What is the ICD 10 code for perianal ulcer?
K62. 6 - Ulcer of anus and rectum | ICD-10-CM.
Can Z76 89 be used as a primary diagnosis?
The patient's primary diagnostic code is the most important. Assuming the patient's primary diagnostic code is Z76. 89, look in the list below to see which MDC's "Assignment of Diagnosis Codes" is first. That is the MDC that the patient will be grouped into.
What is the ICD 10 code for stoma?
ICD-10 code Z93. 3 for Colostomy status is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is the ICD 10 code for ulceration?
Non-pressure chronic ulcer of skin of other sites with unspecified severity. L98. 499 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM L98.
What is diagnosis code Z71 89?
Other specified counselingICD-10 code Z71. 89 for Other specified counseling is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
Is Z76 89 a billable code?
Z76. 89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is the ICD-10 PCS code for colostomy?
2022 ICD-10-PCS Procedure Code 0D1L0Z4: Bypass Transverse Colon to Cutaneous, Open Approach.
What is the ICD 10 code for colostomy complication?
K94.0ICD-10 code K94. 0 for Colostomy complications is a medical classification as listed by WHO under the range - Diseases of the digestive system .
How do you code a colostomy?
You should report CPT code 44146 (see Table 1). Although the CPT descriptor includes the term “colostomy,” the Medicare physician fee schedule work relative value unit (RVU) for this code is based on creation of either a colostomy or an ileostomy.
What is the ICD 10 code for non healing ulcer?
Non-pressure chronic ulcer of skin of other sites limited to breakdown of skin. L98. 491 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM L98.
What are non-pressure ulcers?
The term “non-pressure ulcer” was coined to designate a primary mechanism other than shear or pressure. If there is poor circulation, such as that caused by venous or arterial insufficiency or excessive moisture or trauma, a patient may develop a non-pressure ulcer.
What is the ICD 10 code for non healing surgical wound?
998.83 - Non-healing surgical wound is a topic covered in the ICD-10-CM.
Can you bill for establishing care?
You can't code or bill a service that is performed solely for the purpose of meeting a patient and creating a medical record at a new practice.
What is the ICD-10 code for annual physical exam?
Z00.00ICD-10 Code for Encounter for general adult medical examination without abnormal findings- Z00. 00- Codify by AAPC.
What does obesity unspecified mean?
Having a high amount of body fat (body mass index [bmi] of 30 or more). Having a high amount of body fat. A person is considered obese if they have a body mass index (bmi) of 30 or more.
What is the ICD-10 code for referral to specialist?
Encounter for other administrative examinations The 2022 edition of ICD-10-CM Z02. 89 became effective on October 1, 2021. This is the American ICD-10-CM version of Z02.
What is a peptic ulcer?
Peptic ulcer, site unspecified, unspecified as acute or chronic, without hemorrhage or perforation 1 K00-K95#N#2021 ICD-10-CM Range K00-K95#N#Diseases of the digestive system#N#Type 2 Excludes#N#certain conditions originating in the perinatal period ( P04 - P96)#N#certain infectious and parasitic diseases ( A00-B99)#N#complications of pregnancy, childbirth and the puerperium ( O00-O9A)#N#congenital malformations, deformations and chromosomal abnormalities ( Q00-Q99)#N#endocrine, nutritional and metabolic diseases ( E00 - E88)#N#injury, poisoning and certain other consequences of external causes ( S00-T88)#N#neoplasms ( C00-D49)#N#symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified ( R00 - R94)#N#Diseases of the digestive system 2 K20-K31#N#2021 ICD-10-CM Range K20-K31#N#Diseases of esophagus, stomach and duodenum#N#Type 2 Excludes#N#hiatus hernia ( K44.-)#N#Diseases of esophagus, stomach and duodenum 3 K27#N#ICD-10-CM Diagnosis Code K27#N#Peptic ulcer, site unspecified#N#2016 2017 2018 2019 2020 2021 Non-Billable/Non-Specific Code#N#Includes#N#gastroduodenal ulcer NOS#N#peptic ulcer NOS#N#Type 1 Excludes#N#peptic ulcer of newborn ( P78.82)#N#Use Additional#N#code to identify:#N#alcohol abuse and dependence ( F10.-)#N#Peptic ulcer, site unspecified
When will the ICD-10-CM K27.9 be released?
The 2022 edition of ICD-10-CM K27.9 became effective on October 1, 2021.
Why do we put skin barriers around the stoma?
As part of the pouching process, solid skin barriers are placed around the stoma to protect the underlying skin from detrimental components of the stoma output ( urine or stool). These barriers work to keep the skin dry by absorbing both effluent from the stoma and moisture from the underlying skin. If too much moisture is absorbed from ...
How to treat periwound moisture dermatitis?
Manage wound exudate with dressings chosen for proper absorbency. Apply a barrier film or skin protectant to the periwound skin when appropriate. The first step in treatment of periwound moisture-associated dermatitis is managing the excessive exudate.
How long does it take for a stoma to adjust to a new shape?
When cutting or molding the skin barrier to fit the stoma, it is recommended that frequent measurements of the stoma be conducted over the first 6 weeks to adjust to the changing shape of the stoma.
How to treat intertriginous dermatitis?
Keep at-risk areas clean and dry. Shower after exercise, then thoroughly pat dry the skin inside the fold. Use a pH-balanced skin cleanser. Promote proper general skin hygiene. The goal of treatment for intertriginous dermatitis is to minimize moisture and friction in the skin fold and to treat any infections.
How are gastric ulcers subdivided?
Rationale: Gastric ulcers are subdivided by severity and then further subdivided by hemorrhage and/or perforation.
What is the ICD-10 code for cellulitis?
Rationale:Documentation supports that cellulitis is the first listed diagnosis. Review of the Tabular shows that ICD-10-CM classifies the laterality of cellulitis of the lower extremity, with L03.115 being the right lower extremity. A note appears in the Tabular under the section Infections of the Skin and Subcutaneous Tissue (L00-L08) instructing to use an additional code (B95-B97) to identify infectious agent. ICD-10-CM also classifies decubitus ulcers of the buttocks both by stage and laterality. Gluteus is not listed in the classification, but it refers to the buttock region.
What is the ICd 10 code for Crohn's disease?
K50.012 Crohn’s disease –see Enteritis, regional, Enteritis (acute) (diarrheal) (hemorrhagic) (noninfective) (septic), regional (of), small intestine, with complication, intestinal obstruction Rationale:An additional code for the small bowel obstruction is not required as the combination code in ICD-10-CM identifies both the Crohn’s disease and the small bowel obstruction. Exacerbation is not a qualifier for Crohn’s disease.
What is the index for dermatitis?
This was documented as irritant contact dermatitis, but not allergic, so Index contact, irritant, due to cosmetics, L24.3. Under contact, allergic, due to cosmetics there is a different code L23.2, if documentation supported that code.
What is the instructional note code for a drug?
An instructional note appears in the Tabular, under codes L27.0 and L27.1, stating to use additional code for adverse effect, if applicable, to identify drug (T36-T50 with fifth or sixth character 5).
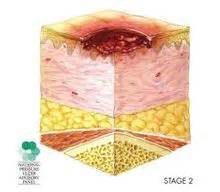
What stage is oSite, laterality, and severity specified in single code oSeverity identified as?
oSite, laterality, and severity specified in single code oSeverity identified as stage 1–4
Why is O75.2 not coded?
The fever during labor (O75.2) is not coded because the cause is known (infection).
Etiology
Symptoms
- Periwound moisture-associated dermatitis is marked by erythema (which may be harder to discern in persons with darkly pigmented skin), maceration (white, pale, or gray skin that is softened and/or wrinkled), and irregular or diffuse edges (as opposed to pressure ulcers which typically have distinct edges). Wounds with more viscous exudate are more prone to periwound …
Risk Factors
- The following wounds are more prone to developing periwound moisture-associated dermatitis: 1. Diabetic foot ulcers 2. Venous leg ulcers 3. Pressure ulcers 4. Fungating tumors 5. Full-thickness (third-degree) burns Wound infection will also greatly increase the risk of periwound maceration, as it increases the exudate production.
Treatment & Interventions
- The following precautions can help minimize the risk of developing periwound moisture-associated dermatitis in at-risk patients and to minimize complications in patients already exhibiting symptoms: 1. Monitor the wound area routinely for changes in skin condition. 2. Manage wound exudate with dressings chosen for proper absorbency. 3. Apply a barrier film or …
References
- Alvey B, Beck DE. Peristomal Dermatology. Clin Colon Rectal Surg. 2008;21(1):41-44. doi: 10.1055/s-2008-1055320 Black JM, Gray M, Bliss DZ, Kennedy-Evans KL, Logan S, Baharestani MM, Colwell JC, Goldberg M, Ratliff CR. MASD Part 2: Incontinence-Associated Dermatitis and Intertriginous Dermatitis. J Wound Ostomy Continence Nurs. 2011;38(4):359-370. doi: 10.1097/…
Popular Posts:
- 1. icd 10 code for hpvd
- 2. icd-10 code for breast 9 fibroglandular tissue
- 3. icd 10 code for left hip effusion
- 4. icd 10 code for e. coli
- 5. icd 10 code for swelling of thyroid gland
- 6. icd 10 code for alzheimer's with vascular dementia
- 7. icd 10 code for lap band
- 8. icd 10 code for fhx brca
- 9. icd 10 cm code for bloody discharge nipple
- 10. icd-10 code for axilla carcinoma invasive