What is the HCPCS code for a nebulizer?
Oct 01, 2021 · 2022 ICD-10-CM Diagnosis Code Z79.51 Long term (current) use of inhaled steroids 2016 2017 2018 2019 2020 2021 2022 Billable/Specific Code POA Exempt Z79.51 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z79.51 became effective on October 1, 2021.
What is the ICD 10 code for inhalation?
Policy Appendix: Applicable Code List Nebulizers: Diagnosis Codes . This list of codes applies to the Medicare Advantage Policy Guideline titled Nebulizers. Approval Date: September 8, 2021 . Applicable Codes . The following list(s) of procedure and/or diagnosis codes is provided for reference purposes only and may not be all inclusive.
What is the a7003 code for a nebulizer?
Oct 01, 2021 · Z99.89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z99.89 became effective on October 1, 2021. This is the American ICD-10-CM version of Z99.89 - other international versions of ICD-10 Z99.89 may differ.
What is the ICD 10 code for urinalysis?
Apr 30, 2018 · Nebulizer . A7003, A7004, A7005 . dornase alpha (J7639) tobramycin (J7682) acetylcysteine (J7608) Bronchiectasis 2° (A15.0, J47.0, J47.1, J47.9, E0570 Small Volume Nebulizer . A7003, A7004, tobramycin (J7682)
What diagnoses cover a nebulizer?
Doctors recommend nebulizers to treat:asthma.bronchitis.bronchiectasis.COPD.cystic fibrosis.respiratory infections.
What is the CPT code for nebulizer treatment?
The code for the nebulizer treatment is, "94640 Pressurized or nonpressurized inhalation treatment for acute airway obstruction for therapeutic purposes and/or for diagnostic purposes such as sputum induction with an aerosol generator, nebulizer, metered dose inhaler or intermittent positive pressure breathing (IPPB) ...Jun 12, 2018
How do you bill for a nebulizer treatment?
If the patient receives a nebulizer treatment of less than 1 hour (CPT code 94640) during an episode of care and subsequently returns on the same date of service to the urgent care to receive another nebulizer treatment of less than 1e hour, then you would bill CPT code 94640 and append modifier -76, “Repeat procedure ...Oct 2, 2017
How do I bill for Albuterol treatment?
J7613, 'Albuterol, inhalation solution, FDA-approved final product, non-compounded, administered through DME, unit dose, 1 mg'Jul 24, 2019
What is included in CPT code 94010?
CPT code 94010, “Spirometry, including graphic record, total and timed vital capacity, expiratory flow rate measurement(s), with or without maximal voluntary ventilation,” may be separately reported when performed and documented with a six-minute walk test.
What is the CPT code for Albuterol?
HCPCS code J7613 for Albuterol, inhalation solution, FDA-approved final product, non-compounded, administered through DME, unit dose, 1 mg as maintained by CMS falls under Inhalation Solutions .
What does CPT code 94640 mean?
CPT code 94640 describes treatment of acute airway obstruction with inhaled medication and/or the use of an inhalation treatment to induce sputum for diagnostic purposes.
What is modifier 76 medical billing?
Modifier 76 is used to report a repeat procedure or service by the same physician and is appended to the procedure to report: Repeat procedures performed on the same day. Indicate that a procedure or service was repeated subsequent to the original procedure or service.Feb 21, 2020
What ICD 10 DX code covers CPT 94640?
Group 1CodeDescription94640PRESSURIZED OR NONPRESSURIZED INHALATION TREATMENT FOR ACUTE AIRWAY OBSTRUCTION FOR THERAPEUTIC PURPOSES AND/OR FOR DIAGNOSTIC PURPOSES SUCH AS SPUTUM INDUCTION WITH AN AEROSOL GENERATOR, NEBULIZER, METERED DOSE INHALER OR INTERMITTENT POSITIVE PRESSURE BREATHING (IPPB) DEVICE5 more rows
What is CPT code A7003?
HCPCS code A7003 for Administration set, with small volume nonfiltered pneumatic nebulizer, disposable as maintained by CMS falls under Breathing Aids .
What is the CPT code for DuoNeb?
Code J7620 is often called a “DuoNeb” because the nebulizing product is a combination of two medication agents.Sep 1, 2015
Can CPT code 94664 and 94640 be billed together?
To bill both 94640 and 94664 on the same date of service, there must be documentation supporting that the procedures were separate and distinct from one another. The medical record should include a request for each procedure, and therapist documentation should support that procedures occurred at separate times.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, §1833 (e) prohibits Medicare payment for any claim which lacks the necessary information to process the claim.
Article Guidance
The information in this article contains billing, coding or other guidelines that complement the Local Coverage Determination (LCD) for Respiratory Therapy and Oximetry Services L33446.#N#CPT ® code 31720 is payable only if it is personally performed by the physician (or qualified Non-Physician Practitioner (NPP)).#N#Note:#N#CPT ® codes 94760, 94761 and 94762 are bundled by the Correct Coding Initiative (CCI) with critical care services.
ICD-10-CM Codes that Support Medical Necessity
The CPT/HCPCS codes included in this Billing and Coding: Respiratory Therapy and Oximetry Services A56730 article will be subjected to "procedure to diagnosis" editing. The following list includes only those diagnoses for which the identified CPT/HCPCS procedures are covered.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
Document Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
CMS Manual System, Pub. 100-03, Medicare National Coverage Determinations Manual, Chapter 1, Section 200.2, Section 280.1
Coverage Guidance
For any item to be covered by Medicare, it must 1) be eligible for a defined Medicare benefit category, 2) be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and 3) meet all other applicable Medicare statutory and regulatory requirements.#N#The purpose of a Local Coverage Determination (LCD) is to provide information regarding “reasonable and necessary” criteria based on Social Security Act § 1862 (a) (1) (A) provisions.#N#In addition to the “reasonable and necessary” criteria contained in this LCD there are other payment rules, which are discussed in the following documents, that must also be met prior to Medicare reimbursement:.
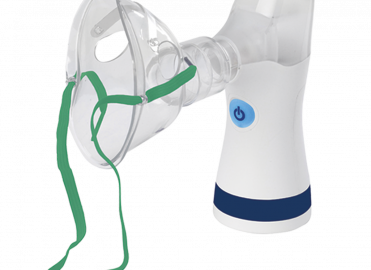
What is a nebulizer?
Commonly used as bronchodilators, nebulizers are medical devices that can convert liquids into aerosols in the form of mist, so that it can be easily inhaled into the lower respiratory tract. This device plays a crucial part in the treatment of patients suffering from respiratory diseases such as asthma and chronic obstructive pulmonary disease (COPD). It works by relaxing and opening air passages to the lungs to make breathing easier. Medicare Part B covers nebulizers and some medicines used in nebulizers, only if they are considered reasonable and necessary. These are covered as durable medical equipment (DME) that your doctor prescribes for use in your home. Hospitals providing this treatment can consider medical billing services provided by experienced firms to submit error-free claims for reimbursement. Nebulizer devices are often used to deliver bronchodilator (airway-opening) medications such as albuterol, Xopenex or Pulmicort. Nebulizer medications are prescribed in unitdose vials and multidose bottles.
Does Medicare cover nebulizers?
It works by relaxing and opening air passages to the lungs to make breathing easier. Medicare Part B covers nebulizers and some medicines used in nebulizers, only if they are considered reasonable and necessary. These are covered as durable medical equipment (DME) that your doctor prescribes for use in your home.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
For any item to be covered by Medicare, it must 1) be eligible for a defined Medicare benefit category, 2) be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and 3) meet all other applicable Medicare statutory and regulatory requirements.
ICD-10-CM Codes that Support Medical Necessity
The presence of an ICD-10 code listed in this section is not sufficient by itself to assure coverage. Refer to the LCD section on “ Coverage Indications, Limitations, and/or Medical Necessity ” for other coverage criteria and payment information.#N#For HCPCS codes A4619, E0565, E0572:
ICD-10-CM Codes that DO NOT Support Medical Necessity
For the specific HCPCS codes indicated above, all ICD-10 codes that are not specified in the previous section.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
Wednesday, November 15, 2017
For a DME item to be covered by Medicare, it must 1) be eligible for a defined Medicare benefit category, 2) be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and 3) meet all other applicable Medicare statutory and regulatory requirements.
Nebulizer cpt code list - A7017, A7018, A7007
For a DME item to be covered by Medicare, it must 1) be eligible for a defined Medicare benefit category, 2) be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and 3) meet all other applicable Medicare statutory and regulatory requirements.

Popular Posts:
- 1. icd 10 code for bike riding
- 2. icd 10 code for acute appendicitis with perforation
- 3. icd 10 code for skin staph aureus skin infection,
- 4. icd 10 code for surgical wound infection of left leg amputation
- 5. icd 10 code for newborn twin, male, delivered by cesarean delivery
- 6. icd 9 code for endotracheal infection
- 7. 2017 icd 10 code for addenopathy retroperitoneal
- 8. icd 10 code for candidal paronychia
- 9. icd code for hyperplasia of appendix
- 10. icd 10 code for right breast implant rupture