What is the secondary code for Chapter 20?
When will the ICd 10 T84.53XA be released?
About this website
What is the ICD-10-CM code for knee surgery?
ICD-10: Z96. 651, Status (post), organ replacement, by artificial or mechanical device or prosthesis of, joint, knee-see presence of knee joint implant. ICD-10: R26.
What is the ICD-10 code for right knee arthroscopy?
In ICD-10-PCS, arthroscopy goes to the root operation “inspection,” which is defined as visually and/or manually exploring a body part. Therefore, an arthroscopy of the right knee is classified to code 0SJC4ZZ, and arthroscopy of the left knee is classified to code 0SJD4ZZ.
What is the ICD-10 code for status post left knee arthroplasty?
652.
What is the code for infection due to the presence of a right knee joint prosthesis subsequent encounter?
T84. 53XA - Infection and inflammatory reaction due to internal right knee prosthesis [initial encounter].
How do you code a knee arthroscopy?
Report HCPCS code G0289 per compartment to Medicare or private payers that require this code if arthroscopic knee procedures other than a meniscectomy are performed at the same operative session, same knee.
What is the ICD 10 code for right total knee arthroplasty?
Z96. 651 - Presence of right artificial knee joint. ICD-10-CM.
When do you use ICD-10 Z47 89?
ICD-10 code Z47. 89 for Encounter for other orthopedic aftercare is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is diagnosis code Z98 890?
ICD-10 code Z98. 890 for Other specified postprocedural states is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is the ICD-10 code for status post surgery?
ICD-10-CM Code for Encounter for surgical aftercare following surgery on specified body systems Z48. 81.
What is the ICD-10 code for right knee infection?
ICD-10 Code for Direct infection of right knee in infectious and parasitic diseases classified elsewhere- M01. X61- Codify by AAPC.
What is the ICD-10 code for prosthetic joint infection?
T84. 50XA - Infection and inflammatory reaction due to unspecified internal joint prosthesis [initial encounter] | ICD-10-CM.
Which of the following is a periprosthetic joint infection?
Periprosthetic joint infection (PJI) is one of the most devastating and costly complications following total joint arthroplasty (TJA). Diagnosis and management of PJI is challenging for surgeons.
What is the ICD 10 code for left TKA infection?
ICD-10-CM Code for Infection and inflammatory reaction due to internal left knee prosthesis, initial encounter T84. 54XA.
What is the ICD 10 code for right knee swelling?
461 - Effusion, right knee.
What is the ICD 10 code for septic joint?
ICD-10-CM M00. 849 is grouped within Diagnostic Related Group(s) (MS-DRG v39.0): 548 Septic arthritis with mcc. 549 Septic arthritis with cc.
What causes knee infection?
Knee infections happen when harmful bacteria contaminates the fluid that lubricates your knee joint. While most anyone can develop one, you hold a higher risk if you have an inflammatory condition like arthritis, a traumatic injury involving your knee, or a compromised immune system.
2022 ICD-10-CM Code T84.53XA - Infection and inflammatory reaction due ...
T84.53XA is a billable diagnosis code used to specify a medical diagnosis of infection and inflammatory reaction due to internal right knee prosthesis, initial encounter. The code T84.53XA is valid during the fiscal year 2022 from October 01, 2021 through September 30, 2022 for the submission of HIPAA-covered transactions.
Search Page 1/20: RIGHT TOTAL KNEE ARTHROPLASTY REVISION - ICD10Data.com
Search Results. 500 results found. Showing 1-25: ICD-10-CM Diagnosis Code Z96.651. [convert to ICD-9-CM]
2022 ICD-10-CM Diagnosis Code T84.53XD
Free, official coding info for 2022 ICD-10-CM T84.53XD - includes detailed rules, notes, synonyms, ICD-9-CM conversion, index and annotation crosswalks, DRG grouping and more.
2022 ICD-10-CM Code M01.X61 - Direct infection of right knee in ...
M01.X61 is a billable diagnosis code used to specify a medical diagnosis of direct infection of right knee in infectious and parasitic diseases classified elsewhere. The code M01.X61 is valid during the fiscal year 2022 from October 01, 2021 through September 30, 2022 for the submission of HIPAA-covered transactions.
M01.X61 - ICD-10-CM Direct infct of r knee in infec/parastc dis classd ...
M01.X61 is a valid billable ICD-10 diagnosis code for Direct infection of right knee in infectious and parasitic diseases classified elsewhere.It is found in the 2022 version of the ICD-10 Clinical Modification (CM) and can be used in all HIPAA-covered transactions from Oct 01, 2021 - Sep 30, 2022.. ↓ See below for any exclusions, inclusions or special notations
What is the cap of the knee called?
Knee is one of the biggest joint in body which joints thigh bone (femur) and lower leg joint (tibia). The knee cap is called patella. Tendons (flexible connective tissue) and ligaments (inelastic collagen tissue) help joining these bones and make the knee joint.
What tests are needed for knee joint swelling?
There may be need of radiological tests (X-ray, CT, MRI, ultrasound) or arthrocentesis (lab analysis of knee joint fluid) for further evaluation to check for infections or injury to tendon or ligament.
Why does my knee hurt so bad?
Knee pain can be mild, moderate or severe. The reasons for pain can vary such as injury, overuse, infection and inflammation. Sometimes there may be swelling and redness depends on the cause. We need to visit doctor as per the severity and as per how long the pain lasts.
Is knee pain a symptom?
Knee pain is a symptom; hence follow ICD coding guideline of not coding signs and symptoms when there is a definitive diagnosis made.
Can you code knee pain?
Review the entire medical record thoroughly especially physical examination to determine the correct anatomical site of pain. Do not code unspecified knee pain if there is any site specification mentioned in the record.
Is Hoffa's syndrome a bilateral ICd 10?
Hoffa’s syndrome is not coded as it is mentioned as “possible”.
What is PJI in medical?
The diagnosis of prosthetic joint infections (PJI) poses a significant challenge since real evidence-based guidelines to aid clinicians in choosing the most accurate diagnostic strategy are lacking. Despite a significant amount of basic and clinical research in this field, many questions pertaining to the definition of infection as well as diagnosis and management of these infections remains unanswered. Clinical practice guidelines for the diagnosis and management of PJI have been proposed by a number of organizations, including the 2021 European Bone and Joint Infection Society (EBJIS) criteria, the 2018 International Consensus Meeting (ICM) criteria, the 2013 ICM criteria, the 2013 Infectious Disease Society of America guidelines (IDSA), and the 2011 Infection Society (MSIS) criteria. These guidelines stress the importance of using a multi-disciplinary approach to aid in the diagnosis of PJI, requiring supporting evidence from clinical examination, laboratory results, microbiological culture identification, histological interpretation, and intraoperative findings. These guidelines are meant to serve as an educational tool designed to assist practitioners in providing appropriate care for patients. It is anticipated that consideration of these guidelines may help reduce morbidity, mortality and the costs associated with PJI.
When suspected prosthetic joint infection is not clinically apparent, Sedimentation Rate or C-Reactive Protein?
When suspected prosthetic joint infection is not clinically apparent, Sedimentation rate or C-reactive protein (CRP) tests should be performed.
How long does it take for a pji to develop?
The classification scheme useful for identification of PJI is simply based on the time to infection, classified as early, delayed, or late onset. Early onset PJI occurs less than three months after the last surgery. These infections are most commonly initiated at the time of operation, through intraoperative contamination, and are usually caused by relatively virulent microorganisms. Delayed onset PJI occurs after 3 months but before 12 or 24 months. Different authors have used different time points to differentiate between delayed and late onset PJIs. However, regardless of the cutoff used, the common theme is that these infections are also typically acquired at the time of surgery but are caused by less virulent microorganisms such that the overt presentation of infections does not occur within the first 3 months. Late onset PJI, usually occurs 12-24 months after surgery and is likely due to a hematogenous infection but may also be due to extremely indolent infection initiated at the time of surgery.
What is biofilm in prosthetic joints?
The pathogenesis of prosthetic joint infections by pathogens is dependent on the formation of biofilm. Biofilms are complex communities of microorganisms embedded in an extracellular matrix that forms on surfaces. Pathogens will adhere to orthopedic hardware, and proliferate with elaboration of exopolysaccharides known as glycocalyx, which after a certain period, will coalesce into biofilm. This biofilm microenvironment serves as a barrier that renders host defenses and antimicrobials less effective. Complicating matters further, pathogens hidden deep in the biofilm have characteristic indolent low metabolic rate which also prevent accurate culture identification. Together, S. epidermis, S. aureus and Pseudomonas aeruginosa make up almost 75% of the biofilms found in medical devices. S. aureus and Staphylococcus epidermis are the most common biofilm-forming bacteria.
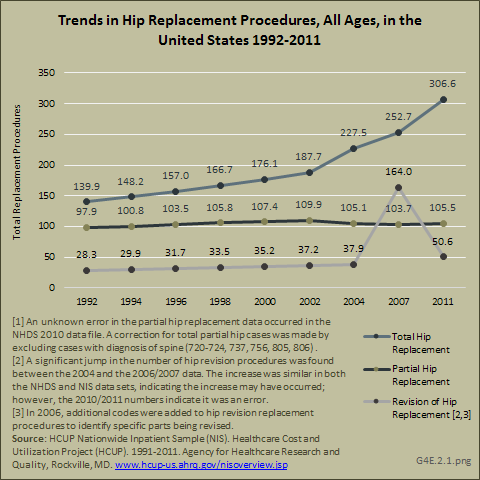
How many hip and knee arthroplasties are performed annually?
It is estimated that 3,481,000 primary total knee and 572,000 primary total hip arthroplasties will be performed annually in the US by 2030. With the increase in prosthetic joint implantations, serious complications of prosthetic joint infections (PJI) of the hip and knee is also on the rise.
Is a culture positive for prosthetic joint infection?
Cultures are more likely to be positive for early-onset prosthetic joint infection.
Purpose
To determine the positive predictive values (PPVs) of ICD-9, ICD-10, and Current Procedural Terminology (CPT)-based diagnostic coding algorithms to identify prosthetic joint infection (PJI) following knee arthroplasty (TKA) within the United States Veterans Health Administration.
Methods
We identified patients with: 1) hospital discharge ICD-9 or ICD-10 diagnosis of PJI, 2) ICD-9, ICD-10, or CPT procedure code for TKA prior to PJI diagnosis, 3) CPT code for knee X-ray within ±90 days of the PJI diagnosis, and 4) at least 1 CPT code for arthrocentesis, arthrotomy, blood culture, or microbiologic procedure within ±90 days of the PJI diagnosis date.
Conclusions
An algorithm consisting of an ICD-9 or ICD-10 PJI diagnosis following a TKA code combined with CPT codes for a knee X-ray and either a relevant surgical procedure or microbiologic culture yielded a PPV of 75.0% (ICD-9) and 85.0% (ICD-10), for confirmed PJI events and could be considered for use in future pharmacoepidemiologic studies.
What is the secondary code for Chapter 20?
Use secondary code (s) from Chapter 20, External causes of morbidity, to indicate cause of injury. Codes within the T section that include the external cause do not require an additional external cause code. Type 1 Excludes.
When will the ICd 10 T84.53XA be released?
The 2022 edition of ICD-10-CM T84.53XA became effective on October 1, 2021.
Popular Posts:
- 1. icd 10 code for cervical length in pregnancy
- 2. icd 10 code for extremity edema of hands
- 3. what is the icd 10 code for coumadin therapy
- 4. icd 10 code for sacral pressure ulcer stage 1
- 5. icd 9 code for foreign body
- 6. icd 10 code for pontine infarct
- 7. icd 10 code for orif r hip history
- 8. icd 10 code for otitis
- 9. icd-10 code for std counseling
- 10. icd 10 code for basal cell ca left ear