What is the ICD 10 code for encounter for lipoid disorders?
encounter for screening for respiratory tuberculosis ( Z11.1) ICD-10-CM Diagnosis Code E78.9 [convert to ICD-9-CM] Disorder of lipoprotein metabolism, unspecified. Abnormal lipid deposits; Cholesterol, abnormal; Disorder of lipid metabolism; Lipid …
What is the ICD-10 code for screening for hypercholesterolemia?
Z13.220 Z13.228 ICD-10-CM Code for Encounter for screening for lipoid disorders Z13.220 ICD-10 code Z13.220 for Encounter for screening for lipoid disorders is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services . Subscribe to Codify and get the code details in a flash.
What is the ICD 10 code for screening for asymptomatic?
2022 ICD-10-CM Code Z13.220 Encounter for screening for lipoid disorders. ICD-10-CM Index; Chapter: Z00–Z99; Section: Z00-Z13; Block: Z13; Z13.220 - …
What is the ICD 10 code for present on admission?
· Z13.220 is a valid billable ICD-10 diagnosis code for Encounter for screening for lipoid disorders . It is found in the 2022 version of the ICD-10 Clinical Modification (CM) and can be used in all HIPAA-covered transactions from Oct 01, 2021 - Sep 30, 2022 . POA Exempt Z13.220 is exempt from POA reporting ( Present On Admission).
What is Encounter for screening for lipoid disorders?
220, "Encounter for screening for lipoid disorders." For a patient already diagnosed with hyperlipidemia who is undergoing a lab test and being monitored or treated, you would use a code from category E78, "Disorders of lipoprotein metabolism and other lipidemias."
What is the ICD-10 code for screening?
9.
What is diagnosis code E78?
E78: Disorders of lipoprotein metabolism and other lipidaemias.
What is z13220?
Z13. 220 - Encounter for screening for lipoid disorders | ICD-10-CM.
What does code Z12 11 mean?
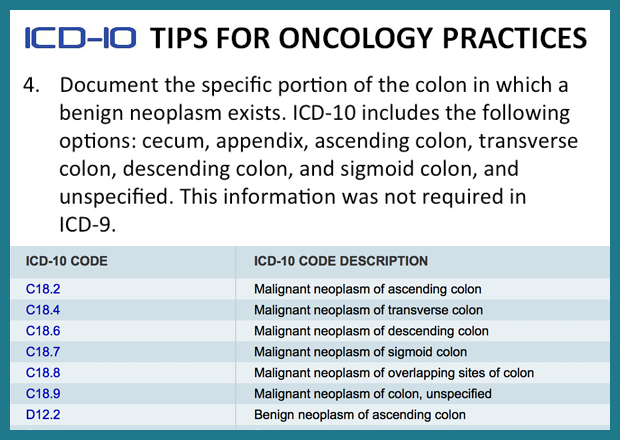
A screening colonoscopy should be reported with the following International Classification of Diseases, 10th edition (ICD-10) codes: Z12. 11: Encounter for screening for malignant neoplasm of the colon.
What is the ICD-10 code for preventive care?
The adult annual exam codes are as follows: Z00. 00, Encounter for general adult medical examination without abnormal findings, Z00.
What is ICD-10 code I10?
Essential (primary) hypertension: I10 That code is I10, Essential (primary) hypertension. As in ICD-9, this code includes “high blood pressure” but does not include elevated blood pressure without a diagnosis of hypertension (that would be ICD-10 code R03. 0).
What does E78 2 mean?
2022 ICD-10-CM Diagnosis Code E78. 2: Mixed hyperlipidemia.
What is Dyslipoproteinemia?
Dyslipoproteinemia, also referred to as dyslipidemia, encompasses a range of disorders of lipoprotein lipid metabolism that include both abnormally high and low lipoprotein concentrations, as well as abnormalities in the composition of these lipoprotein particles.
When do you use Z11 59?
52 will replace Z11. 59 (Encounter for screening for other viral diseases), which the CDC previously said should be used when patients being screened for COVID-19 have no symptoms, no known exposure to the virus, and test results that are either unknown or negative.
What is R53 83?
ICD-10 | Other fatigue (R53. 83)
What is HLD hyperlipidemia?
Hyperlipidemia (high cholesterol) means your blood has too many lipids (fats) in it. These can add up and lead to blockages in your blood vessels. This is why high cholesterol can put you at risk for a stroke or heart attack.
When was the ICd 10 code implemented?
FY 2016 - New Code, effective from 10/1/2015 through 9/30/2016 (First year ICD-10-CM implemented into the HIPAA code set)
What is the Z13.220 code?
Z13.220 is a billable diagnosis code used to specify a medical diagnosis of encounter for screening for lipoid disorders. The code Z13.220 is valid during the fiscal year 2021 from October 01, 2020 through September 30, 2021 for the submission of HIPAA-covered transactions. The code is exempt from present on admission (POA) reporting for inpatient admissions to general acute care hospitals.#N#The code Z13.220 describes a circumstance which influences the patient's health status but not a current illness or injury. The code is unacceptable as a principal diagnosis.
Why do you need to report POA indicators to CMS?
POA indicators must be reported to CMS on each claim to facilitate the grouping of diagnoses codes into the proper Diagnostic Related Groups (DRG). CMS publishes a listing of specific diagnosis codes that are exempt from the POA reporting requirement.
What is a screening test?
Also called: Screening tests. Screenings are tests that look for diseases before you have symptoms. Screening tests can find diseases early, when they're easier to treat. You can get some screenings in your doctor's office. Others need special equipment, so you may need to go to a different office or clinic.
What is the ICd 10 code for lipoid disorders?
Z13.220 is a valid billable ICD-10 diagnosis code for Encounter for screening for lipoid disorders . It is found in the 2021 version of the ICD-10 Clinical Modification (CM) and can be used in all HIPAA-covered transactions from Oct 01, 2020 - Sep 30, 2021 .
Is Z13.220 a POA?
Z13.220 is exempt from POA reporting ( Present On Admission).
What is the ICd10 code for lipoid disorders?
The ICD10 code for the diagnosis "Encounter for screening for lipoid disorders" is "Z13.220". Z13.220 is a VALID/BILLABLE ICD10 code, i.e it is valid for submission for HIPAA-covered transactions.
When did the ICD-10-CM Z13.220 become effective?
The 2019 edition of ICD-10-CM Z13.220 became effective on October 1, 2018.
When should a child be screened for lipids?
In a statement on screening for lipid disorders in children, the USPSTF (2007) concluded that the evidence is insufficient to recommend for or against routine screening for lipid disorders in infants, children, adolescents, or young adults (up to age 20).
What is the USPSTF recommendation for cholesterol screening?
The USPSTF recommends screening with total cholesterol, HDL-C, and lipoprotein analysis for persons with major coronary heart disease risk factors (e.g., smoking, hypertension, and diabetes). These guidelines recommend, for high-risk persons, lipoprotein analysis to help identify individuals at highest risk of coronary heart disease (CHD) in whom individual diet or drug therapy may be indicated. The optimal frequency of screening has not been determined and is left to clinical discretion.
How old do you have to be to get a cholesterol test?
The AAP does not recommend screening before 2 years of age. The NCEP recommends screening once with total blood cholesterol for children and adolescents 2 years of age or older whose parents have a blood cholesterol level greater than 240 mg/dL.
What age should a child be to get a cholesterol test?
Although routine cholesterol screening is recommended only for high-risk children, pediatricians should suggest that all children 2 years of age and older follow the American Heart Association's Step One Diet, which is essentially a low-cholesterol diet. The NCEP recommends measurement of triglyceride levels.
Is cholesterol screening mandatory?
The American College of Physicians (ACP) - American Society of Internal Medicine, in guidelines revised in 1996, concluded that screening serum cholesterol was appropriate but not mandatory for asymptomatic men aged 35 to 65 and women aged 45 to 65; the guidelines do not recommend screening for younger persons unless they have evidence of having a familial lipoprotein disorder or have multiple cardiac risk factors. The ACP concluded that evidence was not sufficient to recommend for or against screening asymptomatic persons between the ages of 65 and 75, but the ACP recommends against screening after age 75.
Is adolescent blood cholesterol screened?
The NCEP recommends periodic total blood cholesterol screening children and adolescent with several risk factors whose family history can not be ascertained; the optimal screening frequency for high blood cholesterol in this risk group has not been determined and is left to clinical discretion.
Popular Posts:
- 1. icd-9 code for wilms tumor
- 2. icd 10 diagnosis code for pain as sequela from multiple broken ribs
- 3. icd 10 code for soft tissue abscess
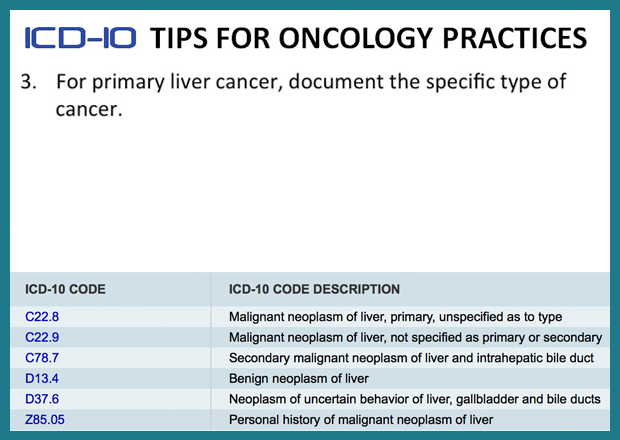
- 4. icd 10 code for lung cancer with mets to liver
- 5. icd 10 cm code for epidermoid cyst)
- 6. icd 10 code for right thumb pain 2017
- 7. icd 10 code for abnl gi
- 8. icd 10 code for disorder of bone unspecified
- 9. icd-10-pcs code for heart transplantation, allogeneic
- 10. icd 10 code for seizures with status epilepticus