What is the ICD 10 code for persistent vegetative state?
Persistent vegetative state. R40.3 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2019 edition of ICD-10-CM R40.3 became effective on October 1, 2018.
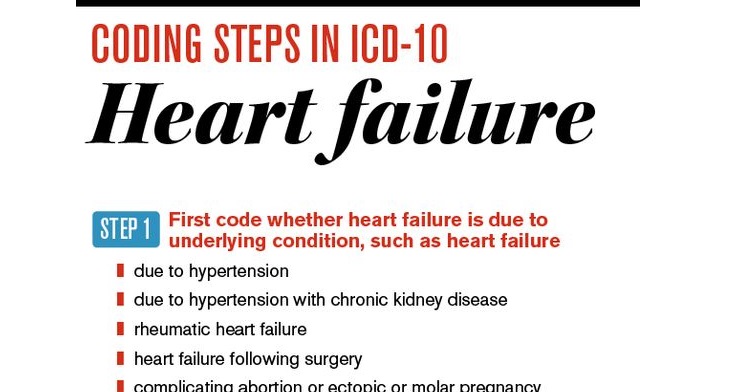
What is the ICD 10 code for hypertension?
ICD-10 uses only a single code for individuals who meet criteria for hypertension and do not have comorbid heart or kidney disease. That code is I10, Essential (primary) hypertension.
What is a type 1 exclude note in ICD 10?
It means "not coded here". A type 1 excludes note indicates that the code excluded should never be used at the same time as I48.1. A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition.
What is the ICD-10 code G44 52?
New daily persistent headacheG44. 52 New daily persistent headache (NDPH) - ICD-10-CM Diagnosis Codes.
What is this diagnosis code F34 9?
F34. 9 - Persistent Mood [affective] Disorder, Unspecified [Internet]. In: ICD-10-CM.
What is diagnosis code F43 21?
ICD-10 code F43. 21 for Adjustment disorder with depressed mood is a medical classification as listed by WHO under the range - Mental, Behavioral and Neurodevelopmental disorders .
What is the ICD-10 code for persistent vegetative state?
R40.3ICD-10 code R40. 3 for Persistent vegetative state is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
What does diagnosis F34 1 mean?
ICD-10 code: F34.1. Persistent depressive disorder (dysthymia) is part of a cluster of diagnoses called the depressive disorders. Depressive disorders are a group of psychiatric conditions that include: Major depressive disorder (including major depressive episode)
What does anxiety F41 9 mean?
Code F41. 9 is the diagnosis code used for Anxiety Disorder, Unspecified. It is a category of psychiatric disorders which are characterized by anxious feelings or fear often accompanied by physical symptoms associated with anxiety.
What is F43 22 code?
ICD-10 code F43. 22 for Adjustment disorder with anxiety is a medical classification as listed by WHO under the range - Mental, Behavioral and Neurodevelopmental disorders .
What is the diagnosis code F43 23?
ICD-9 Code Transition: 309.28 Code F43. 23 is the diagnosis code used for Adjustment Disorder (AD) with Mixed Anxiety and Depressed Mood. It is sometimes known as situational depression. It occurs when an individual is unable to adjust to or cope with a particular stress or a major life event.
What does f41 8 mean?
8: Other specified anxiety disorders.
What is a semi conscious state?
A minimally conscious state is severe but not complete impairment of awareness. It results from widespread damage to the cerebrum (the part of the brain that controls thought and behavior). A minimally conscious state may result from brain damage, or it may follow a vegetative state as people recover some function.
What is a human vegetable?
A vegetative state is when a person is awake but is showing no signs of awareness. A person in a vegetative state may: open their eyes. wake up and fall asleep at regular intervals. have basic reflexes (such as blinking when they're startled by a loud noise or withdrawing their hand when it's squeezed hard)
What is the ICD 10 code for unresponsive?
ICD-10-CM R40. 20 is grouped within Diagnostic Related Group(s) (MS-DRG v39.0): 080 Nontraumatic stupor and coma with mcc. 081 Nontraumatic stupor and coma without mcc.
Is Dmdd a mental illness?
DMDD is a newly classified disorder, first appearing in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) in 2013. The DSM is used for the assessment and diagnosis of mental disorders; it does not include specific guidelines for the treatment of any disorder.
Is F34 9 a billable code?
F34. 9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What does unspecified PTSD mean?
Code F43. 10 is the diagnosis code used for Post-Traumatic Stress Disorder, Unspecified. It is an anxiety disorder that develops in reaction to physical injury or severe mental or emotional distress, such as military combat, violent assault, natural disaster, or other life-threatening events.
What is the ICd 10 code for chronic pain?
Chronic pain, not elsewhere classified 1 G89.2 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail. 2 The 2021 edition of ICD-10-CM G89.2 became effective on October 1, 2020. 3 This is the American ICD-10-CM version of G89.2 - other international versions of ICD-10 G89.2 may differ.
When will the ICD-10 G89.2 be released?
The 2022 edition of ICD-10-CM G89.2 became effective on October 1, 2021.
What is the difference between an unspecified and an other code?
These two codes have different meanings. An “other” code means that there are codes for some diagnoses, but there is not one specific for the patient’s condition. In this case, the physician knows what the condition is, but there is no code for it. An “unspecified” code means that the condition is unknown at the time of coding. An “unspecified” diagnosis may be coded more specifically later, if more information is obtained about the patient’s condition.
Can ICD-10 codes be denied for Medicare Part B?
In July 2015, the Centers for Medicare & Medicaid Services (CMS) announced an agreement with the AMA that Medicare Part B claims generally will not be denied solely based on the specificity of the diagnosis codes, as long as they are from the appropriate family of ICD-10 codes. In addition, some commercial payers have allowed flexibility with the level of detail of diagnosis codes during the early transition phase. CMS’ acceptance of the “family of codes” will end in September 2016, and it is uncertain when the commercial payers will no longer allow less specific coding. Therefore, it is best for physicians to begin evaluating their level of coding specificity and ensure they are coding to the greatest level of detail representing the patient’s condition and supported by the documentation of the encounter.
Popular Posts:
- 1. icd-10 code for familial dissection of the thoracic aorta
- 2. icd 10 code for myoclonic epilepsy
- 3. icd 10 code for severe djd of hands
- 4. icd 10 cm code for bleeding from fistula
- 5. icd-10 code for hammertoe of left foot
- 6. icd 10 code for acute back sprain
- 7. icd-10 code for glycosuria
- 8. icd 10 code for squamous cell carcinoma left cheek
- 9. icd 10 code for asymmetry of the prostate on the right side
- 10. icd 10 cm code for helminth infection, unspecified