What indicates perforation and peritonitis?
a sign of intestinal perforation, this indicates the presence of free air in the peritoneal cavity originating from the perforated intestine. Usually this is an early sign of peritonitis [10]. If a pneumoperitoneum occurs due to rupture of a hollow organ, air will accumulate in the right side of the abdomen under the
What are the causes and symptoms of peritoneal cancer?
- Swelling of the abdomen or ankles
- Breathing problems
- Extreme fatigue
- Loss of appetite
- Unusual weight gain from fluid accumulation
- Lower back pain
What are the nursing responsibilities in peritoneal dialysis?
The nurses responsibilities include:
- checking the patients' vital signs and talking with them to assess their condition
- teaching patients about their disease and its treatment and answering any questions
- overseeing the dialysis treatment from start to finish
- making sure patients are given the correct medications ordered by their doctors
What are abdominal symptoms of peritonitis?
Signs and symptoms of peritonitis include:
- Abdominal pain or tenderness
- Bloating or a feeling of fullness in your abdomen
- Fever
- Nausea and vomiting
- Loss of appetite
- Diarrhea
- Low urine output
- Thirst
- Inability to pass stool or gas
- Fatigue
How do you code peritonitis due to peritoneal dialysis?
ICD-10 Code for Infection and inflammatory reaction due to peritoneal dialysis catheter, initial encounter- T85. 71XA- Codify by AAPC.
What is the ICD-10 code for peritonitis?
K65. 9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM K65.
What is the ICD-10 PCS code for peritoneal?
Hemodialysis, single encounter, is classified to ICD-10-PCS code 5A1D00Z, which is located in the Extracorporeal Assistance and Performance section. Multiple encounters of hemodialysis is classified to code 5A1D60Z. Peritoneal dialysis is classified to code 3E1M39Z, which is located in the Administration section.
What is DX code Z51 89?
Encounter for other specified aftercareICD-10 code Z51. 89 for Encounter for other specified aftercare is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What peritonitis means?
Peritonitis is a redness and swelling (inflammation) of the lining of your belly or abdomen. This lining is called the peritoneum. It is often caused by an infection from a hole in the bowel or a burst appendix.
What is perforation peritonitis?
Introduction: Perforation peritonitis mostly results from the perforation of a diseased viscus. Other causes of perforation include abdominal trauma, ingestion of sharp foreign body and iatrogenic perforation. The diagnosis is mainly based on clinical grounds.
What is the ICD-10 code for dialysis?
ICD-10 code Z99. 2 for Dependence on renal dialysis is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
How do you bill for peritoneal dialysis?
You have the correct billing code, 90966, to use when reporting monthly outpatient care for PD ESRD patients. Medicare pays the same for PD MCP care (90966) regardless of the number of outpatient visits that occur during the month.
What is the ICD-10 code for removal of peritoneal dialysis catheter?
Note: Code 0WPGX3Z, defined for external approach, is assigned for removal of the peritoneal dialysis catheter by pull.
What is diagnosis code Z51 11?
ICD-10 code Z51. 11 for Encounter for antineoplastic chemotherapy is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
When do you use ICD-10 Z47 89?
Use Z codes to code for surgical aftercare. Z47. 89, Encounter for other orthopedic aftercare, and. Z47. 1, Aftercare following joint replacement surgery.
What kind of settings can Z codes be used in?
any healthcare settingZ codes are for use in any healthcare setting. Z codes may be used as either a first-listed (principal diagnosis code in the inpatient setting) or secondary code, depending on the circumstances of the encounter. Certain Z codes may only be used as first-listed or principal diagnosis.
What is secondary peritonitis?
Secondary peritonitis arises from the abdominal cavity itself through rupture or abscess of intra-abdominal organs. Inflammation of the peritoneum, a condition marked by exudations in the peritoneum of serum, fibrin, cells, and pus. Inflammation of the thin membrane surrounding abdominal cavity, called peritoneum.
What is the cause of peritoneal inflammation?
Inflammation of the peritoneum lining the abdominal cavity as the result of infectious, autoimmune, or chemical processes. Primary peritonitis is due to infection of the peritoneal cavity via hematogenous or lymphatic spread and without intra-abdominal source. Secondary peritonitis arises from the abdominal cavity itself through rupture or abscess of intra-abdominal organs.
What is the peritoneum?
Clinical Information. Inflammation of the peritoneum (tissue that lines the abdominal wall and covers most of the organs in the abdomen). Peritonitis can result from infection, injury, or certain diseases. Symptoms may include swelling of the abdomen, severe pain, and weight loss.
What is the term for a peritoneal infection that covers most of the abdominal organs?
peritonitis with or following appendicitis ( K35.-) retroperitoneal infections ( K68.-) Inflammation of the peritoneum (tissue that lines the abdominal wall and covers most of the organs in the abdomen). Peritonitis can result from infection, injury, or certain diseases.
Why does my peritoneum hurt?
Inflammation of the peritoneum due to infection by bacteria or fungi. Causes include liver disease, perforation of the gastrointestinal tract or biliary tract, and peritoneal dialysis. Patients usually present with abdominal pain and tenderness, fever, chills, and nausea and vomiting.
When will the ICd 10 K65.9 be released?
The 2021 edition of ICD-10-CM K65.9 became effective on October 1, 2020.
What is the cause of peritoneal inflammation?
Inflammation of the peritoneum lining the abdominal cavity as the result of infectious, autoimmune, or chemical processes. Primary peritonitis is due to infection of the peritoneal cavity via hematogenous or lymphatic spread and without intra-abdominal source. Secondary peritonitis arises from the abdominal cavity itself through rupture or abscess of intra-abdominal organs.
What is the peritoneum?
Inflammation of the peritoneum (tissue that lines the abdominal wall and covers most of the organs in the abdomen). Peritonitis can result from infection, injury, or certain diseases. Symptoms may include swelling of the abdomen, severe pain, and weight loss.
Why does my peritoneum hurt?
Inflammation of the peritoneum due to infection by bacteria or fungi. Causes include liver disease, perforation of the gastrointestinal tract or biliary tract, and peritoneal dialysis. Patients usually present with abdominal pain and tenderness, fever, chills, and nausea and vomiting. It is an emergency medical condition that requires prompt medical attention and treatment.
When will the ICD-10-CM K65 be released?
The 2022 edition of ICD-10-CM K65 became effective on October 1, 2021.
What is peritoneal dialysis?
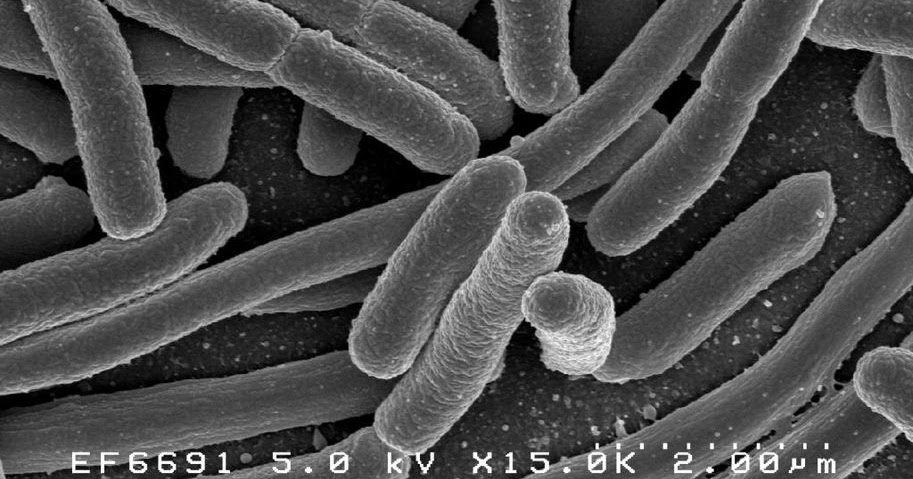
Introduction to Peritonitis in Peritoneal Dialysis. Peritonitis is the inflammation of the peritoneum or peritoneal membrane. This type of inflammation typically has an infectious etiology that is mainly caused by bacteria (~80% of cases). Bacterial infections mainly come from contamination during a peritoneal dialysis (PD) session.
What is the treatment for tuberculous peritonitis?
Special culture techniques should be considered. Treatment should be based on a 4 drug regimen: rifampicin, isoniazid, pyrazinamide, and ofloxacin, if diagnosed. Pyraz inamide and ofloxacin can be stopped after 2 months but rifampin and isoniazid should be continued for a total of 12 to 18 months. Patients often respond to therapy without catheter removal.
What is the most common complication of PD?
Peritonitis is a major complication of PD due to the structural changes in the peritoneal membrane that result from PD. Approximately 4% of peritonitis episodes result in death. Since peritonitis is one of the more common complications of PD, it has caused patients to switch from this modality to hemodialysis.
Why is culture negative for peritonitis?
Culture negative peritonitis may be due to recent antibiotic usage or technical reasons. The guidelines recommend repeat WBC count with differential if the effluent yields no growth after 3 days. If the peritonitis has not clinically improved at day 3, special culture techniques that test for mycobacteria, nocardia, legionella, filamentous fungus, or other fastidious bacteria should be considered. Initial therapy may be continued for 2 weeks if clinical improvement is noted and the effluent clears quickly. However, if improvement is not observed in 5 days, catheter removal should be strongly considered.
Why is monitoring peritonitis important?
Monitoring peritonitis rates and evaluating outcomes of peritonitis treatment are important to ensure patients are receiving the best possible treatment.
How long after refractory peritonitis can you take antibiotics?
Simultaneous re-insertion of a new catheter is not recommended for refractory and fungal peritonitis. Antibiotics should be continued for at least 2 weeks after catheter removal for refractory peritonitis.
How long does it take to treat polymicrobial peritonitis?
The patient should be treated with effective antibiotics for 3 weeks.
What causes PD in the peritoneum?
Most cases of PD-related peritonitis are the result of touch contamination, in which the infecting organism gains access to the peritoneum via the catheter lumen. A small percentage result from exit-site or tunnel infections, in which organisms spread down the catheter tunnel outside the lumen to the peritoneum.3Exit-site infection presents as purulent drainage at the exit site, with or without erythema. Erythema by itself does not indicate an exit-site infection.5Swelling, induration, and/or erythema that extends more than 2 cm proximally to the exit site defines a tunnel infection, which presents a much higher risk of developing peritonitis. The organisms causing exit-site infections with the highest risk of subsequent peritonitis are S. aureus, coagulase-negative staphylococci, diphtheroids, streptococcal species, Pseudomonas aeruginosa, and Candida.6Nontuberculous mycobacteria (NTM) species have also been reported to cause exit-site infections and peritonitis, particularly in patients using gentamicin cream for exit-site prophylaxis.7
What is the source of peritonitis?
The PD catheter is the source of infection for the vast majority of PD-related cases of peritonitis. The catheter provides a portal of entry for organisms into the normally sterile peritoneum. Most cases of PD-related peritonitis are the result of “touch contamination”, where the patient or their helper inadvertently breaks sterile technique and contaminates the catheter or its connections. The most common pathogens are coagulase-negative staphylococcal species (eg, Staphylococcus epidermidis) that commonly colonize human skin and hands, and Staphylococcus aureus, which together are responsible for 50% or more of infections in most series.2–4Exit-site and tunnel infections may also lead to peritonitis. Less commonly, the abdomen itself may be the source. Diverticulitis, appendicitis, cholecystitis, or a perforated viscus may be the source, as well as intra-abdominal surgery, colonoscopy, hysteroscopy, and transmigration of bowel flora from constipation. In cases with an intra-abdominal source, the infecting organisms are usually Gram-negative enteric bacteria, streptococci and anaerobic bacteria. Bacteremia from another source may also seed the peritoneum.
What antibiotics should be used for PD?
The choice of antibiotics should be determined by the prevalence and types of antibiotic-resistant bacterial isolates from peritonitis patients in the program. Antibiotics should be administered intraperitoneally in most cases.2For empiric coverage of Gram-positive bacteria, recommended drugs are cefazolin or vancomycin . In programs with a low incidence of MRSA species and enterococci, cefazolin would be preferred. In many programs, MR coagulase-negative staphylococci and MRSA are common pathogens in peritonitis patients, and vancomycin should be used initially, pending culture results. For empiric coverage of Gram-negative bacteria, initial therapy should include a third-generation cephalosporin (ceftazidime or cefepime) or an aminoglycoside (gentamicin, tobramycin, or amikacin). Again, the choice of antibiotics for empiric Gram-negative coverage is dependent on the species of bacteria and the prevalence and types of antibiotic-resistant pathogens in the program.
How to administer antibiotics for PD?
The preferred method of antibiotic administration for PD-related peritonitis is intraperitoneal. The advantages of intraperitoneally administered antibiotics include delivery of a high concentration of antibiotics at the site of infection, antibiotics also being absorbed into the systemic circulation and diffusing back into the peritoneum, allowing daily or less frequent administration, and intravenous (IV) access, which would be required for 2–4 weeks, is not necessary (Table 2).
How long does it take for peritonitis to improve?
Treatment for 14 days is recommended, with cure rates about 70% or more in most series.16Catheter replacement or removal is often required for relapsing or recurrent cases, which presumably occurs due to biofilm formation in the catheter.
Is peritoneal dialysis effective?
Peritoneal dialysis is an effective treatment modality for patients with end-stage renal disease. The relative use of peritoneal dialysis versus hemodialysis varies widely by country. Data from a 2004 survey reports the percentage of patients with end-stage renal disease treated with peritoneal dialysis to be 5%–10% in economically developed regions like the US and Western Europe to as much as 75% in Mexico. This disparity is probably related to the availability and access to hemodialysis, or in some cases patient preference for peritoneal over hemodialysis. Peritoneal dialysis-related peritonitis remains the major complication and primary challenge to the long-term success of peritoneal dialysis. Fifty years ago, with the advent of the Tenckhoff catheter, patients averaged six episodes of peritonitis per year on peritoneal dialysis. In 2016, the International Society for Peritoneal Dialysis proposed a benchmark of 0.5 episodes of peritonitis per year or one episode every 2 years. Despite the marked reduction in peritonitis over time, peritonitis for the individual patient is problematic. The mortality for an episode of peritonitis is 5% and is a cofactor for mortality in another 16% of affected patients. Prevention of peritonitis and prompt and appropriate management of peritonitis is essential for the long-term success of peritoneal dialysis in all patients. In this review, challenges and solutions are addressed regarding the pathogenesis, clinical features, diagnosis, treatment, and prevention of peritoneal dialysis-related peritonitis from the viewpoint of an infectious disease physician.
Does S. aureus cause peritonitis?
S. aureusgenerally produces a more clinically severe form of peritonitis in PD patients, because of its many virulence factors. S. aureuscolonizes many patients in their nares and on their skin, as well as disruptions of the skin, like an exit site. In one study, 45% of patients initiating PD were found to be nasal carriers of S. aureusand had a significantly higher risk of developing an exit-site infection.17S. aureusis a common cause of exit-site and tunnel infections. Mupirocin for exit-site prophylaxis seems to reduce exit-site infections, peritonitis, and catheter loss due to S. aureus.18
How long should I treat peritonitis?
In essence, if the clinical response is satisfactory, peritonitis caused by coagulase-negative staphylococci, streptococci, or culture-negative episodes should be treated for 2 weeks ( 6 ). For culture-negative episodes, it remains controversial whether the antibiotic for Gram-negative coverage should be discontinued. The current recommendations state that if aminoglycoside is used as the empirical Gram-negative coverage, it should be stopped to minimize the risk of ototoxicity from repeated exposure ( 6 ), although a small study has suggested that N-acetylcysteine may prevent aminoglycoside-related ototoxicity ( 42 ).
How long should antibiotics be given for peritonitis?
aureus, enterococci, Corynebacterium species, Gram-negative bacilli ( Pseudomonas or non- Pseudomonas species), and polymicrobial peritonitis, effective antibiotics should be continued for 3 weeks.
How often should peritonitis be monitored?
The ISPD recommendations emphasize that every PD program should monitor the PD-associated peritonitis rate at least on a yearly basis ( 6 ). The rate should be reported as the number of episode per patient-year but not the number of patient-months per episode ( 6 ). In addition to the overall peritonitis rate, the peritonitis rates of specific organisms, percentage of peritonitis-free patients per year, and the spectrum of antibiotic resistance should be monitored ( 6 ). During the calculation of peritonitis rate, relapsing episodes should be counted only once, and all episodes that develop after PD training has commenced (not completed) should be counted ( 6 ). Although the recommendations state that the overall peritonitis rate should be below 0.5 episodes per patient-year, there is a wide variation in the peritonitis rates reported by different countries, as well as by different centers within the same country ( 8 ). A recent study shows highly variable rates of adopting the ISPD recommendations across different centers, and such variations probably account for the difference in infection risk between PD centers ( 9 ).
What should be done after each episode of peritonitis?
After each episode of peritonitis, a root cause analysis should be performed to determine the etiology and possible interventions to prevent further episodes ( 6 ). For example, exchange technique should be reviewed after peritonitis episodes caused by touch contamination, and replacement of PD catheter should be considered after relapsing or repeat peritonitis episodes ( 6 ). The key measures for the prevention of PD-associated peritonitis are summarized in Table 1.
Does mupirocin cream help with peritonitis?
Daily application of mupirocin cream or ointment to the skin around the exit site reduces the rate of S. aureus exit site infection and probably decreases the rate of peritonitis ( 24, 25 ). Intranasal mupirocin is effective for reducing S. aureus exit site infection, but not peritonitis ( 26 ).
When should antibiotics be adjusted for PD?
Once the PD effluent Gram stain or culture results are known , antibiotic therapy should be adjusted ( 6 ). In general, if Gram-positive organisms are identified, antibiotic coverage for Gram-negative bacteria ( i.e., aminoglycoside or third-generation cephalosporin) could be stopped, and vice versa once sensitivities are available. PD effluent leukocyte counts and bacterial culture should be performed again 2–3 days after antibiotic therapy, especially when there is no clinical improvement. PD effluent leukocyte count >1090/ µ l on day 3 may predict treatment failure ( 41 ).
Does nystatin help with peritonitis?
Most fungal peritonitis episodes are preceded by the use of systemic antibiotics ( 6, 33 ). Randomized, controlled trials and a systematic review show that the use of either oral nystatin or fluconazole during antibiotic therapy reduces the risk of secondary fungal (especially Candida) peritonitis ( 6, 10 ). In countries where nystatin is available, it should be the preferred choice because it has no systematic effect or drug interactions. Antifungal prophylaxis may also reduce the risk of fungal peritonitis when a patient on PD receives systemic antibiotics for nonperitonitis infections ( 10 ), but this practice does not seem to be widely adopted.

Popular Posts:
- 1. icd 10 code for history of pericardial effusion
- 2. icd 10 code for feet dysesthesia
- 3. low back surgery for spinal stenosis icd code
- 4. icd 10 code for atypia of undetermined significance thyroid
- 5. icd 10 cm code for slow weight gain
- 6. icd 10 code for left ovarian follicular cyst
- 7. icd 10 code for abnormal hemoglobin and hematocrit
- 8. icd 9 code for cannabis dependence
- 9. icd 10 code for amebic balanitis
- 10. icd 10 code for lumbar radiculopathy right side