What is the ICD 10 code for post op pain?
The code is paired with a nerve block such as 64415 for post op pain. The dx codes we use for both are ex; G89.18 & M75.101 (acute post procedural pain and chronic rotator cuff tear right shoulder). Any thoughts on dx code that would better pair with the 76942-26.
What is the ICD 10 code for severe pain?
What is the ICD 10 code for severe pain? Pain, unspecified . R52 is a billable /specific ICD -10- CM code that can be used to indicate a diagnosis for reimbursement purposes.
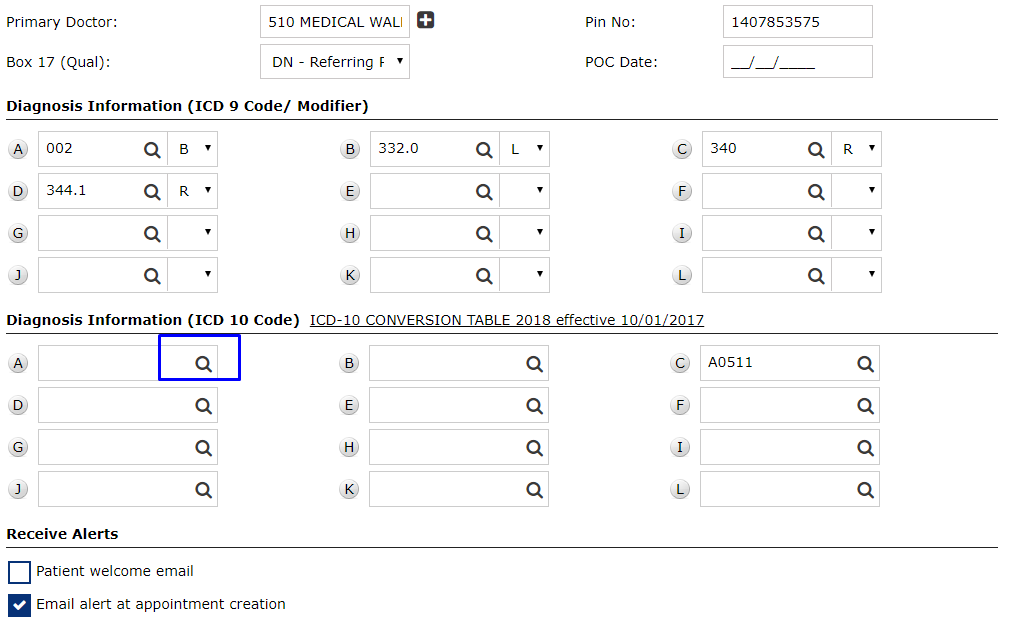
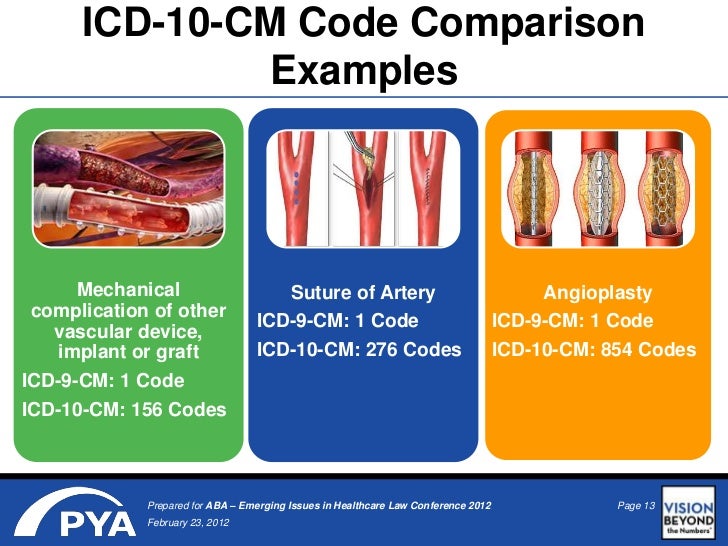
What is diagnosis code 10?
- Similar to the diagnosis code set, the alpha characters in ICD 10 code sets are not case-sensitive.
- The letters “O” and “I” are not in the code set. ...
- The 7 characters in the procedure code set help in providing very precise details. ...
- The fourth character identifies the part of the body. ...
What is the ICD 10 code for surgery?
§The ICD-10-PCS (procedure code), if utilized to map the resident into a surgical clinical category, must be recorded on the second line of item I8000. PT and OT Components Major Joint Replacement or Spinal Surgery ICD-10-CM Code Description
How do you code post op pain?
Coding Guidelines for Pain338.0, Central pain syndrome.338.11, Acute pain due to trauma.338.12, Acute post-thoracotomy pain.338.18, Other acute postoperative pain.338.19, Other acute pain.338.21, Chronic pain due to trauma.338.22, Chronic post-thoracotomy pain.338.28, Other chronic postoperative pain.More items...
What is the ICD-10 code for Post op abdominal pain?
18: Other acute postprocedural pain.
What is the ICD-10 code for surgical wound?
ICD-10 Code for Disruption of external operation (surgical) wound, not elsewhere classified, initial encounter- T81. 31XA- Codify by AAPC.
What is the ICD 9 code for postoperative pain?
Other chronic post-operative pain: ICD-9-CM Code 338.
What is acute postoperative pain?
Postoperative pain can be divided into acute pain and chronic pain. Acute pain is experienced immediately after surgery (up to 7 days) and pain which lasts more than 3 months after the injury is considered to be chronic pain.
When do you use ICD-10 code G89 29?
ICD-10 code G89. 29 for Other chronic pain is a medical classification as listed by WHO under the range - Diseases of the nervous system .
How do you code a non-healing surgical wound?
998.83 - Non-healing surgical wound. ICD-10-CM.
When do you use z48 01?
01 for Encounter for change or removal of surgical wound dressing is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is the ICD 10 code for post operative wound infection?
ICD-10 Code for Infection following a procedure- T81. 4- Codify by AAPC.
When do you code acute pain due to trauma?
ICD-10-CM Code for Acute pain due to trauma G89. 11.
What is the code for pain?
The ICD-10-CM Index indicates that pain NOS is reported with code R52 (Pain, unspecified).
When do you code chronic pain?
You may report the acute/chronic pain code (G89) as a secondary diagnosis if the diagnosis provides additional, relevant information not adequately explained by the primary diagnosis code.
What is disruption of surgical wound?
Wound dehiscence is a surgery complication where the incision, a cut made during a surgical procedure, reopens. It is sometimes called wound breakdown, wound disruption, or wound separation. Partial dehiscence means that the edges of an incision have pulled apart in one or more small areas.
What is dehiscence wound?
Dehiscence is a partial or total separation of previously approximated wound edges, due to a failure of proper wound healing. This scenario typically occurs 5 to 8 days following surgery when healing is still in the early stages.
How do you code wound dehiscence?
code 12020 (Treatment of superficial wound dehiscence; simple closure), which has a global period of 10 days, or. code 13160 (Secondary closure of surgical wound or dehiscence; extensive or complicated), which has a 90-day global period.
What is the ICD 10 code for wound dehiscence?
Wound dehiscence under the ICD-10-CM is coded T81. 3 which exclusively pertains to disruption of a wound not elsewhere classified. The purpose of this distinction is to rule out other potential wound-related complications that are categorized elsewhere in the ICD-10-CM.
What is the code for postoperative pain?
Postoperative pain not associated with a specific postoperative complication is reported with a code from Category G89, Pain not elsewhere classified, in Chapter 6, Diseases of the Nervous System and Sense Organs. There are four codes related to postoperative pain, including:
What is code assignment in coding?
The key elements to remember when coding complications of care are the following: Code assignment is based on the provider’s documentation of the relationship between the condition and the medical care or procedure.
Is postoperative pain normal?
Determining whether to report postoperative pain as an additional diagnosis is dependent on the documentation, which, again, must indicate that the pain is not normal or routine for the procedure if an additional code is used. If the documentation supports a diagnosis of non-routine, severe or excessive pain following a procedure, it then also must be determined whether the postoperative pain is occurring due to a complication of the procedure – which also must be documented clearly. Only then can the correct codes be assigned.
Is postoperative pain a part of recovery?
Postoperative pain typically is considered a normal part of the recovery process following most forms of surgery. Such pain often can be controlled using typical measures such as pre-operative, non-steroidal, anti-inflammatory medications; local anesthetics injected into the operative wound prior to suturing; postoperative analgesics;
Is post thoracotomy pain acute or chronic?
If the documentation does not specify whether the post-thoracotomy or post-procedural pain is acute or chronic, the default is acute.
Is postoperative pain a reportable condition?
Only when postoperative pain is documented to present beyond what is routine and expected for the relevant surgical procedure is it a reportable diagnosis. Postoperative pain that is not considered routine or expected further is classified by whether the pain is associated with a specific, documented postoperative complication.
What is the secondary code for Chapter 20?
Use secondary code (s) from Chapter 20, External causes of morbidity, to indicate cause of injury. Codes within the T section that include the external cause do not require an additional external cause code. Type 1 Excludes.
When will the ICd 10 T85.848A be released?
The 2022 edition of ICD-10-CM T85.848A became effective on October 1, 2021.
What is the ICd 10 code for pain?
The ICD-10-CM Official Guidelines for Coding and Reporting provide extensive notes and instruction for coding pain (category G89). Review these guidelines in full. The following summary identifies key points.#N#When seeking a pain diagnosis, identify as precisely as possible the pain’s location and/or source. If pain is the primary symptom and you know the location, the Alphabetic Index generally will provide all the information you need.#N#Only report pain diagnosis codes from the G89 category as the primary diagnosis when: 1 The acute or chronic pain and neoplasm pain provide more detail when used with codes from other categories; or 2 The reason for the service is for pain control or pain management.
How long does pain last?
Acute pain is sudden and sharp. It can range from mild to severe and may last a few minutes or a few months. Acute pain typically does not last longer than six months and usually disappears when the physician identifies and treats the underlying cause or condition. Chronic pain may last for months or years, and may persist even after the underlying injury has healed or the underlying condition has been treated. There is no specific timeframe identifying when you can define the pain as chronic. Determine the code assignment based on provider documentation.
Can you report G89 as a primary diagnosis?
Do not report codes from category G89 as the first-listed diagnosis if you know the underlying (definitive) diagnosis and the reason for the service is to manage/treat the underlying condition. You may report the acute/chronic pain code (G89) as a secondary diagnosis if the diagnosis provides additional, relevant information not adequately explained by the primary diagnosis code.
What is the ICd 10 code for pain?
The ICD-10-CM Index indicates that pain NOS is reported with code R52 (Pain, unspecified). However, reimbursement for this vague code is likely to be problematic, so try to obtain a more specific diagnosis whenever possible.
What is the code for abdominal pain?
In addition to the codes for pain in the various parts of the abdomen, there are codes for: Acute abdomen (R10.0): This is sudden, severe abdominal pain, often accompanied by rigidity of the abdomen.
What is the G89 code?
For example, you can assign a G89 code to indicate that the pain is acute or chronic. You should assign the site-specific pain code first unless the purpose of the encounter is pain management, in which case the G89 code is first. For example, a patient is referred for ankle x-rays for chronic right ankle pain.
What is a pain that does not point to a specific body system?
Pain that does not point to a specific body system is classified in the Symptoms and Signs chapter. For example, abdominal pain is classified to category R10. Certain specific types of pain are classified to category G89 (Pain, not elsewhere classified) in the Nervous System chapter.
Why do radiologists order pain studies?
Many imaging studies are ordered because the patient is experiencing pain. Once ICD-10 is implemented on October 1 of next year, radiology coders will need to be ready to assign the appropriate codes for these studies. In this article we’ll give you a run-down of how pain is classified in ICD-10, as well as the rules for sequencing the pain codes.
What is R10.81?
Abdominal tenderness (R10.81-): Tenderness is abnormal sensitivity to touch. While pain is a symptom that the patient reports, tenderness is a reaction that the physician observes while examining the patient’s abdomen.
What does R07.1 mean?
Chest pain on breathing (R07.1): This type of pain can be a sign of pulmonary embolism.
When will the ICD-10 T81.89XA be released?
The 2022 edition of ICD-10-CM T81.89XA became effective on October 1, 2021.
What is the secondary code for Chapter 20?
Use secondary code (s) from Chapter 20, External causes of morbidity, to indicate cause of injury. Codes within the T section that include the external cause do not require an additional external cause code. Type 1 Excludes.
What is the 5th character of the ICD-10 operative procedure code assigned by a medical coder?
The hysterectomy procedure approach (5th character of the ICD-10 operative procedure code assigned by a medical coder) identifies whether an abdominal incision was made and determines if the procedure is categorized as a NHSN HYST or VHYS.
What is NHSN operative procedure code?
The NHSN operative procedure code documents, posted on the NHSN site, are not intended to be instructive to medical coders for assigning procedure codes to surgical procedures. The documents are provided as a tool to assist NHSN users participating in SSI reporting with categorizing operative procedures by NHSN procedure categories and to standardize the reporting of surgical procedures between facilities.
How often are NHSN codes updated?
NHSN operative procedure codes are reviewed and updated annually and as needed.
Where to find NHSN procedure code?
Procedure code documents of past years are found on the NHSN Data Validation’s web page in the “Resources” section for the respective year.
Is the scope of a procedure code a four or a four?
If the fifth character of the ICD-10-PCS procedure code is a four (4) or F, then the field for scope should be YES.
Is a distal shunt replacement a revision?
Within the ICD-9 code system there were specific revision codes for procedures that involved distal shunt replacement or revision of the distal catheter, there are no codes within the ICD-10-PCS code system that are specific for this type of procedure.
What is the secondary code for Chapter 20?
Use secondary code (s) from Chapter 20, External causes of morbidity, to indicate cause of injury. Codes within the T section that include the external cause do not require an additional external cause code. Type 1 Excludes.
When will the ICD-10-CM T82.847A be released?
The 2022 edition of ICD-10-CM T82.847A became effective on October 1, 2021.
Popular Posts:
- 1. what is the icd-10-cm code for dm with neuropathy
- 2. what is the icd 10 code for overactive bladder
- 3. icd 10 code for abdominal seroma capsule
- 4. icd 10 code for low o2 sat
- 5. icd 10 code for lightheadedness unspecified
- 6. icd 10 code for edema both legs
- 7. what is the icd 10 code for dry eyes
- 8. icd 10 code for labor with delivery eminent
- 9. icd-10 code for annual physical labs
- 10. icd 9 code for j tube status