What is the diagnosis code for low back pain?
- BILLABLE CODE - Use M54.50 for Low back pain, unspecified
- BILLABLE CODE - Use M54.51 for Vertebrogenic low back pain
- BILLABLE CODE - Use M54.59 for Other low back pain
What is the ICD 10 code for back pain?
The ICD 10 code M545 is used to define conditions connected with acute back pain (C & O lumbar pain, C & O back pain, or chronic back pain) or complaints about back pain or facet or joint pain. This code is used in common practice, internal medicine, and orthopedic works to define clinical ideas such as neck pain.
What is the CPT code for back pain?
Pain management cpt codes 62310, 62319, 64415 - 64449
- Claims for moderate sedation should be submitted hard copy indicating the medical necessity for the procedure. ...
- Moderate sedation does not include minimal sedation (anxiolysis), deep sedation or monitored anesthesia care (00100-01999).
- Moderate sedation is restricted to recipients from birth to age 13. ...
What is the ICD 10 code for chronic pain?
ICD-10 code G89.4 for Chronic pain syndrome is a medical classification as listed by WHO under the range - Diseases of the nervous system . Subscribe to Codify and get the code details in a flash. headache syndromes ( G44 .-) abdomen pain ( R10 .-) spine pain ( M54 .-)
What is the ICD-10 code for unspecified back pain?
ICD-10-CM Code for Dorsalgia, unspecified M54. 9.
What is the 2021 ICD-10 code for low back pain?
ICD-10 code M54. 5, low back pain, effective October 1, 2021. That means providers cannot use M54. 5 to specify a diagnosis on or after October 1—and existing patients with the M54. 5 diagnosis will need to be updated to a valid ICD-10 code.
What is unspecified back pain?
Non-specific low back pain is defined as low back pain not attributable to a recognizable, known specific pathology (eg, infection, tumour, osteoporosis, lumbar spine fracture, structural deformity, inflammatory disorder,radicular syndrome, or cauda equina syndrome).
Is non specific low back pain a diagnosis?
Nonspecific low back pain is diagnosed on the basis of the exclusion of specific causes, usually by means of history taking and physical examination. Imaging is not routinely indicated in patients with nonspecific low back pain.
What is the new ICD code for low back pain?
M54. 50 (Low back pain, unspecified) M54. 51 (Vertebrogenic low back pain)
What is Dorsalgia unspecified?
Dorsalgia means back or spine pain, including low back, mid back, and sciatic pain. It does not include pain related to scoliosis, lordosis, or other specifically classified conditions.
How common is non specific low back pain?
About 8 in 10 people have one or more bouts of low back pain. In most cases, it is not due to a serious disease or serious back problem, and the exact cause of the pain is not clear. This is called nonspecific lower back pain. The usual advice is to keep active and do normal activities as much as possible.
What is non specific muscle pain?
Non-specific low back pain is the type of back pain that neither you nor your healthcare provider can definitively, accurately trace back to its root. In other words, it is not related to a specific, diagnosable disease. An example is a back muscle strain due to an athletic injury or other trauma.
What is the ICD-10 for chronic back pain?
M54. 9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM M54.
What is mechanical and non mechanical pain?
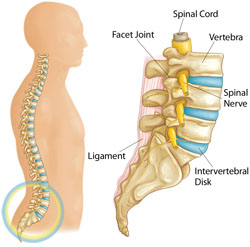
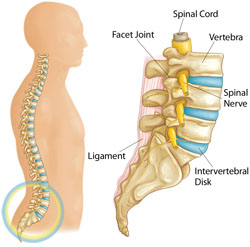
Abstract. Low back pain is usually nonspecific or mechanical. Mechanical low back pain arises intrinsically from the spine, intervertebral disks, or surrounding soft tissues. Clinical clues, or red flags, may help identify cases of nonmechanical low back pain and prompt further evaluation or imaging.
What are the types of back pain?
Types of Back PainHerniated disc(s)Muscle strains (from overuse or poor posture)Muscle injury.Pinched/compressed nerves.Narrowing of the spinal canal (spinal stenosis)Vertebral fracture(s)Osteoporosis.The natural processes of aging.More items...
What is a classification of back pain based on duration?
Low back pain may be classified by duration as acute (pain lasting less than 6 weeks), sub-chronic (6 to 12 weeks), or chronic (more than 12 weeks). The condition may be further classified by the underlying cause as either mechanical, non-mechanical, or referred pain.
How long does back pain last?
Acute back pain comes on suddenly and usually lasts from a few days to a few weeks. Back pain is called chronic if it lasts for more than three months. most back pain goes away on its own, though it may take awhile.
What does it mean when you feel a bad feeling in your back?
Sensation of unpleasant feeling indicating potential or actual damage to some body structure felt in the back.
How long does it take for back pain to go away?
If your back pain is severe or doesn't improve after three days, you should call your health care provider. You should also get medical attention if you have back pain following an injury.treatment for back pain depends on what kind of pain you have, and what is causing it.
When will the ICd 10-CM M54.9 be released?
The 2022 edition of ICD-10-CM M54.9 became effective on October 1, 2021.
Where is chronic pain located?
Acute or chronic pain located in the posterior regions of the thorax, lumbosacral region, or the adjacent regions.
What is the code for lower back pain?
This year, one of the major adjustments that relates to physical therapy practices is the removal of the code M54.5, which is generally used to document lower back pain. Lower back pain is the most common cause of disability in all age groups and accounts for one-fourth to one-third of all causes of disabilities. Lower back pain can be caused by injury, overuse or simply wear and tear on the structures related to normal spine function.
Why was M54.5 removed from the ICd 10?
Both R05 – Cough and R63.3 – Feeding difficulties were also slated for removal. Again, the reason given for removal of these codes is that each is too broad and doesn’t adequately describe a true diagnosis.
Is physical therapy a pain in the back?
There has been a recent development in the lives of providers and front office staff at therapy offices around the country, and to say it has been a pain in the back is to put it mildly. Beginning Oct. 1, one of the most common CMS codes used by physical therapy practices has been removed. This is not a rare occurrence, every year CMS releases a list of changes that are to be made to the Medicare program along with any other changes to the rules and regulations governing healthcare.
Is lower back pain a common complaint?
Lower back pain remains a common complaint for patients seeking treatment from physical therapists across the nation. This change has generated considerable concern among therapists that this move will eliminate payment for many treatments involving lower back pain diagnosis/treatment, including lumbar spine stabilization exercises. Keeping informed about the adjustment to how treatment for lower back pain should be coded though, should prevent any confusion.
Does the ICD-10 manual apply to Medicare?
Though CMS guidance on treatment coding technically only applies to reimburs ement from Medicare and Medicaid, the system has also been adopted by private insurers.
What is the meaning of pain?
Pain is a feeling triggered in the nervous system. Pain may be sharp or dull.
When will the ICD-10-CM R52 be released?
The 2022 edition of ICD-10-CM R52 became effective on October 1, 2021.
How long does pain last?
Once you take care of the problem, pain usually goes away. However, sometimes pain goes on for weeks, months or even years.
What is the pain of the coccyx?
Pain of coccyx greater than 3 months, chronic. Clinical Information. A disorder characterized by the sensation of marked discomfort, distress or agony. An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons.
Popular Posts:
- 1. icd 10 code for hepatitis a exposure
- 2. icd 9 code for acinetobacter bacteremia
- 3. what is the icd-10-cm code for dysphagia
- 4. icd 10 code for right groin strain
- 5. icd 10 code for left flank pain
- 6. icd 10 code for broken right arm
- 7. icd 10 code for abscess to left finger
- 8. icd-10-pcs code for ct guided needle biopsy of an enlarged mediastinal mode
- 9. icd 10 code for periorbital cellulitis left
- 10. icd 10 code for conjunctivitistivitis