How do you find ICD-10-CM codes?
ICD-10 CM Guidelines, may be found at the following website: https://www.cdc.gov/nchs/icd/icd10cm.htm.Dec 1, 2021
How are ICD-10 codes organized?
ICD-10-CM is a seven-character, alphanumeric code. Each code begins with a letter, and that letter is followed by two numbers. The first three characters of ICD-10-CM are the “category.” The category describes the general type of the injury or disease. The category is followed by a decimal point and the subcategory.
When coding a diagnosis What comes first?
Etiology/Manifestation. Coding conventions require the condition be sequenced first followed by the manifestation. Wherever such a combination exists, there is a “code first” note with the manifestation code and a “use additional code” note with the etiology code in ICD-10.
What are some common ICD-10 codes?
Top 10 Outpatient Diagnoses at Hospitals by Volume, 2018RankICD-10 CodeNumber of Diagnoses1.Z12317,875,1192.I105,405,7273.Z233,219,5864.Z00003,132,4636 more rows
What does "type 1 excludes" mean?
A type 1 excludes note is a pure excludes. It means "not coded here". A type 1 excludes note indicates that the code excluded should never be used at the same time as U07.1.
What does the title of a manifestation code mean?
In most cases the manifestation codes will have in the code title, "in diseases classified elsewhere.". Codes with this title are a component of the etiology/manifestation convention. The code title indicates that it is a manifestation code.
What is the code for a carrier of infectious disease?
Carrier or suspected carrier of infectious disease - instead, use code Z22. -. Infectious and parasitic diseases complicating pregnancy, childbirth and the puerperium - instead, use code O98.-. Infectious and parasitic diseases specific to the perinatal period - instead, use Section P35-P39.
What does "type 2 excludes" mean?
Type-2 Excludes. Type-2 Excludes means the excluded conditions are different, although they may appear similar. A patient may have both conditions, but one does not include the other. Excludes 2 means "not coded here.". Carrier or suspected carrier of infectious disease - instead, use code Z22.-. Infectious and parasitic diseases complicating ...
What does excludes2 mean?
An excludes2 note indicates that the condition excluded is not part of the condition it is excluded from but a patient may have both conditions at the same time. When an Excludes2 note appears under a code it is acceptable to use both the code and the excluded code together.
What is type 1 excludes?
An Excludes1 is used when two conditions cannot occur together , such as a congenital form versus an acquired form of the same condition .
What is the difference between ICD-10 and CM?
The ICD-10-CM has two types of excludes notes. Each note has a different definition for use but they are both similar in that they indicate that codes excluded from each other are independent of each other.
How many characters are in a placeholder X?
For codes less than 6 characters that require a 7th character a placeholder X should be assigned for all characters less than 6. The 7th character must always be the 7th character of a code.
What is the 10th revision of the ICD-10?
The International Classification of Diseases, 10th Revision (ICD-10) is the official system to assign health care codes describing diagnoses and procedures in the United States (U.S). The ICD is also used to code and classify mortality data from death certificates.
When was ICD-10-CM implemented?
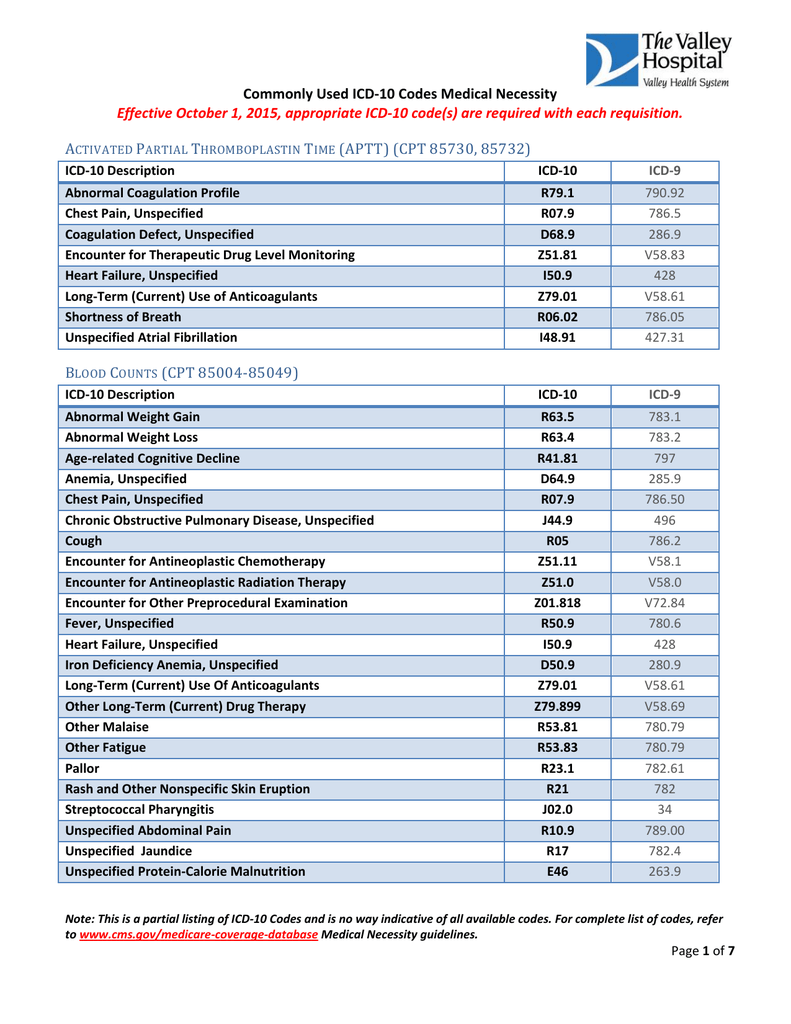
ICD-10 was implemented on October 1, 2015, replacing the 9th revision of ICD (ICD-9).
Do SLPs have to report ICD-10 codes?
SLPs practic ing in a health care setting, especially a hospital, may have to code disease s and diagnoses according to the ICD-10. Payers, including Medicare, Medicaid, and commercial insurers, also require SLPs to report ICD-10 codes on health care claims for payment.
General Information
CPT codes, descriptions and other data only are copyright 2021 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, §1833 (e) states that no payment shall be made to any provider for any claim which lacks the necessary information to process the claim.
Article Guidance
The information in this article contains billing, coding or other guidelines that complement the Local Coverage Determination (LCD) for Continuous Peripheral Nerve Blocks (CPNB) L37641.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
Popular Posts:
- 1. icd 10 code for acute prostatitis due to e. coli
- 2. icd 10 code for laceration left ringer finger
- 3. icd 10 code for refusal of vaccine
- 4. icd 10 code for encounter for monoclonal antibodies
- 5. icd-9-cm code for acute perforated peptic ulcer
- 6. icd 10 code for bronchitis acute
- 7. icd 10 cm code for lump on right side of face
- 8. icd 10 cm code for cancer history lung
- 9. icd 10 code for psa free and total
- 10. what is the icd 10 code for kepra levels