Coding Information:
- HCPCS code J0897 should be used to report denosumab (Prolia™, Xgeva™) for claims submitted to the Part A and Part B MAC.
- The administration of denosumab, when billed, should be billed using the therapeutic administration code 96372...
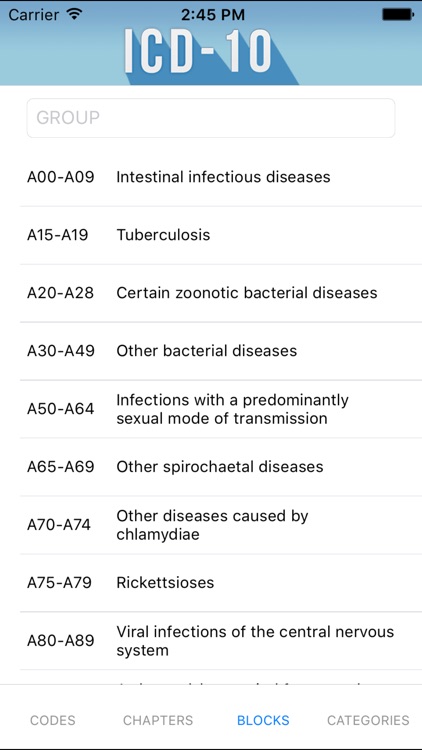
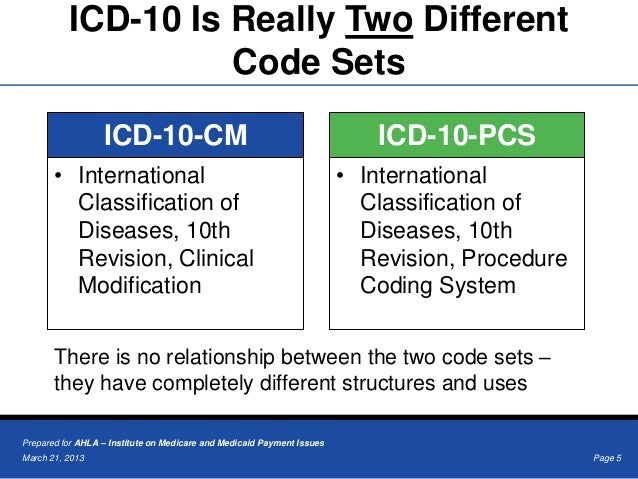
- Correct coding requires that a bone metastasis diagnosis (ICD-10-CM code C79.51) be present on the claim as the...
What is the ICD 10 code for POA exempt?
2016 2017 2018 2019 2020 2021 Billable/Specific Code POA Exempt Z79.899 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2021 edition of ICD-10-CM Z79.899 became effective on October 1, 2020.
What is the latest version of the ICD 10 for 2019?
The 2019 edition of ICD-10-CM Z79.899 became effective on October 1, 2018. This is the American ICD-10-CM version of Z79.899 - other international versions of ICD-10 Z79.899 may differ.
What is the ICD 10 code for billing and coding?
In Group 4, ICD-10 code N18.3 has been deleted and replaced with N18.30, N18.31 and N18.32. The descriptor for ICD-10 code Z88.8 was changed in Group 4. This article was converted to the new Billing and Coding Article format.
How do you administer denosumab Prolia?
Denosumab (Prolia™) is supplied in a single-use prefilled syringe with a safety guard or in a single-use vial. Denosumab (Xgeva™) is administered at a dose of 120mg every four weeks as a subcutaneous injection in the upper arm, upper thigh, or abdomen for bone metastasis from solid tumors.
What is the HCPCS code for Prolia?
What is the ICD-10 code for hypercalcemia of malignancy?
What is the ICd 10 code for bone metastasis?
About this website
What diagnosis covers Prolia?
Prolia® is indicated for the treatment of postmenopausal women with osteoporosis at high risk for fracture, defined as a history of osteoporotic fracture, or multiple risk factors for fracture; or patients who have failed or are intolerant to other available osteoporosis therapy.
What is the ICD 10 code for long term use of Prolia?
Long term (current) use of bisphosphonates The 2022 edition of ICD-10-CM Z79. 83 became effective on October 1, 2021.
What is the code for Prolia?
Prolia® (Denosumab – J0897) Administration.
What is Prolia used for?
Denosumab injection (Prolia) is used to treat bone loss in men who are being treated for prostate cancer with certain medications that cause bone loss, to treat bone loss in women with breast cancer who are receiving certain medications that increase their risk for fractures.
How do I bill for a Prolia injection?
We bill the admin code of 96401 with J0897, because Prolia is a biologic---and the 96401 is the appropriate code for that category of drug. That also means that your reimbursement would be greater for the admin because of the risks/side effects for biologics.
What is the diagnosis code for long term medication use?
Other long term (current) drug therapy Z79. 899 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z79. 899 became effective on October 1, 2021.
What is ICD 10 code for osteoporosis?
0 – Age-Related Osteoporosis without Current Pathological Fracture. ICD-Code M81. 0 is a billable ICD-10 code used for healthcare diagnosis reimbursement of Age-Related Osteoporosis without Current Pathological Fracture.
What is procedure code J0897?
Drugs that have the ingredient denosumab are billed using HCPCS code J0897, if all existing guidelines for coverage under the home health benefit are met. HCPCS code J0897 is defined as 1 mg.
Does Medicare pay for Prolia for osteoporosis?
Denosumab (Prolia) is used to treat osteoporosis in women after menopause and in men. This drug is more popular than comparable drugs. There are currently no generic alternatives to Prolia. It is covered by most Medicare and insurance plans, but some pharmacy coupons or cash prices may be lower.
How often do you get a Prolia injection?
Compared to other osteoporosis treatments, only Prolia® is 1 shot every 6 months. You should take calcium and vitamin D as your doctor tells you to while you receive Prolia®.
How long can you take Prolia for osteoporosis?
In studies, people have safely taken Prolia for up to 8 years. If the drug is working to improve your condition, your doctor may have you take it long term. They'll discuss with you the long-term benefits of Prolia and how long you should continue treatment.
How many Prolia shots are required?
The dosage frequency of Prolia is one injection every 6 months. If you have other questions about receiving your Prolia injections, talk with your doctor.
What is ICD-10 code for osteoporosis?
0 – Age-Related Osteoporosis without Current Pathological Fracture. ICD-Code M81. 0 is a billable ICD-10 code used for healthcare diagnosis reimbursement of Age-Related Osteoporosis without Current Pathological Fracture.
Does Medicare pay for Prolia for osteoporosis?
Denosumab (Prolia) is used to treat osteoporosis in women after menopause and in men. This drug is more popular than comparable drugs. There are currently no generic alternatives to Prolia. It is covered by most Medicare and insurance plans, but some pharmacy coupons or cash prices may be lower.
What is E83 52?
ICD-10 code E83. 52 for Hypercalcemia is a medical classification as listed by WHO under the range - Endocrine, nutritional and metabolic diseases .
What is procedure code J0897?
HCPCS code J0897 for Injection, denosumab, 1 mg as maintained by CMS falls under Drugs, Administered by Injection .
Prolia Injections -Billed J0897 with 96372 or 96401 - AAPC
Billing J0897 for Diagnosis code M810. Is the proper administration code 96372 or 96401. Received various answers in reference to which administration code is the correct code to us for J0897. Apparently UHC-Medicare wants us to us 96372. I received information the Medicare will accept 96401...
Does Medicare Cover Prolia? | Medicare Prescription Drug Coverage
Prolia ®; Chemical name: Denosumab Typical dosage: 60mg/ml Typical type: Injection 1 Prolia ® is typically used to help treat osteoporosis in men and in women who are at increased risk for weakened bones after menopause. It can also be used to help treat bone loss in cancer patients who are receiving treatment for prostate cancer (men) or breast cancer (women).
Does Your Medicare Insurance Plan Cover Prolia?
Osteoporosis is a common condition in the United States. Over 10 million people have osteoporosis, and 44 million have bone density levels that are well
CPT code J0897 - Prolia Injection new J code - Medical billing cpt ...
New CPT code for Prolia injection effective from 2012. Please go through the below update . *Beginning January 1, 2012, a new HCPCS procedure code has been assigned to the drug denosumab. J0897 Injection, denosumab, 1 mg The drug denosumab has two brand names with two different indications. The brand…
Prolia® (denosumab) | Paying for Treatment
Nearly 77% of Medicare Part B Prolia ® patients have supplemental insurance ‡ and pay $0 § out-of-pocket every six months. The remaining 23% of Medicare Part B Prolia ® patients pay up to $212.99 §, ** out-of-pocket every six months depending on the patient's selected Part B plan. Patients pay for Prolia® twice per year. These data do not include out-of-pocket costs related to office ...
When will the ICd 10 Z79.899 be released?
The 2022 edition of ICD-10-CM Z79.899 became effective on October 1, 2021.
What is a Z77-Z99?
Z77-Z99 Persons with potential health hazards related to family and personal history and certain conditions influencing health status
When will the ICd 10 Z79.810 be released?
The 2022 edition of ICD-10-CM Z79.810 became effective on October 1, 2021.
What is a Z77-Z99?
Z77-Z99 Persons with potential health hazards related to family and personal history and certain conditions influencing health status
What is Prolia used for?
Prolia® is a prescription medicine used to treat osteoporosis (thinning and weakening of bone) in women after menopause who are at high risk for fracture, meaning women who have had a fracture related to osteoporosis, or who have multiple risk factors for fracture. [1]
Why would this drug ever be reported using 96401?
You may ask, why would this drug ever be reported using 96401? A coding “hint” that alerts us is the suffix “-mab,” which tells us the drug is a mono clonal antibody . We learn from CMS that administration monoclonal antibodies are reported with the chemotherapy administration code 96401.
Is 96401 a coding question?
We each looked up other payer guidance and found that one recommends reporting 964011 or 96372. Most payers agree with CMS and instruct us to report 96401.
Where to administer Prolia?
Administer Denosumab (Prolia™) via subcutaneous injection in the upper arm, the upper. thigh, or the abdomen. Denosumab (Prolia™) is supplied in a single-use prefilled syringe with a safety guard or in a single-use vial.
Why was Prolia developed?
Prolia was developed as a result of a scientific understanding of how bones stay strong.
Is denosumab approved by Medicare?
The FDA has approved the use of denosumab (PROLIA™) and (Xgeva™). Medicare has determined under Section 1861 (t) that this drug may be paid when it is administered incident to a physician’s service and is determined to be reasonable and necessary.
Is Prolia approved for multiple myeloma?
Limitations: • Denosumab (PROLIA™) is contraindicated in patients with hypocalcemia. • Denosumab (PROLIA™) is contraindicated in patients with pregnancy. • Denosumab (Xgeva™) is not approved for patients with multiple myeloma or other cancers of the blood. Coding Guidelines:
What is the HCPCS code for ustekinumab?
J3358: Effective September 23, 2016, IV ustekinumab (Stelara®) should be billed with HCPCS J3590 (OPPS: C9399 for dates of service (DOS) before 04/01/2017; C9487 for DOS from 04/01/2017 to 06/30/17, Q9989 for DOS from 07/01/2017-12/31/17 and J3358 for DOS 01/01/2018 and after) for the initial IV dose of Stelara® when used for Crohn’s disease and Ulcerative Colitis and each subsequent subcutaneous dose must be billed with J3357. This IV formulation is now FDA approved for Crohn’s disease and Ulcerative Colitis. On and after July 31, 2017, both the drug and administration should be billed on the same claim with no other drugs or administration to prevent inappropriate claim rejection.
What is the CPT code for chemotherapy?
The Current Procedural Terminology (CPT) codebook contains the following information and direction for the Chemotherapy and Other Highly Complex Drug or Highly Complex Biological Agent Administration CPT® codes: “Chemotherapy Administration codes 96401-96549 apply to parenteral administration of non-radionuclide anti-neoplastic drugs; and also to anti-neoplastic agents provided for treatment of non-cancer diagnoses (e.g. cyclophosphamide for auto-immune conditions) or to substances such as certain monoclonal antibody agents, and other biologic response modifiers. The highly complex infusion of chemotherapy or other drug or biologic agents requires physician or other qualified health care professional work and/or clinical staff monitoring well beyond that of therapeutic drug agents (96360-96379) because the incidence of severe adverse patient reactions are typically greater. These services can be provided by any physician or other qualified health care professional. Chemotherapy services are typically highly complex and require direct supervision for any or all purposes of patient assessment, provision of consent, safety oversight, and intraservice supervision of staff. Typically, such chemotherapy services require advanced practice training and competency for staff who provide these services; special considerations for preparation, dosage, or disposal; and commonly, these services entail significant patient risk and frequent monitoring. Examples are frequent changes in the infusion rate, prolonged presence of the nurse administering the solution for patient monitoring and infusion adjustments, and frequent conferring with the physician or other qualified health care professional about these issues. When performed to facilitate the infusion of injection, preparation of chemotherapy agent (s), highly complex agent (s), or other highly complex drugs is included and is not reported separately. To report infusions that do not require this level of complexity, see 96360-96379. Codes 96401-96402, 96409-96425, 96521-96523 are not intended to be reported by the individual physician or other qualified health care professional in the facility setting.”
What is the HCPCS code for octreotide acetate?
The subcutaneous or intravenous formulation of octreotide acetate is billed using HCPCS code J2354 with the JA (intravenous) or JB (subcutaneous) modifier.
What is the JB modifier for filgrastim?
J1442, Q5101 or Q5110: The subcutaneous or intravenous formulation of filgrastim needs to billed with the JA (intravenous) or JB (subcutaneous) modifier.
When is the JW modifier not permitted?
A situation in which the JW modifier is not permitted is when the actual dose of the drug or biological administered is less than the billing unit. For example, one billing unit for a drug is equal to 10mg of the drug in a single use vial. A 7mg dose is administered to a patient while 3mg of the remaining drug is discarded. The 7mg dose is billed using one billing unit that represents 10mg on a single line item. The single line item of 1 unit would be processed for payment of the total 10mg of drug administered and discarded. Billing another unit on a separate line item with the JW modifier for the discarded 3mg of drug is not permitted because it would result in overpayment. Therefore, when the billing unit is equal to or greater than the total actual dose and the amount discarded , the use of the JW modifier is not permitted.
Can you add 96367 to Medicare?
To avoid unnecessary rejections; claims for chemotherapy drugs and their chemotherapy administration should be billed as a pair on a separate claim. In this circumstance, the Medicare Claims Processing System will still allow the add-on codes 96367 and 96368 if billed appropriately on a separate claim from the initial claim for the chemotherapy drug and administration codes with the same date of service.
Is Medicare coverage italicized?
Language quoted from Centers for Medicare and Medicaid Services (CMS), National Coverage Determinations (NCDs) and coverage provisions in interpretive manuals is italicized throughout the policy.
What is the HCPCS code for Prolia?
HCPCS code J0897 should be used to report denosumab (Prolia™, Xgeva™) for claims submitted to the Part A and Part B MAC.
What is the ICD-10 code for hypercalcemia of malignancy?
For management of hypercalcemia of malignancy (ICD-10-CM code E83.52)
What is the ICd 10 code for bone metastasis?
Correct coding requires that a bone metastasis diagnosis (ICD-10-CM code C79.51) be present on the claim as the primary diagnosis and the original cancer or history of cancer be included as the secondary diagnosis. This article does not limit the primary cancer (as long as it is a solid tumor and not a myeloma or other cancer of the blood). Effective for dates of service on or after 01/04/2018, the FDA has approved denosumab (Xgeva®) for the treatment of skeletal-related events in patients with multiple myeloma.
Popular Posts:
- 1. icd 10 code for esbl klebsiella
- 2. what is the icd 10 code for posttussive sncope
- 3. icd 10 code for herniated cervical disc with radiculopathy c5-6
- 4. icd 10 code for ckd mbd
- 5. icd 10 code for diff ambulation difficulty
- 6. icd 10 pcs code for laparotomy with peritoneal biopsy
- 7. what is the icd 10 code for ra
- 8. icd 10 code for borderline type 2 diabetes mellitus
- 9. icd 10 code for urine straight cath
- 10. icd 10 code for factor 8