What is a valid ICD 10 code?
The following 72,752 ICD-10-CM codes are billable/specific and can be used to indicate a diagnosis for reimbursement purposes as there are no codes with a greater level of specificity under each code. Displaying codes 1-100 of 72,752: A00.0 Cholera due to Vibrio cholerae 01, biovar cholerae. A00.1 Cholera due to Vibrio cholerae 01, biovar eltor. A00.9 Cholera, unspecified.
What are the common ICD 10 codes?
ICD-10-CM CATEGORY CODE RANGE SPECIFIC CONDITION ICD-10 CODE Diseases of the Circulatory System I00 –I99 Essential hypertension I10 Unspecified atrial fibrillation I48.91 Diseases of the Respiratory System J00 –J99 Acute pharyngitis, NOS J02.9 Acute upper respiratory infection J06._ Acute bronchitis, *,unspecified J20.9 Vasomotor rhinitis J30.0
What are the unusual ICD-10 codes?
The Strangest and Most Obscure ICD-10 Codes Burn Due to Water Skis on Fire (V91.07X) Other Contact With Pig (W55.49X) Problems in Relationship With In-Laws (Z63.1) Sucked Into Jet Engine (V97.33X) Fall On Board Merchant Ship (V93.30X) Struck By Turkey (W61.42XA) Bizarre Personal Appearance (R46.1)
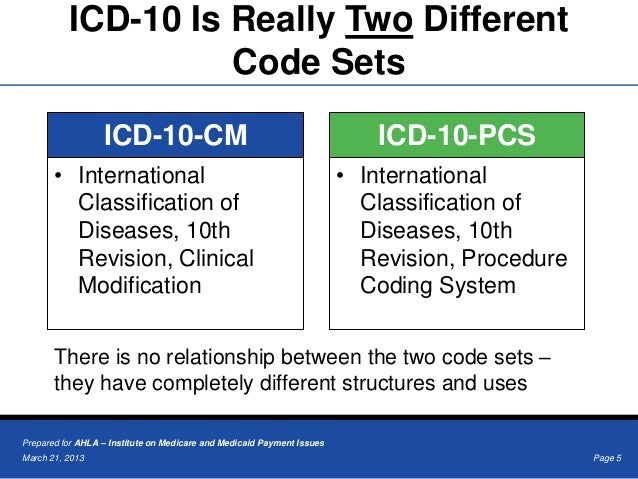
What you should know about ICD-10 codes?
Why ICD-10 codes are important
- The ICD-10 code system offers accurate and up-to-date procedure codes to improve health care cost and ensure fair reimbursement policies. ...
- ICD-10-CM has been adopted internationally to facilitate implementation of quality health care as well as its comparison on a global scale.
- Compared to the previous version (i.e. ...
What is the ICD 10 code for non compliant with medication?
1 for Patient's noncompliance with medical treatment and regimen is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is the F code for no diagnosis?
2022 ICD-10-CM Diagnosis Code Z71. 1: Person with feared health complaint in whom no diagnosis is made.
What is the ICD-10 diagnosis code for left without being seen?
Z53.21Z53. 21 - Procedure and treatment not carried out due to patient leaving prior to being seen by health care provider | ICD-10-CM.
How do you code a procedure not carried out?
ICD-10-CM Code for Procedure and treatment not carried out because of other contraindication Z53. 09.
What is the ICD-10 code for suspected condition not found?
89 - Encounter for observation for other suspected diseases and conditions ruled out | ICD-10-CM.
What is a deferred diagnosis?
Surgical pathology An intraoperative consultation in which tissues of interest to the surgeon are cut, stained, and examined by LM, but a final diagnosis delayed pending final–paraffin–sections.
How do you bill when patient leaves AMA?
A: You can't bill anything for day 1 because the physician's evaluation wasn't done until the next day when the patient was seen, treated and discharged. Use the same-day admit and discharge (99234- 99236) codes based on your level of history, exam and medical decision-making.
What is the ICD 10 code for leaving against medical advice?
Z53.21Left Against Medical Advice is indexed in ICD-10-CM as Z53. 21, which implies that the patient has seen a healthcare professional.
Why do patients leave the ER without being seen?
Sometimes patients who come to a pediatric emergency room (ER) leave before they are seen by a health care provider. A long wait time is a common reason for patients choosing to leave. Patients who leave the ER before being seen by a health care provider may delay care that is important to their health.
How do you code a Cancelled procedure in ICD-10?
Z53. 8 is assigned as an additional diagnosis as per ACS 0011; and ICD-10-AM Alphabetic Index pathway: Cancelled procedure, because of, specified reason.
What is the modifier for incomplete procedure?
For modifier 52, CPT® Appendix A explains: "Under certain circumstances a service or procedure is partially reduced or eliminated at the physician's discretion.
What is the modifier for discontinued procedure?
Modifier 53Modifier 53 — Discontinued Procedure Add this modifier to a surgical or diagnostic procedure code when the physician elects to terminate the procedure due to the patient's well-being.
When will the ICD-10 Z53.9 be released?
The 2022 edition of ICD-10-CM Z53.9 became effective on October 1, 2021.
Why is Z53.20 not carried out?
Z53.20 Procedure and treatment not carried out because of patient's decision for unspecified reasons. Z53.21 Procedure and treatment not carried out due to patient leaving prior to being seen by health care provider. Z53.29 Procedure and treatment not carried out because of patient's decision for other reasons.
What is a Z40-Z53?
Categories Z40-Z53 are intended for use to indicate a reason for care. They may be used for patients who have already been treated for a disease or injury, but who are receiving aftercare or prophylactic care, or care to consolidate the treatment, or to deal with a residual state. Type 2 Excludes.
What is Z71 in medical?
Z71- Persons encountering health services for other counseling and medical advice , not elsewhere classified
What is a Z00-Z99?
Categories Z00-Z99 are provided for occasions when circumstances other than a disease, injury or external cause classifiable to categories A00 -Y89 are recorded as 'diagnoses' or 'problems'. This can arise in two main ways:
What does "exclude note" mean?
A type 1 excludes note is a pure excludes. It means "not coded here". A type 1 excludes note indicates that the code excluded should never be used at the same time as Z71.1. A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition.
When will the Z71.1 be released?
The 2022 edition of ICD-10-CM Z71.1 became effective on October 1, 2021.
What is the ICD-10 code for a nonspecific condition?
ICD-10 guidelines offer clear specifications on billing codes even when a nonspecific condition presents itself and no diagnosis is forthcoming. While the process of arriving at the correct code may be confusing, getting the coding correct will lead to accurate billing, which translates into timelier payments, happier patients, and avoidance of underpayments. As such, every effort should be made to research and apply the appropriate codes, even in cases where the physician cannot make a diagnosis.
Why is there no diagnosis in medical billing?
In many cases, patients come in with symptoms that prompt them to seek medical treatment, yet the physician can make no diagnosis. These cases often result in errors in medical billing coding due to confusion about how to handle the situation. However, in every case, a method exists for proper coding and billing for treatment.
Why do patients leave the office without a diagnosis?
There are many reasons that a patient might report to a physician and leave the office without a diagnosis – maybe the symptoms are nonspecific, or maybe the patient requires a referral to a specialist better suited to make the correct diagnosis. No matter what the reason, coding and billing these cases can be pretty tricky. Medical claims processing is often a complicated and difficult task, and when no diagnosis is reached, properly coding these cases presents a unique challenge.
Why is a symptom not part of a diagnosis?
If the symptom is not part of the diagnosis, it may be listed as part of the history of diagnosis to better explain how the diagnosis was reached, or what obstacles led to difficulties in achieving a diagnosis.
Can you code a follow up visit?
However, there are codes relating to follow-up visits. Coding follow-up visits improperly is a common source of errors and should be very handled carefully. Many times, the follow-up is incorrectly billed as part of the original diagnosis rather than billed as a follow-up visit. This often results in overcharging the patient and insurance company for the visit, and may even have the claim denied under inappropriate billing codes. Be sure to use the proper follow-up visit codes to avoid this error.
Can symptoms disappear before diagnosis?
In many cases, the symptoms were transient and disappear before any diagnosis can be made. In this case, the symptoms themselves are listed in the coding for the billing. In other cases, the symptoms may not immediately lend themselves to a diagnosis; however, rather than returning for a follow-up visit, the patient may elect to find ...
Is coding a medical claim difficult?
No matter what the reason, coding and billing these cases can be pretty tricky. Medical claims processing is often a complicated and difficult task, and when no diagnosis is reached, properly coding these cases presents a unique challenge. Coding a claim incorrectly can be costly for both your practice and for the patient.
Why is Z53.09 not carried out?
Z53.09 Procedure and treatment not carried out because of other contraindication. Z53.1 Procedure and treatment not carried out because of patient's decision for reasons of belief and group pressure. Z53.2 Procedure and treatment not carried out because of patient's decision for other and unspecified reasons.
What is a Z00-Z99?
Categories Z00-Z99 are provided for occasions when circumstances other than a disease, injury or external cause classifiable to categories A00 -Y89 are recorded as 'diagnoses' or 'problems'. This can arise in two main ways:
Can you use Z53 for reimbursement?
Persons encountering health services for specific procedures and treatment, not carried out. Z53 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail.
When will the 2022 ICd-10-CM Z09 be released?
The 2022 edition of ICD-10-CM Z09 became effective on October 1, 2021.
What is Z09 encounter?
Z09- Encounter for follow-up examination after completed treatment for conditions other than malignant neoplasm
What does "type 1 excludes" mean?
A type 1 excludes note is a pure excludes. It means "not coded here". A type 1 excludes note indicates that the code excluded should never be used at the same time as Z09. A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition.
What does the title of a manifestation code mean?
In most cases the manifestation codes will have in the code title, "in diseases classified elsewhere.". Codes with this title are a component of the etiology/manifestation convention. The code title indicates that it is a manifestation code.
When will the ICd 10-CM R03.0 be released?
The 2022 edition of ICD-10-CM R03.0 became effective on October 1, 2021.
Is R03.0 a good admission?
R03.0 is not usually sufficient justification for admission to an acute care hospital when used a principal diagnosis.
When did we switch to ICD-10?
As you probably know, on October 1st we all had to switch to using ICD-10 codes for billing purposes.
What is the difference between Z71.1 and Z03.89?
The difference is that Z71.1 implies that the clinician has chosen not to make a diagnosis based on info that is available, whereas Z03.89 states that all suspected conditions have been ruled out. An important nuance that does little to clarify which I should be using!
Common Circumstances Where No Diagnosis May Be Reached
- There are several circumstances that may arise for a doctor/patient visit that does not result in a diagnosis being reached. For many of these circumstances, there are clear guidelines for medical claims processing on how to code and bill for these services. Preventive care services are often covered by a patient’s insurance and can be billed under the appropriate code for the visit. Thes…
Cases Where An Ill Patient Does Not Receive A Diagnosis
- In many cases, patients come in with symptoms that prompt them to seek medical treatment, yet the physician can make no diagnosis. These cases often result in errors in medical billing coding due to confusion about how to handle the situation. However, in every case, a method exists for proper coding and billingfor treatment. In many cases, where a diagnosis is not immediately abl…
Avoiding Overbilling For Nonspecific Conditions
- ICD-10 guidelines offer clear specifications on billing codes even when a nonspecific condition presents itself and no diagnosis is forthcoming. While the process of arriving at the correct code may be confusing, getting the coding correct will lead to accurate billing, which translates into timelier payments, happier patients, and avoidance of und...
Popular Posts:
- 1. icd 10 code for right hand dupuytren's contracture
- 2. icd 10 code for contused ribs
- 3. icd 10 cm code for scratched by dig
- 4. icd 10 code for fracture of hand
- 5. icd 10 code for paroxysmal hypertension
- 6. icd-10 diagnosis code for neuroendocrine tumor (carcinoid) muscularis propria
- 7. icd 10 code for dm2 with foot ulcer
- 8. icd 9 code for contusion unspecified
- 9. icd 10 cm code for melena
- 10. icd 10 code for unspecified asthma with acute exacerbation