What is ocular cicatricial pemphigoid?
Ocular Cicatricial Pemphigoid is abbreviated OCP. OCP is considered a subtype of Mucous Membrane Pemphigoid (abbreviated MMP), and these terms are sometimes used interchangeably. OCP is a type of autoimmune conjunctivitis that leads to cicatrization (i.e. scarring) of the conjunctiva.
What is the differential diagnosis for ocular conjunctivitis (OCP)?
The differential diagnosis of OCP is broad as it encompasses the differential for cicatricial conjunctivitis.
What are the confounders in the diagnosis of ocular mucosa medicamentosa (OCP)?
A common confounder to clinical diagnosis is medicamentosa, which results in a condition called pseudopemphigoid. Pseudopemphigoid is clinically identical to OCP but is caused by the long-term use of certain offending topical medications. Conjunctival biopsies may show linear staining of the conjunctival basement membrane zone.
What are the signs and symptoms of obstructive corneal polyangiitis (OCP)?
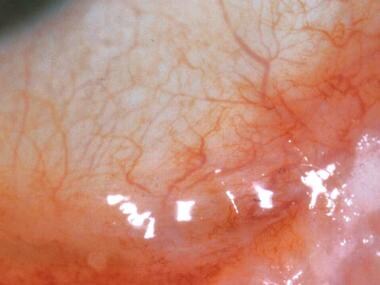
Symblepharon formation in the inferior fornix of a patient with OCP. May include nonspecific symptoms and minimal findings which lead to under-recognition of the disease. Commonly presents as chronic conjunctivitis, tear dysfunction, and subepithelial fibrosis.
What is ocular cicatricial pemphigoid?
Disease Entity. Ocular Cicatricial Pemphigoid is abbreviated OCP. OCP is considered a subtype of Mucous Membrane Pemphigoid (abbreviated MMP), and these terms are sometimes used interchangeably. OCP is a type of autoimmune conjunctivitis that leads to cicatrization (i.e. scarring) of the conjunctiva.
How common is ocular cicatricial pemphigoid?
Ocular cicatricial pemphigoid is present in about 60 to 70 percent of patients with mucous membrane pemphigoid.
What causes cicatricial pemphigoid?
The exact cause of mucous membrane pemphigoid is unknown. MMP is an autoimmune disorder. Autoimmune disorders are caused when the body's natural defenses (antibodies or immunoglobulins) against “foreign” or invading organisms (antigens) begin to attack healthy tissue for unknown reasons.
Can ocular cicatricial pemphigoid be cured?
There is no cure for pemphigoid but with proper long-term treatment and careful follow up it is usually possible to control the inflammation and the vision threatening side effects.
How is ocular cicatricial pemphigoid diagnosed?
Therefore, the clinical diagnosis of cicatricial pemphigoid is made when there is progression of a symblepharon without a history of local radiation or severe perennial allergic conjunctivitis. Diagnosis can be confirmed by conjunctival biopsy showing linear antibody deposition on the basement membrane.
Is ocular cicatricial pemphigoid painful?
Ocular Citatrical Pemphigoid/Mucous Membrane Pemphigoid Typical symptoms include redness, pain, tearing, and sensitivity to light. The inflammatory lesions on the ocular surface may result in scarring, loss of tear film, adhesions of the lids to the eyeball, corneal ulcers, and perforation.
What is the meaning of Cicatricial?
Medical Definition of cicatricial : relating to or having the character of a cicatrix excision of a cicatricial lesion.
What is the difference between pemphigus and pemphigoid?
Pemphigus is characterized by shallow ulcers or fragile blisters that break open quickly. Pemphigoid presents with stronger or “tense” blisters that don't open easily. Those with pemphigoid are also more likely to have hot, red and itchy hive spots.
Which is worse pemphigus and pemphigoid?
Pemphigus is a chronic and potentially fatal disease and patients should be counseled accordingly. Bullous pemphigoid is usually less severe and can resolve in 1 – 2 years.
How do you treat OCP?
The treatment of OCP involves the suppression of autoimmune conjunctival inflammation via the use of systemic immunomodulatory drugs. Conscientious ocular care to minimize the secondary consequences of chronic inflammation also is important.
How do you get pemphigoid?
Bullous pemphigoid is caused by a problem with the immune system (the body's defence against infection). Instead of attacking germs, it attacks and damages the skin. It's not known why this happens. Sometimes it's been linked to skin damage (such as sunburn) or taking certain medicines.
What causes OCP?
Ocular cicatricial pemphigoid (OCP) is a rare ocular surface disease usually due to an autoimmune reaction of the patient's body to the cells in the conjunctiva and eventually the cornea. It often begins with the feeling of dryness and irritation.
Is Cicatricial pemphigoid a genetic disorder?
A combination of environmental and genetic factors appear to play a role in the susceptibility of developing cicatricial pemphigoid.
How is OCP diagnosed?
The diagnosis is usually made during an office examination and can sometimes be confirmed by a small biopsy of the conjunctiva. Treatment of OCP generally involves eye lubrication and oral anti-inflammatory medications.
What causes OCP?
The cause of ocular cicatricial pemphigoid (OCP) is unknown. Genetic factors and several triggers can increase the likelihood of the onset of OCP. Individuals with HLA-DR2, HLA-DR4 (HLA-DR*0401), and HLA-DQw7 (DQB1*0301) are more susceptible to OCP.
How do you treat OCP?
The treatment of OCP involves the suppression of autoimmune conjunctival inflammation via the use of systemic immunomodulatory drugs. Conscientious ocular care to minimize the secondary consequences of chronic inflammation also is important.
The ICD code L121 is used to code Cicatricial pemphigoid
Cicatricial pemphigoid (also known as "Mucous Membrane Pemphigoid", "MMP", "Benign mucosal pemphigoid," "Benign mucous membrane pemphigoid," "Ocular pemphigus," and "Scarring pemphigoid") is a rare chronic autoimmune subepithelial blistering disease characterized by erosive skin lesions of the mucous membranes and skin that results in scarring of at least some sites of involvement.:581.
Coding Notes for L12.1 Info for medical coders on how to properly use this ICD-10 code
Inclusion Terms are a list of concepts for which a specific code is used. The list of Inclusion Terms is useful for determining the correct code in some cases, but the list is not necessarily exhaustive.
ICD-10-CM Alphabetical Index References for 'L12.1 - Cicatricial pemphigoid'
The ICD-10-CM Alphabetical Index links the below-listed medical terms to the ICD code L12.1. Click on any term below to browse the alphabetical index.
Equivalent ICD-9 Codes GENERAL EQUIVALENCE MAPPINGS (GEM)
This is the official approximate match mapping between ICD9 and ICD10, as provided by the General Equivalency mapping crosswalk. This means that while there is no exact mapping between this ICD10 code L12.1 and a single ICD9 code, 694.61 is an approximate match for comparison and conversion purposes.
What is the treatment for ocular cicatricial pemphigoid?
Treatments include topical/local therapies, systemic medications, minor procedures, and surgical intervention when necessary.
What is the medical management strategy for ocular cicatricial pemphigoid?
The medical management strategy for ocular cicatricial pemphigoid is to control inflammation and halt the progression of fibrosis. Treatments include topical/local therapies, systemic medications, minor procedures, and surgical intervention when necessary.
How many people go blind due to cicatricial pemphigoid?
Several studies show that between 25% to 30% of patients progress to blindness due to the pathophysiology leading up to and including corneal opacification.[5] Ocular cicatricial pemphigoid is a lifelong disease that requires follow up care, even when in remission.
What is the best way to diagnose cicatricial pemphigoid?
Conjunctival biopsy with direct immunofluorescence (DIF) is the most reliable method and the gold standard to confirm the ocular cicatricial pemphigoid diagnosis. About 20% to 40% of patients may have clinical signs of ocular cicatricial pemphigoid but may, in fact, have a negative biopsy result. [4],[5],[6]This does not rule out the diagnosis of ocular cicatricial pemphigoid even with a broad and complex differential diagnosis. These patients most likely only have ocular disease, as a positive result is more common in those with ocular, skin, and oral disease. Negative results may be due to the biopsy technique, concurrent quiescence, or even disease burnout.[5] When positive, the results show a linear deposition of IgG, IgA, and sometimes IgM and complement 3 proteins in the epithelial basement membrane zone.[5] Autoantibodies against antigen sites within the basement membrane are rarely detected, even in those patients with a positive biopsy. [5]
How old is a cicatricial pemphigoid?
Ocular cicatricial pemphigoid predominantly affects females (2:1 over males), and the age of onset is around 60 years of age or older. There is no racial predilection. Ocular cicatricial pemphigoid is considered a rare disease, and incidence is estimated to be about 1 per 10,000 to 50,000. [1]
What is OCP in medical terms?
Ocular cicatricial pemphigoid (OCP) is a form of mucous membrane pemphigoid (MMP) that features chronic, relapsing-remitting bilateral conjunctivitis. Ultimately, patients affected by this autoimmune disease will experience conjunctival cicatrization or scarring. If patients do not receive treatment or do not respond to treatment, they will develop corneal opacification and permanent vision loss. Ocular cicatricial pemphigoid is present in about 60 to 70 percent of patients with mucous membrane pemphigoid. This activity reviews the evaluation and management of ocular cicatricial pemphigoid and highlights the role of the interprofessional team in caring for affected individuals.
What are the signs of conjunctivitis?
Early on in the disease, the conjunctiva exhibits the following signs: diffuse hyperemia, papillary reaction, dry eye syndrome, and keratoconjunctivitis sicca due to the destruction of goblet cells. Intermediate stages of the disease are notable for subconjunctival fibrosis and shortening of the inferior fornix. This is most often found when patients are diagnosed. Later on, as the disease progresses, the symblephara develop and there is flattening of the plica and keratinization of the caruncle.
How many cases of cicatricial conjunctivitis are there?
Incidence rates are vary between 1 in 12,000 to 60,000. A study in the UK found that OCP represents 61% of cicatricial conjunctivitis and is estimated to occur with an incidence of 1 in 1 million.
What is differential diagnosis of OCP?
The differential diagnosis of OCP is broad as it encompasses the differential for cicatricial conjunctivitis. The differential includes infectious etiologies such as trachoma, inflammatory etiologies such as rosacea, autoimmune etiologies such as linear IgA disease, Graft Versus Host Disease (GVHD), and Stevens Johnson Syndrome (SJS), allergic etiologies such as atopy, conjunctival trauma, chemical burns, medicamentosa, radiation, and neoplasia.
What is the OCP?
OCP is a type of autoimmune conjunctivitis that leads to cicatrization (i.e. scarring) of the conjunctiva. If OCP is left untreated, it can lead to blindness.
What is OCP in a patient?
OCP is a type of autoimmune conjunctivitis that leads to cicatrization (i.e. scarring) of the conjunctiva. If OCP is left untreated, it can lead to blindness.
How much Dapsone should I take for OCP?
Dapsone is started at a dose of 50 mg/day and slowly increased as tolerated by up to 25mg every 7 days to an effective dose, which is usually between 100-200mg/day. If significant improvement is not achieved within 3 months, escalation of therapy is recommended such as to azathioprine or methotrexate.
Is IL-13 elevated in OCP?
Several pro-inflammatory cytokines are found to be elevated in the conjunctival tissues of patients with OCP. Levels of Interleukin (IL) 1, Tumor Necrosis Factor (TNF) Alpha, migration inhibition factor, and macrophage colony-stimulating factor, and IL-13 have been found to be elevated. IL-13 has been found to have a pro-fibrotic and pro-inflammatory effect on conjunctival fibroblasts, and may be implicated in the progressive conjunctival fibrosis that can occur despite clinical quiescence.
Is a biopsy of the conjunctiva necessary?
Diagnosis is based on clinical signs and positive direct immunofluorescence testing of the conjunctiva. Conjunctival biopsy of an actively involved area is needed and the conjunctival tissue must be submitted unfixed for analysis. If involvement is diffuse, biopsy of the inferior conjunctival fornix is recommended. Judicious biopsy is advisable as OCP is an obliterating disease of the conjunctiva and only the minimal amount of tissue necessary should be removed. Alternatively, biopsy of an active oral mucosa lesion can be diagnostic as well.

Popular Posts:
- 1. icd 10 code for large retroperitoneal hematoma
- 2. icd 10 code for gerd in pediatrics
- 3. icd 10 code for left pes planus
- 4. icd 10 code for painful menstrual periods
- 5. icd 9 code for sore fingers
- 6. icd 10 code for nodular opacities middle lobe
- 7. icd 10 code for nerve stimulator device status
- 8. icd 9 code for unspecified allergic reaction
- 9. icd 10 code for primary osteoarthritis of both knees
- 10. icd 10 code for g93.41