What is the ICD 10 code for sequela of stroke?
Sequela of Stroke – Other deficits ICD-10-CM code ICD-10-CM description I69.30 Unspecified sequela of cerebral infarction I69.31-Cognitive deficits following cerebral infarction Add 6th character for specific cognitive deficit separation I69.320 Aphasia following cerebral infarction I69.321 Dysphasia following cerebral infarction
What is the ICD 10 code for stroke and Tia?
STROKE ICD-10 coding tables for stroke cont’d Acute codes for Stroke/TIA ICD-10-CM code ICD-10-CM description Definition and tip I63.6 Cerebral infarction due to cerebral venous thrombosis, non-pyrogenic I63.8 Other cerebral infarction I63.9 Cerebral infarction unspecified Stroke NOS G45.9 Transient Ischemic Attack, unspecified TIA
What is the ICD-10 code for history of stroke?
› History of stroke (ICD-10 code Z86.73) should be used when there are no identifiable manifestations of the acute stroke, a diagnosis of transient ischemic attack [TIA] was made, or the stroke no longer has a specific treatment plan,
What is the ICD 10 code for CVA with no late effects?
PART 1: ICD 10 Code for CVA with No Late Effects – Video The quick answer is, you have a couple choices, and the couple choices is you can code it as a history, Z86.73, or you can code it as unspecified sequelae I69.30.
What is the ICD-10 code for history of CVA with residual effects?
Other sequelae of cerebral infarction The 2022 edition of ICD-10-CM I69. 398 became effective on October 1, 2021. This is the American ICD-10-CM version of I69. 398 - other international versions of ICD-10 I69.
What is the ICD-10 code for sequela of CVA?
ICD-10 code I69. 3 for Sequelae of cerebral infarction is a medical classification as listed by WHO under the range - Diseases of the circulatory system .
How do you code history of stroke?
Personal history of transient ischemic attack (TIA), and cerebral infarction without residual deficits. Z86. 73 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z86.
When should you code history of stroke?
Once the patient is discharged, it is not appropriate to code for the cerebral infarction. Instead, you would code any and all residual deficits the patient has. If the patient does not have any cerebral infarction deficits, you can apply the ICD-10 code Z86.
What is the ICD-10 code for history of stroke?
73 for Personal history of transient ischemic attack (TIA), and cerebral infarction without residual deficits is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is stroke sequela?
Sequelae are residual effects or conditions produced after the acute phase of an illness or injury has ended. Therefore there is no time limit on when a sequela code can be assigned. Residuals may be apparent early on such as in cerebral infarction, or they can occur months or years later.....
How do you code stroke in ICD-10?
1. Acute Ischemic Stroke (ICD-10 code I63.
What is prior stroke?
The warning signs of stroke include: Weakness or numbness of the face, arm or leg, usually on one side of the body. Trouble speaking or understanding. Problems with vision, such as dimness or loss of vision in one or both eyes. Dizziness or problems with balance or coordination.
What is late effect of stroke?
Right-sided weakness or paralysis and sensory impairment. Problems with speech and understanding language (aphasia) Visual problems, including the inability to see the right visual field of each eye. Impaired ability to do math or to organize, reason, and analyze items.
What is diagnosis code r079?
ICD-9 Code Transition: 786.5 Code R07. 9 is the diagnosis code used for Chest Pain, Unspecified. Chest pain may be a symptom of a number of serious disorders and is, in general, considered a medical emergency.
What should I ask about history of stroke?
Due to the nature of TIAs and strokes, it can be useful to first ask some simple questions, such as the patient's age, the month and what they believe your job role to be....Course“Have the symptoms improved since they first began?”“When were your symptoms at their worst?”“Are the symptoms coming and going?”
What is the most important information in stroke patient history?
The most important initial question to clarify with the patient, family, or witness is the stroke onset time and the patient's “last seen normal time,” as it starts the clock on eligibility for acute treatment, i.e., thrombolytic therapy with tPA and/or endovascular therapy.
How do you code CVA and hemiparesis in sequela?
Coding Guidelines Residual neurological effects of a stroke or cerebrovascular accident (CVA) should be documented using CPT category I69 codes indicating sequelae of cerebrovascular disease. Codes I60-67 specify hemiplegia, hemiparesis, and monoplegia and identify whether the dominant or nondominant side is affected.
Is a cerebral infarction the same as a stroke?
A cerebral infarction (also known as a stroke) refers to damage to tissues in the brain due to a loss of oxygen to the area. The mention of "arteriosclerotic cerebrovascular disease" refers to arteriosclerosis, or "hardening of the arteries" that supply oxygen-containing blood to the brain.
PART 1: ICD 10 Code for CVA with No Late Effects – Video
The quick answer is, you have a couple choices, and the couple choices is you can code it as a history, Z86.73, or you can code it as unspecified sequelae I69.30. Now, the long answer; when you look at those two codes, always err on the side of caution here, but let’s look at this and read them.
PART 2: What is a CVA – Video
Now, in ICD-10 it is very specific.
What is Category I69?
The thing that gets you here is this comment: Category I69, which is the CVA area , is to be used to indicate conditions between this range, I60-I67, as causes of the sequelae. The ‘sequelae’ include conditions specified as such or as residual which may occur at any time after the onset of the causal condition. Again, I’m inclined to say we’ve got a Z code here, a history code, but without all of the documentation. You really can’t make a clear statement that this is the code.
What does TIA mean in CVA?
What about the TIA, people get CVA and TIA confused. Well, a TIA it’s just a little mini-stroke, what it actually means is it kind of temporary. There’s been a blockage, there’s been a problem with the blood flow but it doesn’t usually let tissue die. We think of heart tissue as dying when a person has a heart attack.
How long does a TIA last?
Here we’ve got a little brain attack in the vascular system and it usually can last from like a minute up to 24 hours they said, not usually 24 hours, and sometimes the side effects go away before they even get to the doctor, but it’s still important you need to go. So, that is coded different, that is a G code, G45.9 is kind of a catch all, is a TIA not otherwise specified. Do know that they both can have side effects, residuals. Just summing it up, then that’s the end of the answer sheet. So, ask yourself: Is this the history? And they could have had, just because it says recent doesn’t mean that’s different. That shouldn’t change your way of thinking. You use the information given to you and there are no side effects. And, is that the reason they’re staying at the facility? Maybe they’re just returning after treatment. So, I hope that answers your questions, it was really fun to look into this…
Why do they code I63?
If you’re going to code an I63 code, then the guidelines tell you because there’s this new treatment called this tPA. What it is they get there soon enough. They can give you this injection of this tPA or this treatment that thins out the blood, and what could be a massive horrible stroke can almost, not be reversed but the residual and late effects could be gone. And so, this is very important; and therefore, they want to know: Was this used? If it was, you better code it because it makes a difference in the
How to sign up for CCO forum?
To Sign Up for the New Forum, click here: https://www.cco.us/cco-forum/
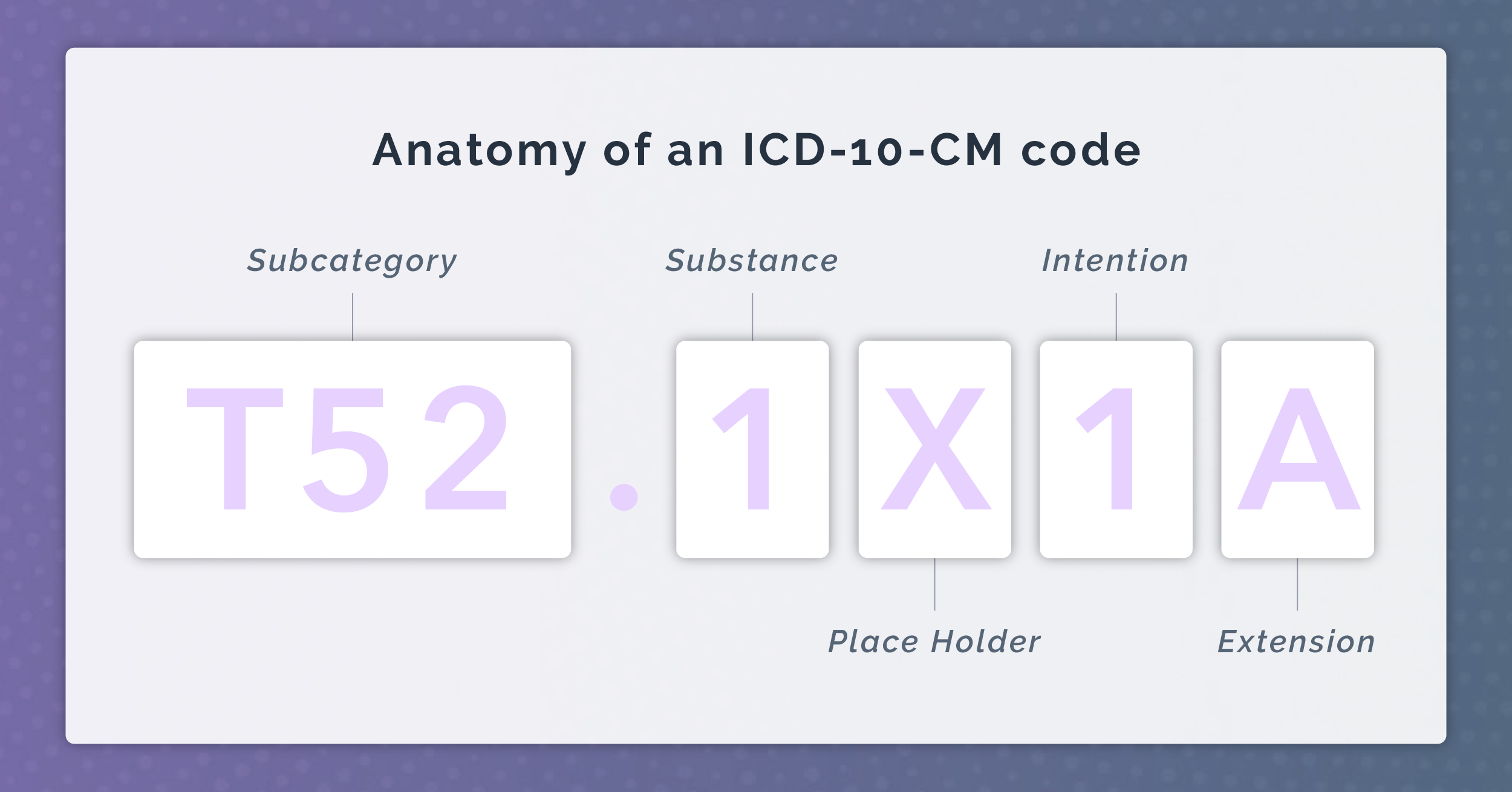
Is ICd 10 specific?
Now, in ICD-10 it is very specific. I even went on and I took it off because I gave you all the list of all of these codes due to this and that, and ultimately is it an embolism? Is it a thrombosis? What part of the vascular system inside the brain, the lining of the brain, all of that in there, but you don’t need to know that to answer this question.
What is the ICD-10 code for stroke?
In ICD-10 CM, code category I63 should be utilized when the medical documentation indicates that an infarction or stroke has occurred. Coding of sequelae of stroke and infarction also demands a level of detail often missing in medical records. There are specific codes which indicate the cause of the infarction, such as embolism or thrombosis, as well as the specific affected arteries. The sixth digit provides additional information which designates the affected side when applicable.
How to code a stroke?
Seek answers to two questions when coding a stroke, infarction, or hemorrhage. First, ask if the cerebral event is acute, or emergent. Second, find in the medical record details of the site and the site, laterality, and type of stroke or infarction. Medical record documentation should clearly specify the cause-and-effect relationship between the medical intervention and the cerebrovascular accident in order to assign a code for an intraoperative or postprocedural cerebrovascular accident.
What is Z86.73?
If a patient has a history of a past cerebrovascular event and has no residual sequelae, report Z86.73 Personal history of transient ischemic attack (TIA ), and cerebral infarction without residual deficits.
What is the ICD-10 code for cerebral infarction?
The patient is admitted into hospital and diagnosed with cerebral infarction, unspecified ( ICD-10 code I63.9). At the 3-week post-discharge follow-up appointment for the cerebral infarction, the office visit note states the patient had a stroke and has a residual deficit of hemiplegia, affecting the right dominant side.
What are the risk factors for stroke?
Also code any documented atrial fibrillation, CAD, diabetes, or hypertension as these comorbidities are stroke risk factors.
When to report neurological deficits?
Report any and all neurological deficits of a cerebrovascular accident that are exhibited anytime during a hospitalization, even if the deficits resolve before the patient is released from the hospital.
Is unilateral weakness a symptom of stroke?
Documentation of unilateral weakness in conjunction with a stroke is considered by the ICD to be hemiparesis/hemiplegia due to the stroke and should be reported separately. Hemiparesis is not considered a normal sign or symptom of stroke and is always reported separately. If the patient’s dominant side is not documented, ...
What is the ICD-10 code for stroke?
Explicitly document findings to support diagnoses of › Stroke sequela codes (ICD-10 category I69.-) should acute stroke, stroke and subsequent sequela of be used at the time of an ambulatory care visit stroke, and personal history of stroke without sequela, oce, which is considered subsequent to any acute
What is the term for a stroke that occurs when there is disruption of blood flow to brain tissue?
stroke occurs when there is disruption of blood flow to brain tissue, this leads to ischemia (deprivation of oxygen) and potentially infarction (dysfunctional scar tissue). Strokes can be either hemorrhagic, or embolic/thrombotic. Hemorrhagic strokes occur as a result of a ruptured cerebral blood vessel. Embolic/thrombic strokes occur as a result of an obstructed cerebral vessel.
What percentage of stroke cases have a Z86 code?
Conversely, 99.7 percent did not have evidence of acute strokes. The findings stated that 285 of 580 (49.1 percent) of enrollees actually had a “history of stroke” diagnosis and should have had a Z86.- code. The financial differential between erroneously falling into HCC 100 (acute ischemic stroke) versus no HCC for a personal history was reportedly $1,826 (from the Centers for Medicare & Medicaid Services/CMS to the MA organization for the transferred enrollee). In 16 of 580 cases (2.8 percent), the sequela of hemiplegia (15 of 16, 93.4 percent) or monoplegia (1of 16, 6.6 percent) was determined to be present, and CMS credited the MA organizations with underpayments.
What is a HCC?
Hierarchical Condition Categories (HCCs) are also calculated according to the provider documentation of the patient’s medical issues (as is the DRG assignment). If HCC capture is done from a non-curated problem list, GIGO (garbage in, garbage out). The problem list grows longer and longer if no one is deleting and assigning end dates appropriately. No one has perpetual acute appendicitis. They undergo an appendectomy, and the appendicitis is eradicated. Acute appendicitis should then fall off the record.
What is the etiology of a CVA?
First, you must indicate what the etiology of the cerebrovascular accident (CVA) is (e.g., non-traumatic subarachnoid, intracerebral, subdural, or epidural hemorrhage or cerebral infarction). Then, the specificity, especially for cerebral infarction, is unwieldy. Maximal granularity includes whether a cerebral infarction occurs due ...
What is the code for a stroke?
After the acute incident has resolved, the patient either has neurological deficits (residua or sequelae) or they do not. The latter is coded with Z86.73, Personal history of transient ischemic attack (TIA) and cerebral infarction without residual deficits, or Z86.79, Personal history of other diseases of the circulatory system, for history of brain bleeds. If there are deficits, and the provider makes the necessary linkage, a “sequelae of” code should be assigned signifying the specific residua.
Why don't providers resolve diagnoses?
They refer to chronic conditions as “ (past medical) history of (e.g., heart failure),” and they don’t resolve diagnoses because they don’t even know that “personal history of” is an option.
Does a stroke count as a HCC?
An acute stroke today has HCC implications for next year, because it is a prospective model. If the year goes from Jan. 1 to Dec. 31, a stroke on Jan. 2 counts for the entire subsequent year (not the year in which the stroke occurred). After the acute incident, the provider should precisely and correctly transition to a sequelae of cerebrovascular disease or a Z86 code. Certain sequelae, such hemi- or monoplegia, have risk-adjusting implications. In fact, motor residua are even more risk-adjusting than acute stroke. There is only a nullification hierarchy between hemiplegia/hemiparesis (HCC 103) and monoplegia and other paralytic syndromes (HCC 104). Acute stroke and risk-adjusting sequelae will have additive risk adjustment factors (RAFs).
How much did Medicare overpay for strokes?
The essence was that beneficiaries who transitioned from traditional Medicare to Medicare Advantage (MA) came with inappropriate acute stroke codes affixed to their risk factor scores, resulting in approximately $14 million of extrapolated overpayments. Documentation of strokes is tricky.

Popular Posts:
- 1. icd 10 code for large adrenal mass
- 2. icd 10 code for pulmonary valve stenosis with insufficiency.
- 3. icd 10 code for chronic migraine without aura
- 4. icd 10 code for primary open angle glaucoma severe stage
- 5. icd 10 cm code for decreased exercise tolerance
- 6. 2047 icd 10 code for enthesophyte at the distal achilles tendon left foot
- 7. icd 10 code for failed back syndrome lumbar
- 8. icd 10 dx code for prediabetes
- 9. icd code for digital rectal examination quizlet
- 10. icd 9 code for dislocation of radius and ulna