What is the treatment for pressure ulcer?
- Patient should be repositioned with consideration to the individual’s level of activity, mobility and ability to independently reposition. ...
- Keep the skin clean and dry.
- Avoid massaging bony prominences.
- Provide adequate intake of protein and calories.
- Maintain current levels of activity, mobility and range of motion.
What are the risk factors of pressure ulcer?
Bedsores (pressure ulcers)
- Overview. Bedsores — also called pressure ulcers and decubitus ulcers — are injuries to skin and underlying tissue resulting from prolonged pressure on the skin.
- Symptoms. Bedsores fall into one of several stages based on their depth, severity and other characteristics. ...
- Causes. ...
- Risk factors. ...
- Complications. ...
- Prevention. ...
Do you know these 10 risk factors for pressure ulcers?
Risk factors include: Immobility. This might be due to poor health, spinal cord injury and other causes. Incontinence. Skin becomes more vulnerable with extended exposure to urine and stool. Lack of sensory perception. Spinal cord injuries, neurological disorders and other conditions can result in a loss of sensation.
What is the cost of pressure ulcer?
What are the Cost Implications of Pressure Ulcers? Pressure ulcers are the single most costly chronic wound in the NHS, costing around £3.8 million per day 1 while the incremental cost of treating a pressure ulcer is up to £374 per day 2. A Category IV pressure ulcer as an example costs £16,000 to treat 3.

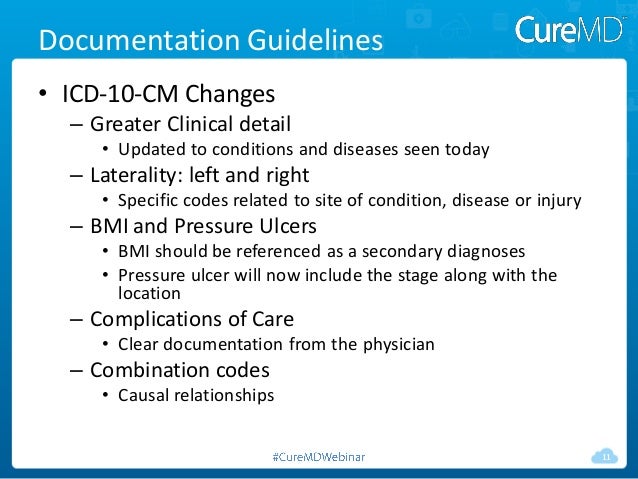
What is the ICD-10 code for pressure ulcers?
Pressure ulcer of unspecified site, unspecified stage L89. 90 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM L89. 90 became effective on October 1, 2021.
How do you code a Pressure ulcer?
“Two codes are needed to completely describe a pressure ulcer: A code from subcategory 707.0, Pressure ulcer, to identify the site of the pressure ulcer and a code from subcategory 707.2, Pressure ulcer stages.
What is L89 90?
90: Decubitus ulcer, stage unspecified Head.
What is the ICD-10 code for Stage 2 sacral ulcer?
ICD-10 code L89. 152 for Pressure ulcer of sacral region, stage 2 is a medical classification as listed by WHO under the range - Diseases of the skin and subcutaneous tissue .
How do you code a deep tissue injury?
The new codes for deep-tissue injury, which specify the affected body part and laterality, include codes such as:L89. 126, pressure-induced deep tissue damage of left upper back.L89. 156, pressure-induced deep tissue damage of sacral region.
What is the ICD-10 code for infected decubitus ulcer?
L89. 159 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is a decubitus ulcer?
Listen to pronunciation. (deh-KYOO-bih-tus UL-ser) Damage to an area of the skin caused by constant pressure on the area for a long time. This pressure can lessen blood flow to the affected area, which may lead to tissue damage and tissue death.
What is the ICD-10 code for deconditioning?
Deconditioning=diminished ability or perceived ability to perform tasks involved in person's usual activities of daily living. 728.2=Use this code for muscle wasting and atrophy due to disuse, where the condition is not classified elsewhere.
What are pressure ulcers?
Pressure ulcers (also known as pressure sores or bedsores) are injuries to the skin and underlying tissue, primarily caused by prolonged pressure on the skin. They can happen to anyone, but usually affect people confined to bed or who sit in a chair or wheelchair for long periods of time.
How do you code an Unstageable pressure ulcer?
Assignment of the ICD-10 code for unstageable pressure ulcer (L89. 000) should be based on the clinical documentation.
How do you treat Stage 2 pressure ulcers?
Stage II pressure sores should be cleaned with a salt water (saline) rinse to remove loose, dead tissue. Or, your provider may recommend a specific cleanser. Do not use hydrogen peroxide or iodine cleansers. They can damage the skin.
How many codes are required to code a pressure ulcer site and stage?
If a patient is admitted to an inpatient hospital with a pressure ulcer at one stage and it progresses to a higher stage, 2 separate codes should be assigned: 1 code for the site and stage of the ulcer on admission and a second code for the same ulcer site and the highest stage reported during the stay.
What is pressure ulcer?
Pressure ulcers are areas of damaged skin and tissue developing as a result of compromised circulation. When a patient stays in one position without movement, the weight of the bones against the skin inhibits circulation and causes an ulceration of the tissue. Pressure ulcers usually form near the heaviest bones (buttocks, hips, and heels).
What is the sequence of a pressure ulcer?
The sequence depends on the pressure ulcer being treated. If all the pressure ulcers are being treated, sequence the code for the most severe pressure ulcer first. Example: A patient with a stage 3 pressure ulcer on her left heel and a stage 2 pressure ulcer of her left hip is scheduled for debridement.
What is an unstageable ulcer?
An unstageable ulcer is when the base of the ulcer is covered in eschar or slough so much that it cannot be determined how deep the ulcer is. This diagnosis is determined based on the clinical documentation. This code should not be used if the stage is not documented.
Where do pressure ulcers form?
Pressure ulcers usually form near the heaviest bones (buttocks, hips, and heels). There are stages of pressure ulcers that identify the extent of the tissue damage. Stage 1—Persistent focal erythema. Stage 2—Partial thickness skin loss involving epidermis, dermis, or both.
Can a pressure ulcer get worse?
If the pressure ulcer is healed completely , a code is not reported for the pressure ulcer. There are some cases where the pressure ulcer will get worse during the course of the admission. For example, the patient is admitted for treatment of a stage 2 ulcer that progresses to stage 3.
Popular Posts:
- 1. what is the correct icd-10-pcs code for wedge resection
- 2. icd 10 code for anemiadvt
- 3. icd 10 code for encounter for aftercare skeletal surgery
- 4. icd 10 cm code for renal cyst
- 5. icd 10 code for maloculing
- 6. icd 10 code for acute eub of right foot pain
- 7. icd 10 code for sprain upper back
- 8. what is the icd 10 code for 599.70
- 9. icd 10 code for streptococcus gallolyticus bacteremia
- 10. icd 10 code for tubal ligation with cesarean section