What can cause respiratory distress in newborns?
You can help prevent many respiratory infections by taking these steps:
- Do not smoke around your child or in places that he goes, even when he is not there. ...
- Keep places where your child will be dust-free.
- Do not use baby powder or cornstarch on your child. ...
- Everyone should practice good hand washing to prevent the spread of germs.
- If possible, keep your child away from people who are sick.
What is respiratory disorder in the neonate?
There are other less common but equally serious neonatal respiratory diseases:
- Congenital bronchiectasis. Airway inflammation caused by an infection.
- Pulmonary hypoplasia. A congenital anomaly that causes incomplete lung development.
- Congenital pneumonia. An inflammation of the lung tissue not caused by infections.
What does respiratory distress syndrome, newborn mean?
Newborn respiratory distress syndrome (NRDS) happens when a baby's lungs are not fully developed and cannot provide enough oxygen, causing breathing difficulties. It usually affects premature babies. It's also known as infant respiratory distress syndrome, hyaline membrane disease or surfactant deficiency lung disease.
Is My Baby in distress?
Your water breaks and is greenish-brown (that’s baby’s first poop; some babies who pass this meconium while still in the uterus may be in distress) The only way to know for sure that your baby’s in fetal distress is with a continuous fetal monitor, performing a nonstress test or with an ultrasound and performing a biophysical profile.

What is the ICD 10 code for resp distress?
ICD-10-CM Code for Acute respiratory distress R06. 03.
What is the diagnosis code for acute respiratory distress syndrome idiopathic type I in a newborn?
P22. 0 - Respiratory distress syndrome of newborn | ICD-10-CM.
What indicates respiratory distress in newborns?
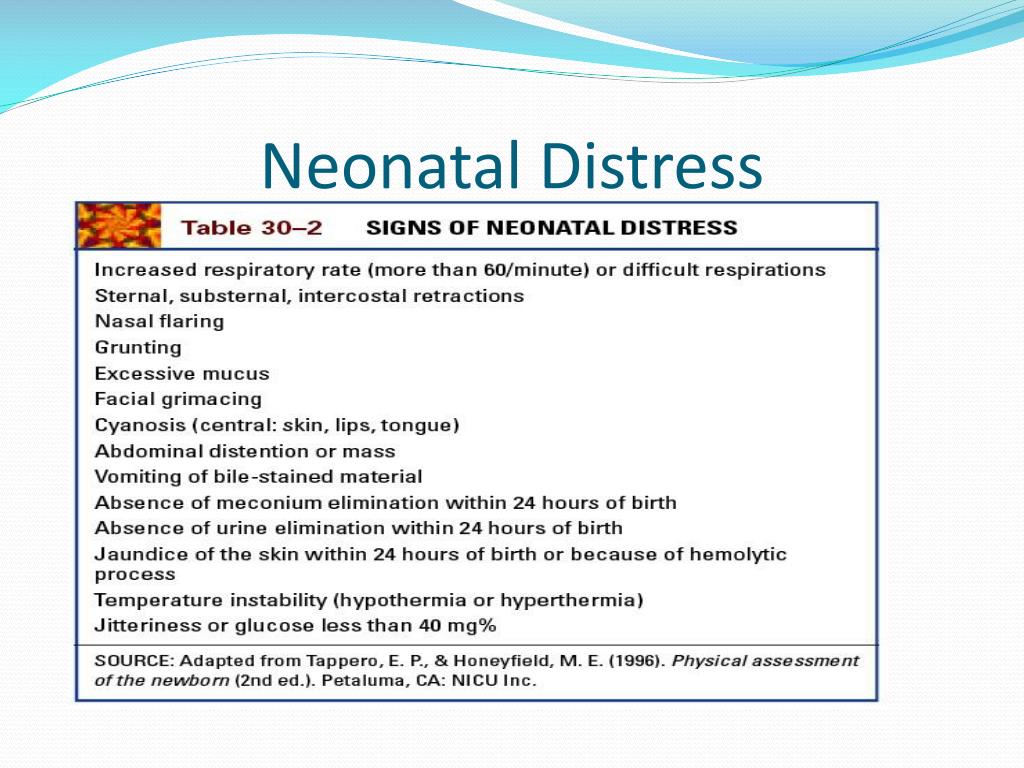
Newborns with respiratory distress commonly exhibit tachypnea with a respiratory rate of more than 60 respirations per minute. They may present with grunting, retractions, nasal flaring, and cyanosis.
What is the code for respiratory failure of newborn?
ICD-10-CM Code for Respiratory failure of newborn P28. 5.
Can F07 81 be used as a primary diagnosis?
Our physicians have used IDC-10 code F07. 81 as the primary diagnosis for patients presenting with post concussion syndrome.
What is diagnosis code H90 3?
ICD-10 code: H90. 3 Sensorineural hearing loss, bilateral.
What is the difference between respiratory distress and respiratory distress syndrome?
One form of respiratory distress is acute respiratory distress syndrome (ARDS), which causes fluid to build up in the lungs, inhibiting breathing and the transfer of oxygen into the bloodstream. ARDS usually develops in patients who are already dealing with another disease or serious injury.
What are the five symptoms of respiratory distress in the newborn?
Babies who have RDS may show these signs:Fast breathing very soon after birth.Grunting “ugh” sound with each breath.Changes in color of lips, fingers and toes.Widening (flaring) of the nostrils with each breath.Chest retractions - skin over the breastbone and ribs pulls in during breathing.
What are four signs of respiratory distress?
Signs of Respiratory DistressBreathing rate. An increase in the number of breaths per minute may mean that a person is having trouble breathing or not getting enough oxygen.Color changes. ... Grunting. ... Nose flaring. ... Retractions. ... Sweating. ... Wheezing. ... Body position.
What is the ICD-10 code for neonatal hypoglycemia?
4.
What is respiratory distress syndrome?
A respiratory distress syndrome in newborn infants, usually premature infants with insufficient pulmonary surfactants. The disease is characterized by the formation of a hyaline-like membrane lining the terminal respiratory airspaces (pulmonary alveoli) and subsequent collapse of the lung (pulmonary atelectasis).
What is cyanosis in babies?
A condition of the newborn marked by dyspnea with cyanosis, most frequently occurring in premature infants, children of diabetic mothers and infants delivered by cesarean section, and sometimes with no predisposing cause. A respiratory distress syndrome in newborn infants, usually premature infants with insufficient pulmonary surfactants.
What is the ICd 10 code for respiratory distress?
Respiratory distress of newborn 1 P22 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail. 2 The 2021 edition of ICD-10-CM P22 became effective on October 1, 2020. 3 This is the American ICD-10-CM version of P22 - other international versions of ICD-10 P22 may differ.
What is cyanosis in babies?
A condition of the newborn marked by dyspnea with cyanosis, most frequently occurring in premature infants, children of diabetic mothers and infants delivered by cesarean section, and sometimes with no predisposing cause. asphyxia from carbon monoxide ( T58.-) asphyxia from inhalation of food or foreign body ( T17.-)
What is respiratory distress in newborns?
Respiratory distress of newborn P22- 1 A condition of the newborn marked by dyspnea with cyanosis, heralded by such prodromal signs as dilatation of the alae nasi, expiratory grunt, and retraction of the suprasternal notch or costal margins, most frequently occurring in premature infants, children of diabetic mothers, and infants delivered by cesarean section, and sometimes with no apparent predisposing cause. 2 A condition of the newborn marked by dyspnea with cyanosis, heralded by such prodromal signs as dilatation of the alae nasi, expiratory grunt, and retraction of the suprasternal notch or costal margins, mostly frequently occurring in premature infants, children of diabetic mothers, and infants delivered by cesarean section, and sometimes with no apparent predisposing cause. 3 A condition of the newborn marked by dyspnea with cyanosis, most frequently occurring in premature infants, children of diabetic mothers and infants delivered by cesarean section, and sometimes with no predisposing cause.
What is the code for cyanosis?
Codes. P22 Respiratory distress of newborn. P22.0 Respiratory distress syndrome of newborn.
What is cyanosis in newborns?
A condition of the newborn marked by dyspnea with cyanosis, heralded by such prodromal signs as dilatation of the alae nasi, expiratory grunt, and retraction of the suprasternal notch or costal margins, most frequently occurring in premature infants, children of diabetic mothers, and infants delivered by cesarean section, and sometimes with no apparent predisposing cause.
What is the ICD code for respiratory distress of newborn?
ICD Code P22 is a non-billable code. To code a diagnosis of this type, you must use one of the four child codes of P22 that describes the diagnosis 'respiratory distress of newborn' in more detail. P22 Respiratory distress of newborn. NON-BILLABLE.
How many babies die from IRDS?
IRDS affects about 1% of newborn infants and is the leading cause of death in preterm infants. The incidence decreases with advancing gestational age, from about 50% in babies born at 26–28 weeks, to about 25% at 30–31 weeks.
What is the cause of respiratory distress syndrome?
Infant respiratory distress syndrome (IRDS), also called neonatal respiratory distress syndrome, respiratory distress syndrome of newborn, or increasingly surfactant deficiency disorder (SDD), and previously called hyaline membrane disease (HMD), is a syndrome in premature infants caused by developmental insufficiency of surfactant production and structural immaturity in the lungs. It can also be a consequence of neonatal infection. It can also result from a genetic problem with the production of surfactant associated proteins. IRDS affects about 1% of newborn infants and is the leading cause of death in preterm infants. The incidence decreases with advancing gestational age, from about 50% in babies born at 26–28 weeks, to about 25% at 30–31 weeks. The syndrome is more frequent in infants of diabetic mothers and in the second born of premature twins.
What is the ICD code for acute care?
P22 . Non-Billable means the code is not sufficient justification for admission to an acute care hospital when used a principal diagnosis. Use a child code to capture more detail. ICD Code P22 is a non-billable code.
Popular Posts:
- 1. icd 10 code for left shoulder osteoarthritis.
- 2. icd 10 code for contusion left thigh
- 3. icd 9 code for bipolar disorder with depression
- 4. icd 10 code for dislocated jaw
- 5. icd-10-cm code for f07.82
- 6. icd 10 code for mass of the parotid gland
- 7. icd 10 code for intermittent arrhythmia
- 8. icd 10 code for pneumonia in right lung
- 9. icd 9 code for muscle sprain abdominal oblique
- 10. icd 10 code for sprain cancer