These codes are used for new patients (99201, 99202, 99203) and established patients (99211, 99212, 99213) when treated in an office and/or outpatient setting. There also are preventive medicine codes that may be used to report the preventive medical evaluation of infants, children and adults.
What does initial office visit mean?
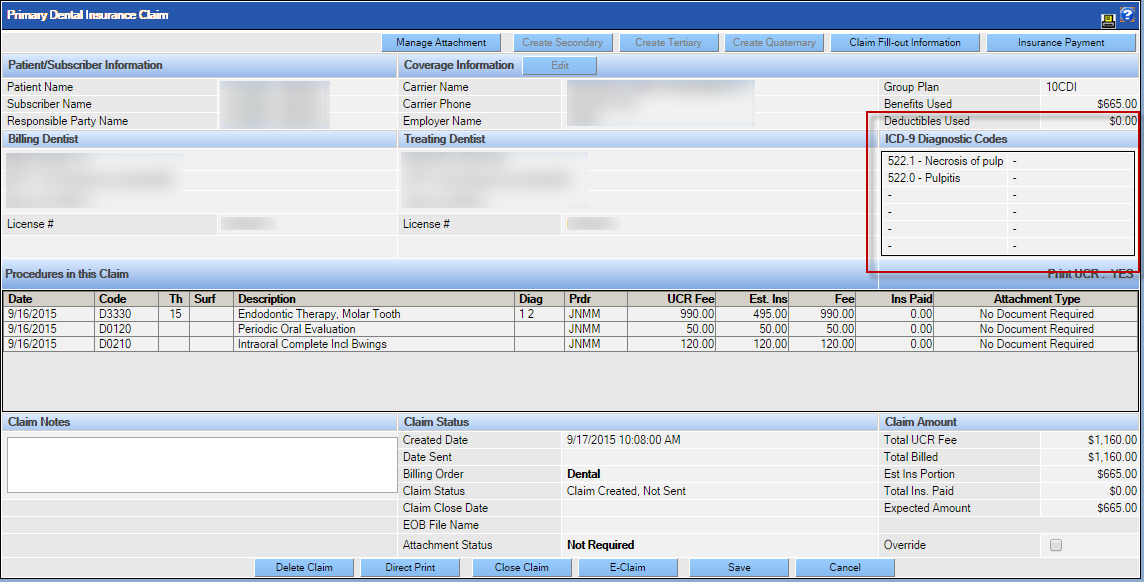
Oct 01, 2021 · Z01.89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z01.89 became effective on October 1, 2021. This is the American ICD-10-CM version of Z01.89 - other international versions of ICD-10 Z01.89 may differ.
What is the longest ICD 10 code?
Oct 01, 2021 · Z00.00 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. Short description: Encntr for general adult medical exam w/o abnormal findings. The 2022 edition of ICD-10-CM Z00.00 became effective on …
Where can one find ICD 10 diagnosis codes?
Choosing an E&M code based on time New patients Established patients (seen in the last 3 years) 99201 doesn't exist anymore 99211 - minimal problem that may not require the presence of a provider 99202 - straightforward MDM, 15 29 minutes 99212 - straightforward MDM, 10 19 minutes 99203 - low level of MDM, 30 44 minutes 99213 - low level MDM, 20 29 minutes 99204 …
How many ICD 10 codes are there?
CPT 99211, 99212, 99213, 99214, 99215 – Established patient office visit. CPT 99211 Office or other outpatient visit for the evaluation and management of an established patient, that may not require the presence of a physician or other qualified health care professional. Usually, the presenting problem (s) are minimal.
What is the diagnosis code for office visit?
Z02. 9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z02. 9 became effective on October 1, 2021.
What is the CPT code for established patient office visit?
What is the code and the charge for office visit established?
What is the code for an established patient?
| History | Medical decision making | |
|---|---|---|
| 99212 | Problem-focused | Straightforward |
| 99213 | Expanded problem-focused | Low |
| 99214 | Detailed | Moderate |
| 99215 | Comprehensive | High |
How do you code patient visits?
...
Typical times for established patient office visits.
| CPT code | Typical time |
|---|---|
| 99212 | 10 minutes |
| 99213 | 15 minutes |
| 99214 | 25 minutes |
| 99215 | 40 minutes |
What is code 99213 used for?
What is office visit in medical billing?
What is EST PT Level 3?
What is established patient level 3?
What is the only difference between new patient and established patient office visit codes?
What is considered a new patient vs established patient?
What is an establish care visit?
What is the CPT code for a physician's office visit?
A physician performed a visit that met the definition of an office visit CPT code 99213 and the total duration of the direct face-to-face services (including the visit) was 65 minutes. The physician bills CPT code 99213 and one unit of code 99354.
What is the CPT code for a domiciliary visit?
A physician performed a visit that met the definition of a domiciliary, rest home care visit CPT code 99327 and the total duration of the direct face-to-face contact (including the visit) was 140 minutes. The physician bills CPT codes 99327, 99 354, and one unit of code 99355.
What is 99211 office?
99211 Office or other outpatient visit for the evaluation and management of an established patient that may not require the presence of a physician. Usually the presenting problem (s) are minimal. Typically, five minutes are spent performing or supervising these services.
What are preoperative and postoperative billing errors?
Preoperative and postoperative billing errors occur when E&M services are billed with surgical procedures during their preoperative and postoperative periods. ClaimCheck bases the preoperative and postoperative periods on designations in the CMS National Physician Fee Schedule. For example, if a provider submits procedure code 99212 (Office or other outpatient visit for the evaluation and management of an established patient, which requires at least 2 of these 3 key components: A problem focused history; A problem focused examination; Straightforward medical decision making [10 minutes]) with a DOS of 11/02/08 and procedure 27750 (Closed treatment of tibial shaft fracture [with or without fibular fracture]; without manipulation) with a DOS of 11/03/08, ClaimCheck will deny procedure code 99212 as a preoperative visit because it is submitted with a DOS one day prior to the DOS for procedure code 27750.#N#Services Provided by Ancillary Providers
What is the CPT code for a physician?
The physician bills CPT code 99215 and one unit of code 99354. ?
How long is a 99213 visit?
A physician performed a visit that met the definition of code 99213 and, while the patient was in the office receiving treatment for 4 hours, the total duration of the direct face-to-face service of the physician was 40 minutes.
What is the billing code 99213?
This code is a piece of a group of therapeutic charging codes depicted by the numbers Medical billing code 99213 speaks to the center (level 3) office or other outpatient set up office patient visit and is a piece of the Healthcare Common Procedure Coding System (HCPCS). This technique code address for built up office patient visits is a piece of a complete arrangement of CPT® addresses composed without anyone else. I am a board affirmed inner solution doctor with more than ten years of clinical hospitalist involvement in a group hospitalist project giving doctor administrations to a vast local healing center framework. I have composed my accumulation of assessment and administration (E/M) addresses throughout the years to help doctors and other non-doctor professionals (medical caretaker experts, clinical attendant masters, confirmed medical caretaker birthing specialists and doctor partners) comprehend the unpredictable and obsolete universe of healing facility and center based coding prerequisites.
Do you include staff time on a visit?
Do not include any staff time or time spent on any days before or after the visit. This allows clinicians to capture the work when a significant amount of it takes place before or after the visit with the patient, and to bill for it on the day of the visit.
How long does a physician spend with a patient?
Physicians typically spend 20 minutes face-to-face with the patient and/or family. CPT code 99203: Office or other outpatient visit for the evaluation and management of a new patient, which requires these 3 key components: A detailed history; A detailed examination; Medical decision making of low complexity.
Does history count toward level of service?
History and exam don’t count toward level of service. Physicians, advanced practice registered nurses, and physician assistants won’t use history or exam to select what level of code to bill for office visits 99202–99215, as they did in the past. They need only document a medically appropriate history and exam.
What is CPT code 99214?
Learn how to correctly bill CPT Code 99214 instead CPT 99213 or CPT 99212 Codes for Evaluation and Management (E&M) Coding of Established Office Patient to increase revenue through legitimate Medicare reimbursement.
What is a new patient?
A new patient is one who has not received any professional services from the physician/qualified health care professional or another physician/qualified health care professional of the exact same specialty and subspecialty who belongs to the same group practice, within the past three years.
How long does a physician have to spend in a face to face scenario?
The physician, if using time as a factor must have spent at least 25 minutes in a face to face scenario with the patient. However, the time component is only a guide and not completely required if the components are included in the visit and the required medical necessity is present.
What is the E/M code for outpatient visits?
Some of the most commonly reported E/M codes are 99201-99215, which represent office or other outpatient visits. In 2020, the E/M codes for office and outpatient visits include patient history, clinical examination, and medical decision-making as the key components for determining the correct code level, and that is the version ...
Is 99201 99215 a minor procedure?
The rules related to reporting 99201-99215 on the same date as a minor procedure are confusing for many coders. You need to understand which services the payer considers separately reportable.
What is the difference between 99211 and 99211?
Code 99211 differs from the other office visit codes in that it does not require the 3 key components. In addition, the code descriptor specifies that the visit may not require the presence of a physician or other qualified healthcare professional:
Can you select an E/M code based on time?
Selecting an office/outpatient E/M code based on the key components is not the only option available. CPT ® and Medicare guidelines also allow you to select from these E/M codes based on time.
What does modifier 25 mean in Medicare?
The National Correct Coding Initiative (NCCI) Policy Manual for Medicare Services, Chapter 1, states that providers also may submit a distinct E/M code with modifier 25 on the same date as a code that has an XXX global indicator. The XXX indicator means the global concept does not apply to the code.
Is E/M coding medical necessity?
No discussion of E/M coding would be complete without mentioning medical necessity. In all cases, whether a visit involves a new or established patient, medical necessity should determine the extent of the service provided, including elements like the history, exam, and MDM. Consequently, medical necessity determines the final E/M code choice.
When to report E/M?
If a physician performs an E/M service on the same date as a major procedure or on the day before the procedure, you may report the E/M separately if the E/M resulted in the decision for surgery. You should append modifier 57 Decision for surgery to the E/M service code in this case.
Popular Posts:
- 1. icd 10 cm code for pre syncope
- 2. icd 10 code for right atrial mass
- 3. icd 10 cm code for scrotal abscess.
- 4. icd 10 code for skin cancer on nose
- 5. icd 10 code for benign prostatic hyperplasia
- 6. icd 10 code for infected left hip
- 7. icd-10 code for necrotizing fasciitis
- 8. icd-10 procedure code for iv fluids
- 9. icd 10 code for pregnancy with hypertension
- 10. icd 10 cm code for urinary and fecal incomplete