What is paradoxical vocal cord movement?
About PVFM PVFM happens when your vocal folds close when they should open. When you take a breath, your vocal folds should open to let air through to your lungs. With PVFM, your vocal folds close part way or all the way. This can make it hard to breathe. PVFM does not happen all the time.
Is paradoxical vocal fold motion a voice disorder?
Ear nose and throat doctors refer to this disorder as “paradoxical vocal fold motion disorder” or PVFMD. Lung doctors (pulmonologists) often refer to this disorder as “vocal cord dysfunction” or VCD. These terms are interchangeable and refer to the same disorder.
What is the major difference between asthma and paradoxical vocal fold motion disorder?
VCD is sometimes confused with asthma because some of the symptoms are similar. In asthma, the airways (bronchial tubes) tighten, making breathing difficult. With VCD, the vocal cord muscles tighten, which also makes breathing difficult. Unlike asthma, VCD is not an allergic response starting in the immune system.
Is Laryngospasm the same as vocal cord dysfunction?
Laryngospasm, a subtype of vocal cord dysfunction, is a brief involuntary spasm of the vocal cords that often produces aphonia and acute respiratory distress. Laryngospasm is a common complication of anesthesia.
What do patients with paradoxical vocal fold motion PVFM typically complain of?
Paradoxical Vocal Fold Motion Disorder Symptoms, Signs, and Diagnosis. Patients with PVFM often report symptoms of increased difficulty with inhalation, feeling as if the throat is tightening or closing off, and a sound (stridor) with inhalation.
How do you fix paradoxical vocal cord dysfunction?
Speech therapy is usually the first treatment for PVCD. Often it is enough to correct the disorder. Other professionals such as psychologists may also be involved in the treatment. Speech therapy focuses on decreasing tension in the larynx by helping patients focus on exhaling rather than inhaling.
When I cough my throat closes up and I can't breathe?
Laryngospasm is a frightening condition that happens when your vocal cords suddenly seize up, making breathing more difficult. This rare phenomenon is often a symptom of an underlying condition. If you've had recurring laryngospasms, you should see your healthcare provider to find out what's causing them.
What is exercise induced vocal cord dysfunction?
Vocal cord dysfunction (also known as exercise-induced laryngeal obstruction) is a common condition characterized by the throat inexplicably closing during rigorous exercise. It can dramatically increase breathing difficulty, diminish performance and often causes panic in those who experience it.
Do asthma inhalers affect vocal cords?
Yes, some asthma inhalers, especially Advair, can cause irritation or inflammation of the vocal cords, he said.
What is a vocal cord spasm?
Laryngospasm (luh-RING-go-spaz-um) is a transient and reversible spasm of the vocal cords that temporarily makes it difficult to speak or breathe. The vocal cords are two fibrous bands inside the voice box (larynx) at the top of the windpipe (trachea).
What is similar to laryngospasm?
Several studies have established that paroxysmal laryngospasm is often secondary to laryngopharyngeal reflux, a variant of gastroesophageal reflux disease (GERD). Paroxysmal laryngospasm is often misdiagnosed as asthma, hysterical stridor, obstructive sleep apnea, paroxysmal nocturnal dyspnea, and other conditions [7].
What is the first action for laryngospasm?
Attempt manual ventilation while continuing to apply continuous positive airway pressure (CPAP). Attempt to break the laryngospasm by applying painful inward and anterior pressure at 'Larson's point' bilaterally while performing a jaw thrust.
What are the symptoms of vocal cord dysfunction?
What are the symptoms of vocal cord dysfunction?Throat or chest tightness.Noisy inhalation.Difficulty getting air "in"Feeling of throat closing.Feeling of being "strangled"Intermittent shortness of breath.Chronic cough.Voice change/Inability to speak.
What kind of doctor do you see for vocal cord dysfunction?
Vocal cord dysfunction is treated by an ear, nose, and throat doctor (ENT, also called an otolaryngologist), a pulmonologist, and a speech therapist. They work together to help the child learn to relax the vocal cords while breathing. Treatment for vocal cord dysfunction may also include: practicing breathing exercises.
Does anxiety cause vocal cord dysfunction?
Stress, posttraumatic stress disorder (PTSD), anxiety, depression and panic attacks have all been linked to episodes of vocal cord dysfunction. Anxiety is more likely to trigger an episode in kids and teenagers than adults.
Can anxiety cause Laryngospasm?
Emotional responses like stress and anxiety can trigger laryngospasm. It's your body's physical response to an intense emotion that you're feeling. Sleep-related laryngospasm. Some people experience laryngospasm in their sleep and wake up gasping for air.
Who demonstrates a simulated period of laryngospasm on a website accessible by searching for?
Dr. Bastian demonstrates a simulated period of laryngospasm on a website accessible by searching for "laryngospasm and bastian"
What is a VCD?
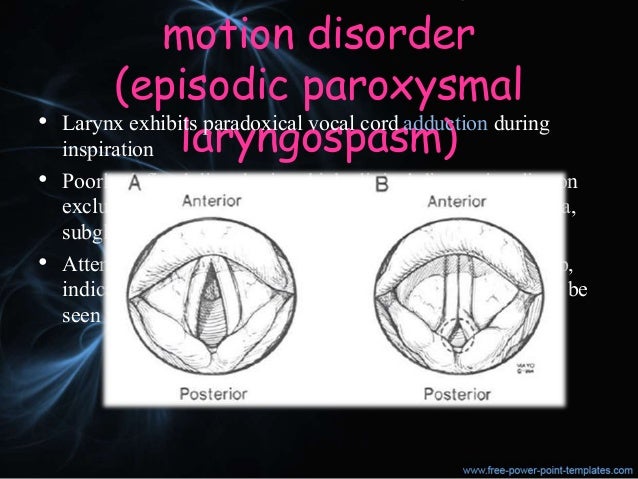
VCD defined as "a paradoxical movement of the vocal cords' - with a hyperfunctional laryngeal reflex which results in adduction (coming together) of the vocal cords with resultant airflow limitation (Porsbjerg 2017, Kenn 2012)
What is somatoform disorder?
Somatoform disorders are psychological difficulties with symptoms of a physical disorder unexplained by a medical condition. Conversion or somatization disorder (more common) unconsciously produced deficit in motor or sensory functioning, always preceded by a psychological stressor; females>males.
Do beta antagonists respond to medical therapy?
Attacks typically do not respond to medical therapy targetted to reactive airway disease (beta antagonists)
Is PVCM a psychological disorder?
As per Forrest et al (Forrest 2012) Although PVCM (paradoxical vocal cord motion) may be a psychological disorder, there are different forms which they divided into "primary, or psychological, and secondary" - with the secondary form consists of medical disorders divided into irritable larynx syndrome and neurologic disorders.
Can laryngeal dystonia cause airway obstruction?
Severe airway obstruction as in the case depicted below of a laryngeal dystonia may be associated with life-threatening airway obstruction and may warrant tracheotomy
What is the term for the movement of the vocal folds?
Paradoxical Vocal Fold Movement (PVFM) Paradoxical vocal fold movement, or PVFM, makes it hard to breathe or talk. It does not happen all of the time but can cause serious problems when it does happen. Children and adults can have PVFM. Speech-language pathologists, or SLPs, can help.
What can a SLP do to help with vocal folds?
The SLP can teach you exercises that help keep your vocal folds open when you breathe and when PVFM happens . See information for professionals on ASHA’s Practice Portal pages on Voice Disorders and Aerodigestive Disorders.
What is vocal cord dysfunction?
Vocal cord dysfunction or paradoxical vocal fold motion (PVFM) is an episodic condition that results when vocal cord movement is dysfunctional. We open our vocal cords when we breathe, and we close them when we speak, sing, swallow or lift heavy items. Vocal cord dysfunction describes what is occurring when our vocal cords close when we intended them to open to breathe. This incorrect vocal cord motion causes an abnormal narrowing of the voice box. The voice box narrowing leaves only a small opening for air to flow through the vocal cords, which can result in a sensation of difficulty moving air into or out of the lungs.
How long does it take to cure vocal cord dysfunction?
Therapy generally requires two to six 60-minute sessions . These sessions aim to:
Why does my voice box narrow?
The voice box narrowing leaves only a small opening for air to flow through the vocal cords, which can result in a sensation of difficulty moving air into or out of the lungs. People who suffer PVFM episodes often have a very sensitive or reactive airway. Common triggers include: Acid reflux. Exercise.
Can vocal cord dysfunction cause asthma?
Cough or fumes. Vocal cord dysfunction is sometimes misdiagnosed as asthma because the symptoms and triggers for PVFM and asthma can be similar. The difference between PVFM and asthma is that if you have asthma, medicines that open your breathing tubes (bronchodilators such as albuterol) will improve your breathing.
How to diagnose vocal cord paralysis?
Vocal cord paralysis is usually diagnosed by an otolaryngologist (NIDCD, 1999). Noting the symptoms the patient has experienced, the otolaryngologist will ask how and when the voice problems started in order to help determine their cause. Next, the otolaryngologist listens carefully to the patient's voice to identify breathiness or harshness. Then, using an endoscope, the otolaryngologist looks directly into the throat at the vocal cords. A speech-language pathologist may also use an acoustic spectrograph, an instrument that measures voice frequency and clarity, to study the patient's voice and document its strengths and weaknesses.
How to treat paralyzed vocal cords?
Treating people who have 2 paralyzed vocal cords may involve performing a surgical procedure called a tracheotomy to help breathing (NIDCD, 1999). In a tracheotomy, an incision is made in the front of the patient's neck and a breathing tube (tracheotomy tube) is inserted through a hole, called a stoma, into the trachea. Rather than breathing through the nose and mouth, the patient now breathes through the tube. Following surgery, the patient may need therapy with a speech-language pathologist to learn how to care for the breathing tube properly and how to reuse the voice.
How long do vocal cord nodules last?
If nothing is done to change vocal abuse habits, vocal cord nodules can last a lifetime, and may even recur after surgical removal. With proper voice training with a certified therapist, nodules can disappear with 6 to 10 voice therapy sessions over 6 to 12 weeks.
What is the role of minimizing voice use in a patient?
Patients are taught to be succinct when speaking, to avoid any loud use of the voice, to keep phone calls brief and to avoid all non-speech voice use (throat clearing, coughing, "voiced" sneezing, crying, "voiced" laughing, and odd sound-effects).
How to treat voice nodules in children?
Treatment for nodules that do not resolve with voice therapy involves surgical removal of the nodules at direct laryngoscopy and correction of the underlying voice abuse. Vocal nodules in children usually regress with voice therapy alone.
What are vocal cord nodules?
Vocal cord nodules (singer's nodules) are small, hard, callus like growths that usually appear singly on the vocal cord (Merck, 1997). Nodules consist of condensations of hyaline connective tissue in the lamina propria at the junction of the anterior 1/3 and posterior 2/3 of the free edges of the true vocal cords. Vocal cord polyps are small, soft growths that usually appear singly on a vocal cord. They are most often caused by vocal abuse or long-term exposure to irritants, such as chemical fumes or cigarette smoke.
What is the procedure to add bulk to a paralyzed vocal cord?
Surgery involves adding bulk to the paralyzed vocal cord or changing its position (NIDCD, 1999). To add bulk, an otolaryngologist injects a substance, commonly Teflon, into the paralyzed cord. Other substances currently used are collagen, silicone, and body fat. The added bulk reduces the space between the vocal cords so the non-paralyzed cord can make closer contact with the paralyzed cord and thus improve the voice.
What is paradoxical vocal fold motion?
Paradoxical vocal fold motion (PVFM), also called paradoxical vocal cord dysfunction, is a breathing disorder characterised by approximation rather than abduction/opening of the vocal folds during inspiration. This can result in upper-airway obstruction and stridor. [1]#N#Andrianopoulos MV, Gallivan GJ, Gallivan KH. PVCM, PVCD, EPL, and irritable larynx syndrome: what are we talking about and how do we treat it? J Voice. 2000;14:607-618. http://www.ncbi.nlm.nih.gov/pubmed/11130117?tool=bestpractice.com#N#[2]#N#Maschka DA, Bauman NM, McCray PB Jr, et al. A classification scheme for paradoxical vocal cord motion. Laryngoscope. 1997;107:1429-1435. http://www.ncbi.nlm.nih.gov/pubmed/9369385?tool=bestpractice.com#N#[3]#N#Mathers-Schmidt BA. Paradoxical vocal fold motion: a tutorial on a complex disorder and the speech-language pathologist's role. Am J Speech Lang Pathol. 2001;10:111-125.#N#[4]#N#Al-Alwan A, Kaminsky D. Vocal cord dysfunction in athletes: clinical presentation and review of the literature. Phys Sportsmed. 2012;40:22-27. http://www.ncbi.nlm.nih.gov/pubmed/22759602?tool=bestpractice.com#N#[5]#N#Patel RR, Venediktov R, Schooling T, et al. Evidence-based systematic review: effects of speech-language pathology treatment for individuals with paradoxical vocal fold motion. Am J Speech Lang Pathol. 2015;24:566-584. http://www.ncbi.nlm.nih.gov/pubmed/25836980?tool=bestpractice.com#N#Diagnosis is most often based upon exclusion of other differentials.
What is breathing disorder?
Summary. Breathing disorder that is frequently mistaken for asthma. Accurate diagnosis is made by a multi-disciplinary team, which can include a speech language pathologist, a primary care physician, an asthma/allergy specialist, a pulmonologist, a psychologist, a psychiatrist, a sports medicine specialist, an athletic trainer, ...
What is paradoxical vocal fold motion?
Paradoxical vocal fold motion (PVFM) is a disorder often misdiagnosed in children presenting with shortness of breath and stridor. In infants, little is known about the clinical course and best approach for treatment of PVFM. This retrospective study assesses the approach to treatment and outcomes for infants with PVFM.
What is the adduction of vocal folds during inspiration?
Paradoxical vocal fold motion (PVFM), also known as vocal cord dysfunction (VCD), is the untimely adduction of vocal cords during inspiration resulting in obstruction at the level of the glottis. The width of the rima glottides, the space between vocal folds, is determined largely by vocal fold movement thereby determining air flow through the glottic aperture. During inspiration, the posterior cricoarytenoid muscle contracts resulting in abduction of vocal folds and widening of the rima glottides, while during expiration contracture of the lateral cricoarytenoid results in adduction of vocal folds and narrowing of the rima glottides. In PVFM, there is aberrant adduction of vocal folds during the act of inspiration [ 1, 2 ]. On visualization of the vocal cords, there is a characteristic, yet uncommon, finding of adduction of the anterior two-thirds with a diamond-shaped gap or “chink” in the posterior aspect of the vocal folds [ 3, 4 ]. Clinically, this manifests as resulting dyspnea and noisy breathing in the form of stridor.
Can PVFM be diagnosed in infants?
PVFM can be challenging to diagnose in the infant population. PVFM resolves uneventfully with reflux treatment, however, it is unknown whether reflux treatment is essential or if PVFM would spontaneously resolve. The rarity of infantile PVFM mandates formal evaluation and monitoring by a pediatric otolaryngologist.
About PVFM
- PVFM happens when your vocal folds close when they should open. When you take a breath, your vocal folds should open to let air through to your lungs. With PVFM, your vocal folds close part way or all the way. This can make it hard to breathe. PVFM does not happen all the time. You may not have any other problems with your vocal folds except when P...
Signs and Symptoms of PVFM
- PVFM can cause breathing problems. Some people will need to go to the hospital if they are having a lot of difficulty breathing. People with PVFM may be told that they have asthma. But PVFM is not asthma. It is a problem with how and when the vocal folds move. Here are some symptoms you might have when PVFM happens: 1. coughing 2. rough-sounding voice 3. difficult…
Causes of PVFM
- The exact cause of PVFM is not known, but it may be triggered by 1. acid reflux, 2. exercise, 3. breathing in cold air, 4. smoke or pollen, and/or 5. emotional stress.
Seeing A Professional
- Testing for PVFM
You will probably see a team of professionals to find out if you have PVFM. The SLP is an important member of the team. Other members may include the following: 1. allergist 2. pulmonologist 3. otolaryngologist (ear, nose, and throat doctor) 4. gastroenterologist 5. neurolo… - Treatments for PVFM
The goal of treatment for PVFM is to make sure your vocal folds open normally and stay open while you are breathing. You also will become aware of what triggers PVFM so you can avoid those triggers. You may need medical treatment for PVFM if you have a medical condition—like …
Other Resources
Popular Posts:
- 1. 2015 icd 10 code for pancreatic cancer
- 2. icd 10 code for right shoulder biceps tenodesis
- 3. icd 10 code for history of thyroid disorder
- 4. icd 10 cm code for r finger got sucked up
- 5. icd 10 code for ocyoconycisis
- 6. icd 10 code for thoracic spine pain
- 7. what is the correct icd 10 code for fetal demise
- 8. icd-10 code for anemia due to vitamin b12 intrinsic factor deficiency
- 9. icd 9 code for fungal dermititis
- 10. icd 10 code for tooth absecss