Can you ever use an unspecified ICD-10 code?
In both ICD-9 and ICD-10, signs/symptoms and unspecified codes are acceptable and may even be necessary. In some cases, there may not be enough information to describe the patient's condition or no other code is available to use. Although you should report specific diagnosis codes when they are supported by the available documentation and clinical knowledge of the patient's health condition, in some cases, signs/symptoms or unspecified codes are the best choice to accurately reflect the ...
What is a valid ICD 10 code?
Z20.822 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z20.822 became effective on October 1, 2021. This is the American ICD-10-CM version of Z20.822 - other international versions of ICD-10 Z20.822 may differ. Z codes represent reasons for encounters.
What is the ICD 10 code for altered level of consciousness?
A Altered Level of Consciousness ICD-10-CM diagnosis code R41.82 Altered mental status, unspecified would not be appropriate. An EXCLUDES note lists altered level of consciousness (R40.-).
What is the ICD 10 code for IDDM?
code for iddm and niddm They would both be 250.00 with the v58.67 for iddm added.
When do you code E11 21?
Type 2 diabetes mellitus with diabetic nephropathy E11. 21 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM E11. 21 became effective on October 1, 2021.
What is diagnosis code E11 22?
ICD-10 code: E11. 22 Type 2 diabetes mellitus With renal complications With other multiple complications, controlled.
What is the difference between E11 21 and E11 22?
E11. 22 states within its code DM with CKD therefore it is a more accurate code than E11. 21 which is just DM with Nephropathy (any kidney condition).
When do you code E11 29?
ICD-10 Code for Type 2 diabetes mellitus with other diabetic kidney complication- E11. 29- Codify by AAPC.
When do you code E11 69?
ICD-10-CM Code for Type 2 diabetes mellitus with other specified complication E11. 69.
When do you use E11 59?
Type 2 diabetes mellitus with other circulatory complications. E11. 59 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
Can you code E11 9 and E11 22 together?
So yes, use the appropriate combination codes, being E11. 22, I12. 9 and N18. 3.
What type of diabetes are included in Category E11?
ICD-10 Code Z79. 4, Long-term (current) use of insulin should be assigned to indicate that the patient uses insulin for Type 2 diabetes mellitus (Category E11* codes).
Can you code E11 40 and E11 42?
If you look in the alphabetical index under diabetes/diabetic with neuropathy it is E11. 40 (type 2 DM with diabetic neuropathy, unspecified). You cannot go with E11. 42 because that is specifically with polyneuropathy which is not documented.
What type of diabetes is e13 9?
9: Other specified diabetes mellitus Without complications.
How do you code diabetes with chronic kidney disease?
E11. 22, Type 2 diabetes mellitus with diabetic CKD. I12. 9, hypertensive CKD with stage 1 through 4 CKD, or unspecified CKD.
What is the code for long term use of insulin?
4.
What is the ICD-10 code for chronic kidney disease?
9.
What is the ICD-10 code for type 2 diabetes?
ICD-Code E11* is a non-billable ICD-10 code used for healthcare diagnosis reimbursement of Type 2 Diabetes Mellitus. Its corresponding ICD-9 code is 250. Code I10 is the diagnosis code used for Type 2 Diabetes Mellitus.
What is the code for diabetes mellitus?
The body system (s) affected 3. The complications affecting the body system (s) When coding diabetes mellitus, you should use as many codes from categories E08-E13* as necessary to describe all of the complications and associated conditions of the disease.
What is the correct ICD-9 code for diabetes mellitus?
Most coders can quickly come up with 250.00. And if the physician only documented diabetes mellitus , that’s the correct ICD-9-CM code. If a physician doesn’t document complications or type of diabetes, coders default to code 250.00 (diabetes mellitus without mention of complications), says Jill Young, CPC, CEDC, CIMC, president of Young Medical Consulting, LLC, in East Lansing, MI. However, 250.00 is not necessarily the best code to describe the patient’s actual condition. Consider these two patients. Patient A is a type 2 diabetic with well controlled diabetes. Patient B is a type 2 diabetic with uncontrolled diabetes who also suffers from diabetes-related chronic kidney disease. If the physician documents “diabetes mellitus” for both patients, coders would report the same code, even though the patients have very different conditions. The physician loses reimbursement on Patient B, who is sicker and requires more care, Young says. Coding in ICD-9-CM When it comes to the code assignment for diabetes mellitus in ICD-9-CM (250 code series), coders identify whether the diabetes is type 1or 2 using a fifth digit, says Shannon E. McCall, RHIA, CCS, CCS-P, CPC, CPC-I, CEMC, CCDS, director of HIM/coding for HCPro, Inc., in Danvers, Mass, and an AHIMA-approved ICD-10-CM/PCS trainer. If the diabetes is secondary, coders choose from codes in the 249 series. Under series 250, coders will find 10 different subcategories that further define and refine the patient’s actual condition. All of those codes require a fifth digit to indicate whether the diabetes is controlled or uncontrolled, type 1or type 2. The fifth digit subclassifications are: Coders also need to note that codes 250.4, 250.5, 250.6, 250.7, and 250.8 all include instructions to use an additional code to ide Continue reading >>
What is type 2 diabetes?
Type 2 Diabetes Mellitus E11- >. A disease in which the body does not control the amount of glucose (a type of sugar) in the blood and the kidneys make a large amount of urine. This disease occurs when the body does not make enough insulin or does not use it the way it should.
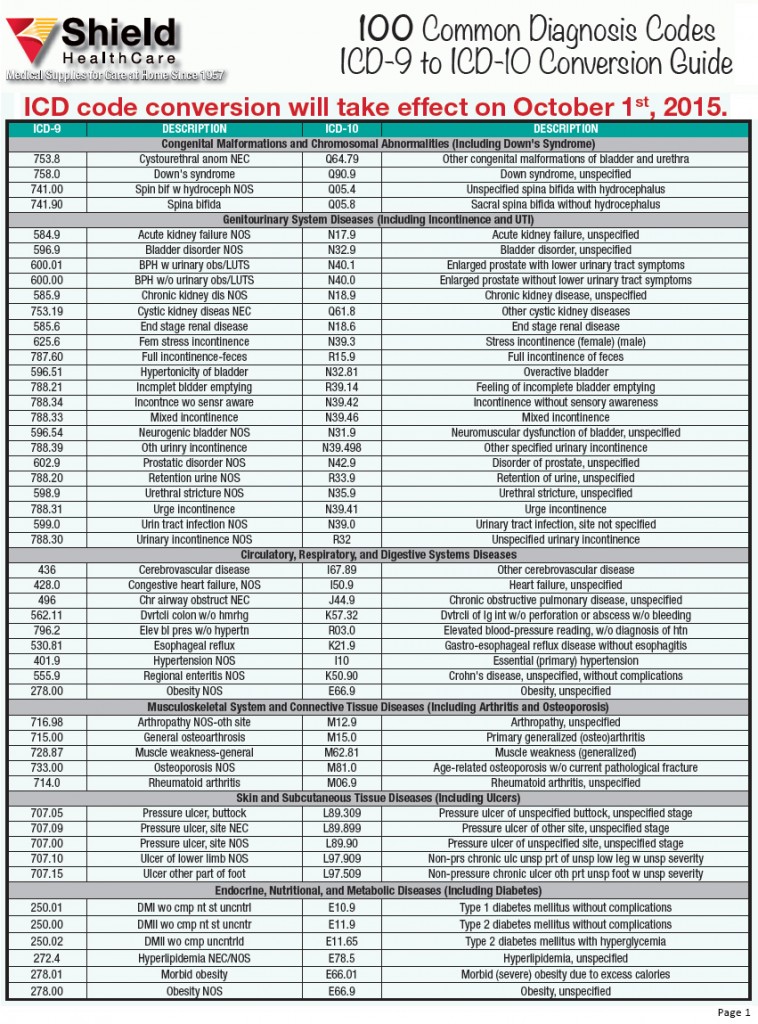
Why is it important to have ICD-9 codes?
Providing the most specific ICD-9 codes is important for several reasons. For one, many hospitals use these codes to keep track of their utilization management. ICD-9 codes are also used by public health officials to track epidemics, create census reports, and for medical research purposes.
Does diabetes mellitus translate to ICD-10?
1. How you state it in the chart matters. Current documentation of noninsulin-dependent diabetes mellitus does not translate to ICD-10. Therefore, language such as “controlled” or “uncontrolled” and “juvenile-onset” or “adult-onset” has become obsolete.
What is type 2 diabetes mellitus?
Subclass of diabetes mellitus that is not insulin responsive or dependent; characterized initially by insulin resistance and hyperinsulinemia and eventually by glucose intolerance, hyperglycemia, and overt diabetes; type ii diabetes mellitus is no longer considered a disease exclusively found in adults; patients seldom develop ketosis but often exhibit obesity.
What is Type II diabetes?
A subclass of diabetes mellitus that is not insulin-responsive or dependent (niddm). It is characterized initially by insulin resistance and hyperinsulinemia; and eventually by glucose intolerance; hyperglycemia; and overt diabetes. Type ii diabetes mellitus is no longer considered a disease exclusively found in adults. Patients seldom develop ketosis but often exhibit obesity.
When will the ICD-10-CM E11.329 be released?
The 2022 edition of ICD-10-CM E11.329 became effective on October 1, 2021.
Can E11.329 be used for reimbursement?
E11.329 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail. Short description: Type 2 diab w mild nonprlf diabetic rtnop w/o macular edema.
What is the ICd 10 code for diabetes?
These include drug- or chemical-induced diabetes mellitus (E09.-); gestational diabetes (Q24.4-); neonatal diabetes mellitus (P70.2); and postpancreatectomy, postprocedural, or secondary diabetes mellitus (E13.-).
What chapter is ICd 10 for diabetic retinopathy?
Finding the ICD-10 codes for diabetic retinopathy can be tricky. They are not listed in Chapter 7, Diseases of the Eye and Adnexa (H00-H59), but are in the diabetes section (E08-E13) of Chapter 4, Endocrine, Nutritional and Metabolic Diseases.
How many people have NIDDM?
Therefore, up to approximately four million Americans may have an autoimmune type of NIDDM.
How many NIDDM patients are recruited per year?
To determine who among these individuals will be more prone to develop the disease and consequently be exposed to its pathologic consequences, including for example, heart failure, the Institute will recruit approximately 300 NIDDM patients per year. Glycemic control will be assessed by periodic monitoring of glycated hemoglobin; a 10-minute intravenous glucose tolerance test (IVGTT) to assess first phase insulin release (FPIR); C-peptide and total insulin; as well as by home blood glucose monitoring performed by the patients. Each subject will have an HLA typing and an annual examination of beta-cell autoimmunity markers.
What is the cause of impaired skeletal muscle FFA uptake and oxidation in NIDDM?
The first hypothesis is that hyperglycemia is the principal cause of impaired skeletal muscle FFA uptake and oxidation in NIDDM. The second hypothesis is that activity of muscle carnitine-palmitoyl transferase (CPTI) is reduced in NIDDM, caused by allosteric inhibition from muscle malonyl CoA, which we postulate to be increased due to hyperglycemia . The hypothesis that FFA uptake is reduced by hyperglycemia during post-absorptive conditions can be tested in two clinical investigations.
Can NIDDM predict beta cell loss?
This study will provide information regarding the feasibility to predict a loss of beta-cell function in patients clinically diagnosed with NIDDM by using a combined analysis of immunological as well as genetic markers of beta-cell autoimmunity and will give new insight for the selection of candidates for safe prevention of insulin dependency among NIDDM patients.

Popular Posts:
- 1. icd-10-cm code for hemoglobinemia
- 2. icd 10 code for end stage glenohumeral arthritis
- 3. icd 9 code for total parenteral nutrition
- 4. icd 10 code for left frontal sinus bone fracture
- 5. icd 10 code for removal of c-section sutures
- 6. icd 10 code for hymenal remnant
- 7. icd 10 code for tonsil abscess
- 8. icd 10 code for temporomandibular joint syndrome
- 9. icd 9 code for menstruation
- 10. icd 10 code for loss of smell and taste