What are the ICD-10 codes for physical therapy?
You can practice Physical Therapy ICD-10 codes with our free online flashcards! Go to Flashcards now! Chapter 13 - Diseases of the musculoskeletal system and connective tissue (M00-M99) + Section M60-M63 -. Disorders of muscles (M60-M63) 10. M62.81.
When should a physical therapist choose between an initial Eval and re-evaluation?
So, to clear up some confusion, we put together a few common situations in which a physical therapist must choose between billing for an initial eval and a re-eval—along with our advice on how to handle those situations: A current patient develops a newly diagnosed, related condition.
Do you need an evaluation code for post-op treatment?
The catch in this situation is that some commercial payers may consider the post-op treatment period a new episode of care, in which case you’d need to use an evaluation code. Example: You treat a patient for osteoarthritis.
When do you need a re-evaluation for post-operative rehabilitation?
Re-evaluations also may be appropriate for patients who received therapy treatment prior to surgery and then returned for additional rehabilitation after surgery. The catch in this situation is that some commercial payers may consider the post-op treatment period a new episode of care, in which case you’d need to use an evaluation code.
How do you code a physical therapy evaluation?
Three codes — 97161, 97162, and 97163 — are used for physical therapy evaluation.
What is the CPT code for physical therapy re-evaluation?
97164 - Re-evaluation of physical therapy established plan of care, requiring these components: An examination including a review of history and use of standardized tests and measures is required; and a revised plan of care using a standardized patient assessment instrument and/or measurable assessment of functional ...
Is PT re eval a timed code?
This is not a timed code. The AMA CPT Assistant, which provides explanations of how CPT codes should be used, includes the following example of a PT re-eval: A 62-year-old male with low back pain presents for a physical therapy re-evaluation on his eighth visit of his episode of care.
What is a re-evaluation in physical therapy?
RE-EVALUATION OF PHYSICAL THERAPY ESTABLISHED PLAN OF CARE, REQUIRING THESE COMPONENTS: AN EXAMINATION INCLUDING A REVIEW OF HISTORY AND USE OF STANDARDIZED TESTS AND MEASURES IS REQUIRED; AND REVISED PLAN OF CARE USING A STANDARDIZED PATIENT ASSESSMENT INSTRUMENT AND/OR MEASURABLE ASSESSMENT OF FUNCTIONAL OUTCOME ...
Can 97164 and 97110 be billed together?
That's because CMS—at the behest of the APTA—has agreed to accept these pairs without the use of a modifier. In other words, you can perform the following services—and receive payment for them—without needing to affix modifier 59: 97110 with 97164.
What is procedure code 97112?
CPT 97112 means “neuromuscular reeducation of movement, balance, coordination, kinesthetic sense, posture, and/or proprioception for sitting and/or standing activities.” Like therapeutic activity, therapeutic procedures also apply to one or multiple body parts and require direct contact with the proper provider1.
Does Medicare cover G0283?
Stimulation delivered via electrodes should be billed as G0283. The charges for the electrodes are included in the practice expense portion of code G0283. Do not bill the Medicare contractor or the patient for electrodes used to provide electrical stimulation as a clinic modality.
Does 97010 need a modifier?
This policy change requires that claims with physical medicine services 97010-97799 will require modifier GP. The modifier is required for dates of service after April 1, 2021. Any PT now billed to Anthem will require the GP modifier.
What is procedure code 97162?
97162 - Physical therapy evaluation: moderate complexity, requiring these components: • A history of present problem with 1-2 personal factors and/or comorbidities that impact the plan of. care; • An examination of body systems using standardized tests and measures in addressing a total of 3 or.
What is procedure code 97116?
CPT® 97116, Under Physical Medicine and Rehabilitation Therapeutic Procedures. The Current Procedural Terminology (CPT®) code 97116 as maintained by American Medical Association, is a medical procedural code under the range - Physical Medicine and Rehabilitation Therapeutic Procedures.
What is procedure code 97165?
Low complexity (97165) An occupational profile and medical and therapy history that includes a brief history, including review of medical and/or therapy records relating to the presenting problem.
Can PTA do reevaluation?
Yes; as the APTA explains here, “although PTAs cannot make changes to the overall plan of care, they are trained to make treatment adjustments to accommodate a patient during a session.” The same holds true for OTAs.
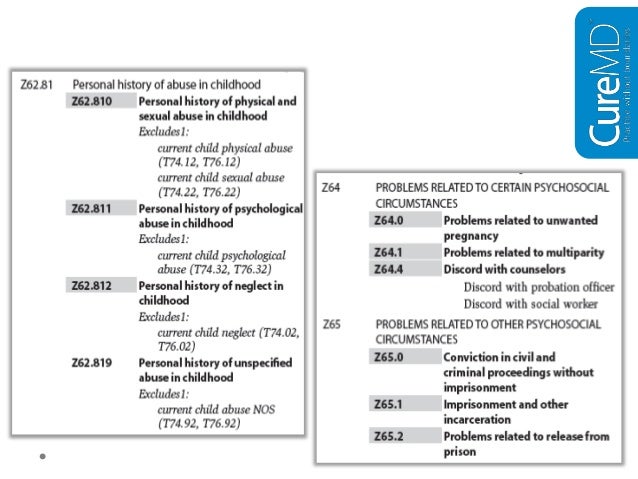
How long did it take to develop the ICd 10?
Yes, it took almost a decade to create ICD-10, and it has taken more than a decade for the US to actually put the final version of the code set to use. Australia was one of the first countries to adopt ICD-10. Half of the Australian states implemented ICD-10 in 1998, and the rest of the country followed in 1999.
Which countries have adopted the ICD-10 code?
Canada adopted the new code set in 2000, and from there, several European countries as well as Thailand, Korea, China, and South Africa adopted ICD-10 in its original, modified, or translated form. Even Dubai made the switch in 2012.
What are external cause codes?
These codes are listed in Chapter 20: External cause codes. They’re secondary codes, which means they expand upon the description of the cause of an injury or health condition by indicating how it happened ( i.e., the cause), the intent ( i.e., intentional or accidental), the location, what the patient was doing at the time of the event, and the patient’s status (e.g., civilian or military). You should use as many external cause codes as necessary to explain the patient’s condition as completely as possible. However, external cause codes need only be used once, usually at the initial encounter.
Is ICd 10 the same as CPT?
Note: ICD-10 codes are completely separate from CPT codes. The transition to ICD-10 does not affect the use of CPT codes. Additionally, ICD-10 codes do not impact guidelines regarding the the KX modifier.
What is 97164 in a re-evaluation?
Use: Re-evaluation (97164) This could include any improvement, decline, or other change in functional status that: you didn’t anticipate when you originally established the plan of care, and. requires further evaluation to ensure the best therapy outcomes.
What is 97164 in medical?
Use: Re-evaluation (97164) If you are treating a patient, and he or she presents with a second diagnosis that is either related to the original diagnosis or is a complication resulting from the original diagnosis, you’ll need to complete a re-evaluation and create an updated plan of care.
What is 97164 in healthcare?
Use: Re-evalua tion (97164) If, during the course of care, you determine that the original plan isn’t having the intended effect on the patient, you may feel it necessary to change the plan of care. In this case, you would perform—and bill for—a re-evaluation.
Can you re-evaluate after surgery?
Re-evaluations also may be appropriate for patients who received therapy treatment prior to surgery and then returned for additional rehabilitation after surgery. The catch in this situation is that some commercial payers may consider the post-op treatment period a new episode of care, in which case you’d need to use an evaluation code.
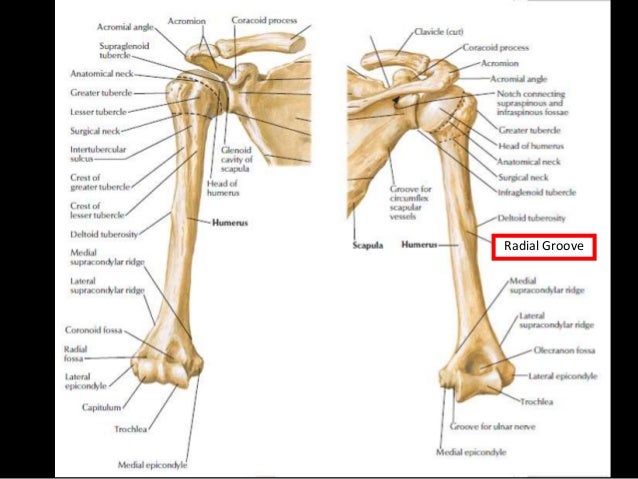
Should you defer to the payer for a rotator cuff evaluation?
For those patients with commercial insurances, you should defer to the payer—as well as your state practice act if it includes guidance on when evaluations and re-evaluations are appropriate . Example: You treat a 30-year-old carpenter for right rotator cuff weakness and discharge him or her from care.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
Therapy evaluation and formal testing services involve clinical judgment and decision-making which is not within the scope of practice for therapy assistants.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
What is re-evaluation of occupational therapy?
Re-evaluation of occupational therapy established plan of care requiring: An assessment of changes in patient functional or medical status, along with a revised plan of care. An update to the initial occupational profile to reflect changes in condition or environment that affect future interventions and/or goals.
What is a CPT code?
What are CPT Codes? CPT is short for Current Procedural Terminology and the codes published by the American Medical Association. CPT codes are used to classify medical, surgical and diagnostic services and procedures, and range from 00100 to 99499.
What is the ICd 9?
ICD-9 was the ninth version of the ICD coding system, connecting the health issues of patients by using 3 to 5 digit alphanumeric codes. However, in 2015, ICD-10 (the 10th revision) was introduced, using 4 to 7 digit alphanumeric code.
What is the difference between CPT and ICD?
While Physical Therapists use CPT codes to regiment the treatment of diagnoses, ICD coding is the standard international system for recording diagnoses and classifying mortality and morbidity statistics. The World Health Organization (WHO) created the ICD and still watches over it.
Why do you need modifiers in CPT?
Modifiers are added to CPT codes when they are required to more accurately describe a procedure performed or service rendered. A modifier should never be used in order to receive a higher reimbursement or to get paid for a procedure that should be bundled with another code.
How long is manual therapy?
Alternatively, the therapy time blocks may be split. For example, manual therapy might be performed for 10 minutes, followed by 15 minutes of therapeutic activities , followed by another 5 minutes of manual therapy. CPT code 97530 should not be reported and modifier 59 should not be used if the two procedures are performed during the same time block.
What is a revised plan of care?
A revised plan of care (a formal re-evaluation is performed when there is a documented change in functional status or a significant change to the plan of care is required) If you need further explanation of the evaluation and re-evaluation codes, do not hesitate to contact your StrataPT account manager.
Document Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
This LCD supplements but does not replace, modify or supersede existing Medicare applicable National Coverage Determinations (NCDs) or payment policy rules and regulations for Therapy and Rehabilitation Services. Federal statute and subsequent Medicare regulations regarding provision and payment for medical services are lengthy.
Coverage Guidance
Please refer to the CMS IOM Publication 100-02, Medicare Benefit Policy Manual, Chapter 15, Section 220 for definitions, references, general therapy guidelines, furnishing therapy services in a pool, conditions of coverage and payment, care of a physician/nonphysician practitioner, plan of care requirements, certification and recertification of need for treatment and therapy plans of care, requirement that services be furnished on an outpatient basis, covered indications and limitations, documentation requirements, functional reporting..
What is the CPT code for physical therapy?
The most commonly used CPT codes for Physical Therapy are listed below. For example, the CPT code for therapeutic exercise is 97110. The CPT code is listed on the left, the name of the code is in the middle and the description is in the right column.
What happens if CPT code doesn't match ICD-10?
If the CPT code doesn’t support the ICD-10 code, you’ll have a problem – and you’ll likely have trouble getting reimbursed.
What is therapeutic exercise?
Therapeutic Exercise. Therapeutic procedure, one or more areas, each 15 minutes; therapeutic exercises to develop strength and endurance, range of motion, and flexibility. (Generally describes a service aimed at improving a single parameter, such as strength, ROM, etc.) 97112.
What does CPT stand for in medical terms?
CPT stands for Current Procedural Terminology and are published by the American Medical Association. Ranging from 00100 to 99499, the CPT codes are used to describe medical, surgical, and diagnostic services and procedures. Medical professionals like Physical Therapists use CPT codes to classify the treatment of diagnoses.
A Current Patient Develops A Newly Diagnosed, Related Condition.
A Current Patient Develops A Newly Diagnosed, Unrelated Condition.
- Use: Initial Evaluation (97161–97163) Conversely, when a patient with an active plan of care presents with a second condition that is totally unrelated to the primary issue, you should select the appropriate initial evaluation code. The nuance for therapists to remember is that a re-evaluation is triggered by a significant clinical change in the condition for which the original pla…
A Patient Undergoes Surgery Mid-Plan of Care.
- Use: Re-evaluation (97164) Re-evaluations also may be appropriate for patients who received therapy treatment prior to surgery and then returned for additional rehabilitation after surgery. The catch in this situation is that some commercial payers may consider the post-op treatment period a new episode of care, in which case you’d need to use an e...
Popular Posts:
- 1. icd 10 code for clogged tear duct
- 2. 2019 icd 10 code for lumbago
- 3. icd 10 code for leukocytes in urine
- 4. icd 10 code for apertognathia
- 5. whats the f for in the icd code
- 6. in icd-10-cm, what is the default code for coronary artery atherosclerosis?
- 7. 2019 icd 10 cm code for chest pain
- 8. icd 10 code for testoserone
- 9. icd 10 code for thrombocythemia
- 10. icd 10 cm code for neck nodule