Is sepsis always coded first?
ICD-10-CM Official Guidelines for Coding and Reporting directs us that when sepsis or severe sepsis is documented as being associated with a noninfectious condition, such as a burn or serious injury, and this condition meets the definition for principal diagnosis, the code for the noninfectious condition should be ...5 Dec 2016
Can sepsis be coded as primary diagnosis?
If severe sepsis is present on admission, and it meets the definition of principal diagnosis, the underlying systemic infection should be assigned as principal diagnosis; the underlying systemic condition should be documented and coded as principal diagnosis followed by the appropriate code from subcategory R65.
How do you code Post procedural sepsis?
The 2019 Guidelines also added the following language for sepsis due to a postprocedural infection: For infections following infusion, transfusion, therapeutic injection, or immunization, a code from subcategory T80. 2-, or code T88. 0-, should be coded first, followed by the code for the specific infection.16 Aug 2018
What is the proper order that severe sepsis should be coded?
The coding of severe sepsis requires a minimum of two codes: first a code for the underlying systemic infection, followed by a code from subcategory R65. 2, Severe sepsis. If the causal organism is not documented, assign code A41.19 Jul 2017
What is the ICD 10 code for sepsis?
A41.9Septicemia – There is NO code for septicemia in ICD-10. Instead, you're directed to a combination 'A' code for sepsis to indicate the underlying infection, such A41. 9 (Sepsis, unspecified organism) for septicemia with no further detail.
What is the ICD 10 code for severe sepsis?
Severe sepsis with septic shock R65. 21 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
How do you code an abscess in ICD-10?
ICD-10 code L02 for Cutaneous abscess, furuncle and carbuncle is a medical classification as listed by WHO under the range - Diseases of the skin and subcutaneous tissue .
When is sepsis not the principal diagnosis?
Other instances when sepsis would not be selected as the principal diagnosis, even if it was POA include the scenario where sepsis is the result of a condition which is classified as a “medical complication” (such as being due to an indwelling urinary catheter or central line.16 Aug 2018
When coding sepsis and severe sepsis which code should be sequenced first?
Coding tips: According to the guidelines, for all cases of documented septic shock, the code for the underlying systemic infection (i.e., sepsis) should be sequenced first, followed by code R65. 21 or T81.1 Jun 2021
What is the principal diagnosis when the term sepsis is documented with an underlying infection?
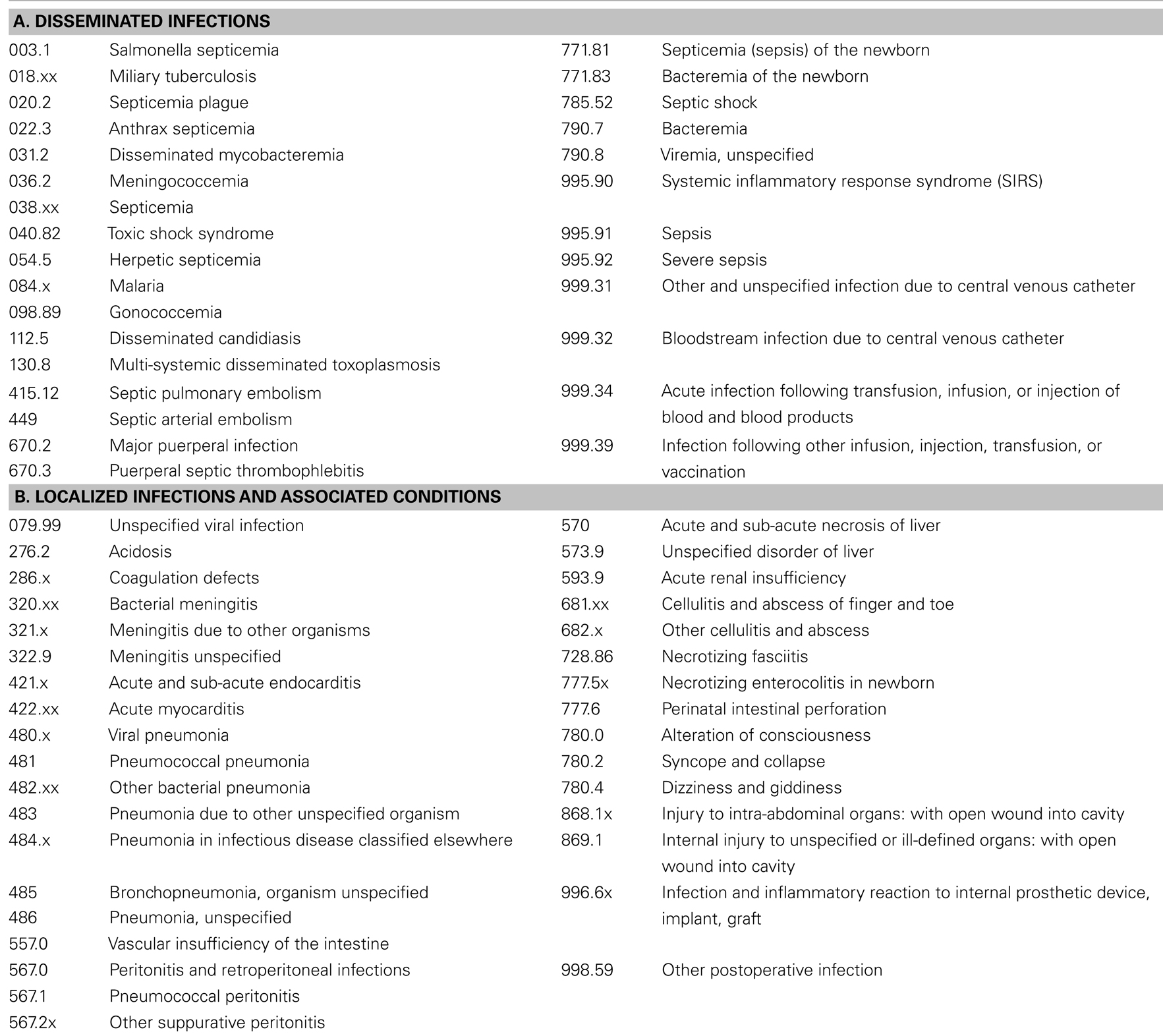
The sequencing of sepsis as a principal diagnosis relies heavily on provider documentation. If sepsis is present on admission and meets the definition of principal diagnosis, the systemic infection code (038. xx, 112.5, etc.)
What is the life threatening condition that occurs when the body’s response to an infection damages its own tissues?
Sepsis is a potentially life-threatening condition that occurs when the body’s response to an infection damages its own tissues. Without timely treatment, sepsis can progress rapidly and lead to tissue damage, organ failure, and then death. Proper coding of sepsis and SIRS requires the coder to understand the stages of sepsis and common documentation issues.
Is septicemia difficult to code?
Sepsis, systemic inflammatory response syndrome (SIRS), and septicemia have historically been difficult to code. Changing terminology, evolving definitions, and guideline updates over the past 20 years have created confusion with coding sepsis.
What is SIRS in the body?
SIRS is an inflammatory state affecting the whole body. It is an exaggerated defense response of the body to a noxious stressor, such as infection or trauma, that triggers an acute inflammatory reaction, which may progress and result in the formation of blood clots, impaired fibrinolysis, and organ failure.
What is the response to sepsis?
Sepsis is an extreme response to infection that develops when the chemicals the immune system releases into the bloodstream to fight infection cause widespread inflammation. This inflammation can lead to blood clots and leaky blood vessels, and without timely treatment, may result in organ dysfunction and then death. Severe cases of sepsis often result from a body-wide infection that spreads through the bloodstream, but sepsis can also be triggered by an infection in the lungs, stomach, kidneys, or bladder. Thus, it is not necessary for blood cultures to be positive to code sepsis (guideline I.C.1.d.1.a.i).
What is septic shock?
Septic shock refers to circulatory failure associated with severe sepsis. It is a life-threatening condition that happens when the exaggerated response to infection leads to dangerously low blood pressure (hypotension). Septic shock is a form of organ failure.
What is systemic infection?
A systemic infection can occur as a complication of a procedure or due to a device, implant, or graft. This includes systemic infections due to postoperative wound infections, infusions, transfusions, therapeutic injections, implanted devices, and transplants.
What are the symptoms of a localized infection?
Documentation issues: A patient with a localized infection usually presents with tachycardia, leukocytosis, tachypnea, and/or fever. These are typical symptoms of any infection. It is up to the clinical judgment of the physician to decide whether the patient has sepsis.
What causes sepsis in a graft?
Patients with devices, implants or grafts often develop sepsis due to the presence of the device. The link MUST be made by the physician. If this link is not made, or there is conflicting documentation, a query is necessary to clarify the cause and effect relationship. When looking in the ICD-10-CM alphabetic index, there are entries under Sepsis—due to for arterial graft to ventricular shunt. The most common graft/device/implant infections are found in hemodialysis, vascular, and urinary patients. This typically occurs due to skin organisms, but this is not always the cause. The coder must read the documentation carefully to help in determining the type of device, implant or graft that is infected.
When is the sepsis code sequenced?
When sepsis is present on admission and due to a localized infection (not a device or post procedural), the sepsis code is sequenced first followed by the code for the localized infection.
What is the most common graft infection?
The most common graft/device/implant infections are found in hemodialysis, vascular, and urinary patients. This typically occurs due to skin organisms, but this is not always the cause. The coder must read the documentation carefully to help in determining the type of device, implant or graft that is infected.
Popular Posts:
- 1. icd 10 code for abdomne free fluid
- 2. icd 10 code for mocus in stool
- 3. icd-10 code for liver function test
- 4. icd 9 code for upper respiratory infection with bilateral acute conjunctivitis
- 5. icd 10 code for increased behaviors
- 6. icd 10 code for riht hand pain
- 7. icd 10 code for billirubina
- 8. 2017 icd 10 code for atrophy of the supraspinatus muscle belly.
- 9. icd 10 cm code for endometriosis of fallopian tube
- 10. billable icd 10 code for cellulitis of hand