. The 2016 WHO classification of MDS is as follows : MDS with single-lineage dysplasia (MDS-SLD) – 1 or 2 blood cytopenias; in bone marrow, dysplasia in ≥ 10% of one cell line, < 5% blasts.
What are the treatment options for myelodysplastic syndrome?
Treatment options include transfusions, drug therapy, chemotherapy, and blood or bone marrow stem cell transplants. nih national cancer institute. Codes. D46 Myelodysplastic syndromes.
What is a bone marrow disorder?
(who, 2001) A disorder characterized by insufficiently healthy hematapoietic cell production by the bone marrow. A group of diseases in which the bone marrow does not make enough healthy blood cells.
Is bone marrow a preleukemia?
They predominantly affect patients over 60, are considered preleukemic conditions, and have high probability of transformation into acute myeloid leukemia. Your bone marrow is the spongy tissue inside some of your bones, such as your hip and thigh bones. It contains immature cells, called stem cells.
What is the table of neoplasms used for?
The Table of Neoplasms should be used to identify the correct topography code. In a few cases, such as for malignant melanoma and certain neuroendocrine tumors, the morphology (histologic type) is included in the category and codes. Primary malignant neoplasms overlapping site boundaries.
What is a type 2 exclude note?
A type 2 excludes note indicates that the condition excluded is not part of the condition it is excluded from but a patient may have both conditions at the same time. When a type 2 excludes note appears under a code it is acceptable to use both the code ( D46) and the excluded code together.
Is myelodysplastic syndrome rare?
myelodysplastic syndromes are rare. People at higher risk are over 60, have had chemotherapy or radiation therapy, or have been exposed to certain chemicals. Treatment options include transfusions, drug therapy, chemotherapy, and blood or bone marrow stem cell transplants. nih national cancer institute. Code History.
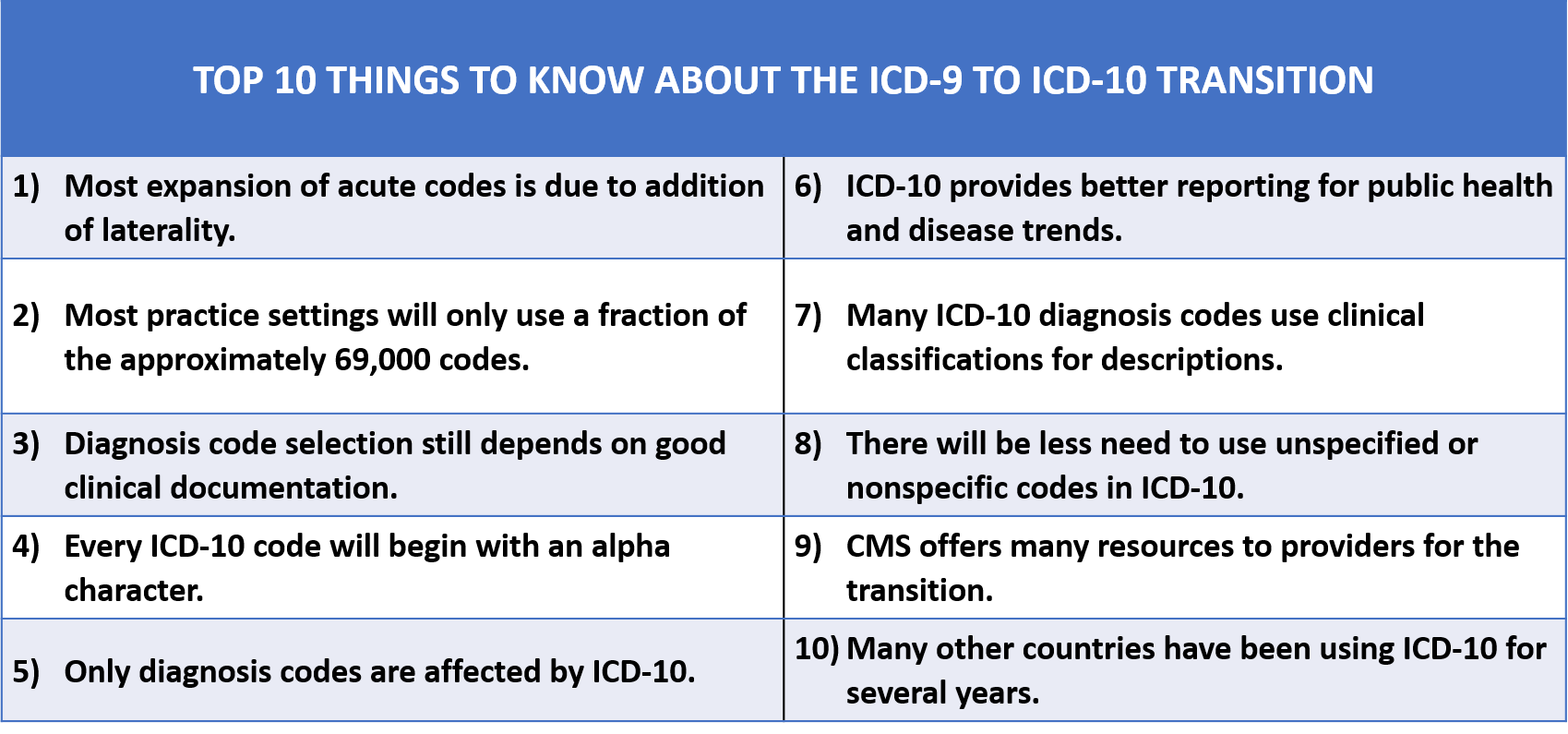
What is the ICD code for myelodysplastic syndrome?
Use a child code to capture more detail. ICD Code D46 is a non-billable code. To code a diagnosis of this type, you must use one of the nine child codes of D46 that describes the diagnosis 'myelodysplastic syndromes' in more detail.
What is an additional code note?
Additional Code Note: Use Additional Code. Use Additional Code note means a second code must be used in conjunction with this code. Codes with this note are Etiology codes and must be followed by a Manifestation code or codes.
What is the code for a primary malignant neoplasm?
A primary malignant neoplasm that overlaps two or more contiguous (next to each other) sites should be classified to the subcategory/code .8 ('overlapping lesion'), unless the combination is specifically indexed elsewhere.
What is a neoplasm of unspecified behavior?
neoplasms of unspecified behavior ( D49.-) A myelodysplastic syndrome character ized by an anemia in which 15% or more of the erythroid precursors are ringed sideroblasts. The ring sideroblast is an erythroid precursor in which one third or more of the nucleus is encircled by granules which are positive for iron stain.
What is the table of neoplasms used for?
The Table of Neoplasms should be used to identify the correct topography code. In a few cases, such as for malignant melanoma and certain neuroendocrine tumors, the morphology (histologic type) is included in the category and codes. Primary malignant neoplasms overlapping site boundaries.
What is the code for a primary malignant neoplasm?
A primary malignant neoplasm that overlaps two or more contiguous (next to each other) sites should be classified to the subcategory/code .8 ('overlapping lesion'), unless the combination is specifically indexed elsewhere.
What is the table of neoplasms used for?
The Table of Neoplasms should be used to identify the correct topography code. In a few cases, such as for malignant melanoma and certain neuroendocrine tumors, the morphology (histologic type) is included in the category and codes. Primary malignant neoplasms overlapping site boundaries.
Abstractor Notes
The principle site s of involvement are the peripheral blood and bone marrow. Any one of the cell type s can be low and look abnormal under the microscope.
Diagnostic Confirmation
This histology can be determined by positive histology (including peripheral blood) with or without genetics and/or immunophenotyping. Review the Definitive Diagnostic Methods, Immunophenotyping and Genetics Data sections below, and the instructions in the Hematopoietic Manual for further guidance on assigning Diagnostic confirmation.
Sources
International Classification of Diseases for Oncology, Third Edition, Second Revision. Geneva: World Health Organization, 2020.
Popular Posts:
- 1. icd 10 code for conjugated hyperbilirubinemia
- 2. icd 10 code for medical clearance for school
- 3. icd 10 cm code for oxygen dependence on ventilator
- 4. icd-10 cm code for chondromalacia
- 5. icd-10 code for parkinson dementia
- 6. icd 9 code for thc abuse]
- 7. icd-10 code for rectocele
- 8. icd 10 code for fractured teeth
- 9. icd 10 diagnosis code for crohn's disease
- 10. icd 10 code for dapsone reaction