What are the new ICD 10 codes?
The new codes are for describing the infusion of tixagevimab and cilgavimab monoclonal antibody (code XW023X7), and the infusion of other new technology monoclonal antibody (code XW023Y7).
What is considered prediabetes A1C ICD 10?
Prediabetes
- R73.03 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM R73.03 became effective on October 1, 2021.
- This is the American ICD-10-CM version of R73.03 - other international versions of ICD-10 R73.03 may differ.
What is the ICD 10 code for morbid obesity?
Morbid (severe) obesity due to excess calories E66. 01 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2020 edition of ICD-10-CM E66. Likewise, what is the CPT code for obesity counseling? G0473 – face-to-face behavioral counseling for obesity, group (2–10), 30 minutes.
What is diabetes insipidus ICD 10 code?
what is diabetes insipidus icd 10 code 234. Destruction of beta-cells of the islets of Langerhans in the pancreas and consequently development of insulin-dependent diabetes is one ...
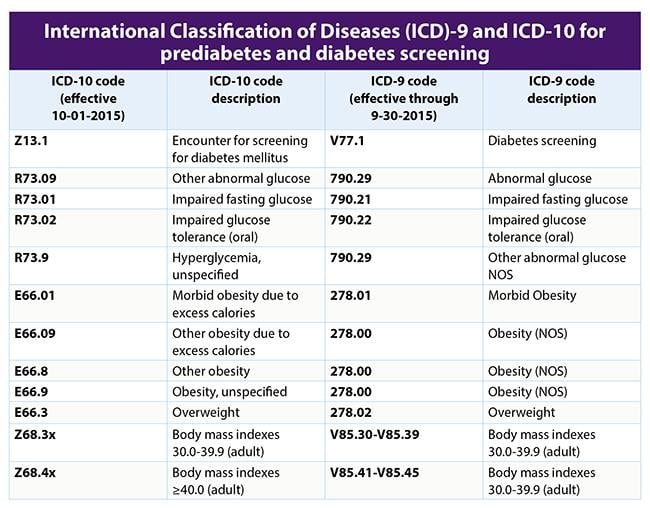
How do you code obesity in ICD-10?
Code E66* is the diagnosis code used for Overweight and Obesity. It is a disorder marked by an abnormally high, unhealthy amount of body fat. Excess body weight can come from fat, muscle, bone, and/or water retention.
What is the ICD-10 code for screening?
9.
What is the ICD-10 code Z13 89?
Code Z13. 89, encounter for screening for other disorder, is the ICD-10 code for depression screening.
Is Z71 3 a preventive code?
Obesity screening and counseling 01 (ICD-10- CM). The suggested coding for counseling for a healthy diet includes 99401-99404, 99411-99412, 99078, 97802-97804, G0447, S9452, S9470 as preventive with Z71. 3 (ICD-10-CM).
What does code Z12 11 mean?
A screening colonoscopy should be reported with the following International Classification of Diseases, 10th edition (ICD-10) codes: Z12. 11: Encounter for screening for malignant neoplasm of the colon.
What is the CPT code for weight check?
The CPT codes for obesity screening and counseling are CPT 99401, CPT 99402, CPT G0446, CPT G0447 & CPT G0473. Medicare does not allow the billing of other services performed on the same day as an obesity counseling.
What is Z13 40?
ICD-10 code Z13. 40 for Encounter for screening for unspecified developmental delays is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is code Z12 39?
39 (Encounter for other screening for malignant neoplasm of breast). Z12. 39 is the correct code to use when employing any other breast cancer screening technique (besides mammogram) and is generally used with breast MRIs.
When do you use Z13 31?
For instance, use ICD-10 code Z13. 31, “Encounter for screening for depression,” when screening for depression in patients at least 12 years old without reported symptoms. This is a preventive service defined under the Affordable Care Act and covered by many health plans.
What is the ICD-10 code for preventive care?
Z00. 00, Encounter for general adult medical examination without abnormal findings, Z00.
What are preventive ICD-10 codes?
“Routine” diagnosis codes are considered Preventive. For example: ICD-10-CM codes Z00. 121, Z00. 129, Z00.
Why is obesity increasing?
This may be due to physical inactivity, lack of exercise, eating habits, hereditary or stress. Number of obese patients are increasing day by day in the world.
What is the BMI for a 19 year old?
BMI for pediatric (2 to 19 years old) – Z68.51 to Z68.54. BMI can be coded even if it is documented by dietitian. But at the same time obesity or overweight should be documented by the treating provider. BMI codes (Z68) should only be coded when there is a diagnosis such as obesity, overweight, underweight etc.
Basics of Obesity Screening and Counseling
Obesity screening and counseling are one of a number of distinct preventive services mandated by national and state regulations (US Dept. of Labor). The U.S. Preventive Services Task Force (USPSTF) recommends screening all adults for obesity this screening also includes children of >6 years old.
Coverage for Medicare
For Medicare beneficiaries with obesity, who are competent and alert at the time that counseling is provided and whose counseling is furnished by a qualified primary care physician or other primary care practitioner and in a primary care setting, CMS covers:
Preventative Counseling (CPT 99401-9941)
The standard obesity medicine behavioral counseling codes are 99401-99412. These codes are used to report services for the purpose of promoting health and preventing illness. Typically, the 5-A’s approach i.e., ask, advise, assess, assist, and arrange is used.
Health Behavior Assessment and Intervention Codes (CPT 96156, 96158)
These codes are similar to preventative service counseling, but they deal more with specific behavioral problems often encountered in an obesity medicine practice.
When evaluating a patient for obesity and you also evaluate comorbidity conditions that you are treating or that
When evaluating a patient for obesity and you also evaluate comorbidity conditions that you are treating or that affect your treatment , you should report the additional diagnoses codes for those conditions you evaluated that affected this specific visit, linked to the appropriate evaluation and management (CPT) code. Unlike Facility services coding, where diagnosis-related groups (DRGs) are used to identify related conditions that may affect a patient’s care and are tied to reimburse-ment, payment for professional services is tied to CPT procedure codes.
What is preventive medicine evaluation?
Initial comprehensive preventive medicine evaluation and management of an individual, including an age and gender appropriate history, examination, counseling/anticipatory guidance/risk factor reduction interventions, and the ordering of laboratory/diagnostic procedures, established patient;
Does Medicare cover behavioral therapy for obesity?
For Medicare beneficiar ies with obesity, defined as a BMI greater than or equal to 30; who are competent and alert at the time that counseling is provided; and whose counseling is furnished by a qualified primary care physician or other primary care practitioner in a primary care setting, CMS will cover intensive behavioral therapy for obesity. This service is described as follows:
Importance of Obesity Management
- Obesity is associated with a wide range of medical problems such as increased risk for coronary heart disease, type 2 diabetes mellitus, various types of cancer, gallstones, and disability. HealthDay recently reported that the percentage of U.S. health spending on treatment of obesity-related illnesses in adults increased from just over 6 percent in 2001 to almost 8 percent in 201…
Definitions of Overweight and Obesity
- Body Mass Index (BMI) is calculated by dividing a person’s weight in kilograms by the square of the person’s height in meters, that is, BMI = weight/height2. In June 2017, the US Preventive Services Task Force (USPSTF) recommended clinicians screen for obesity in children and adolescents aged 6 years and older and offer or refer them to comprehensive, intensive behavio…
Body Mass Index Codes
- Category Z68 contains the ICD-10 codes to report BMI values. BMI adult codes are for use for persons 21 years of age or older and are based on the numerical scale (e.g., 28.0–28.9). Pediatric BMI codes are for use for persons 2-20 years of age and are based on the percentile for age range (e.g., 5th percentile to less than 85th percentile). The fou...
Points to Note
- When evaluating a patient for obesity, clinicians should also assess comorbidity conditions that is being treated or that affect the treatment, and report the additional diagnoses codes for those c...
- Medicare does not allow the billing of other services provided on the same day as an obesity counseling visit. However, commercial plans have a wide array of policies on such care, whic…
- When evaluating a patient for obesity, clinicians should also assess comorbidity conditions that is being treated or that affect the treatment, and report the additional diagnoses codes for those c...
- Medicare does not allow the billing of other services provided on the same day as an obesity counseling visit. However, commercial plans have a wide array of policies on such care, which differ as...
- Coding should be done to the highest degree of specificity. ICD-10 codes should be linked to the CPT codes on the claim.
- The codes assigned should represent an accurate description of “what” was performed and “why” it was performed and be supported by medical documentation, including time spent wit…
Popular Posts:
- 1. icd 10 code for closed nondisplaced fracture of triquetrum of left wrist
- 2. icd 10 code for m19.011
- 3. icd 10 code for hx of triple bypass surgery
- 4. icd 10 code for left proximal humeral shaft fracture
- 5. icd 9 code for neck abscess
- 6. icd 9 code for diabetic peripheral neuropathy
- 7. icd 10 code for neck pain with brachial plexus
- 8. icd 10 code for excision of skin lesion
- 9. icd 10 code for peg tube infection
- 10. icd-10 cm code for fracture/dislocation,right femur, with contusion right hip