How do you code recurrent UTI?
Oct 01, 2021 · Sepsis due to Pseudomonas 2016 2017 2018 2019 2020 2021 2022 Billable/Specific Code A41.52 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM A41.52 became effective on October 1, 2021.
What is the diagnosis code for UTI?
Infection and inflammatory reaction due to pulse generator or receiver of sacral nerve neurostimulator ( T85.734) ICD-10-CM Diagnosis Code A41.52 [convert to ICD-9-CM] Sepsis due to Pseudomonas. Pseudomonas septicemia; Sepsis without acute organ dysfunction due to pseudomonas septicemia; Septic shock acute organ dysfunction, pseudomonas; Septic shock …
What is the code for bacteremia due to Pseudomonas?
Mar 05, 2020 · What is the ICD 10 code for sepsis due to UTI? A41. 51 is a billable/specific ICD - 10 -CM code that can be used to indicate a diagnosis for …
What antibiotics treat Pseudomonas UTI?
The ICD-10-CM code A41.52 might also be used to specify conditions or terms like sepsis caused by pseudomonas aeruginosa, sepsis due to pseudomonas or septic shock co-occurrent with acute organ dysfunction due to pseudomonas. Tabular List of Diseases and Injuries
What is the ICD 10 code for Pseudomonas UTI?
ICD-10-CM Code for Pseudomonas (aeruginosa) (mallei) (pseudomallei) as the cause of diseases classified elsewhere B96. 5.
What is the ICD 10 code for sepsis due to UTI?
The coding of severe sepsis with ICD-10 should include the source of infection, a UTI in this case, plus the code for severe sepsis....The ED coder would assign the following ICD-10 diagnosis codes:R65.21Severe sepsis with shockN39.0UTI, site not specifiedR30.0Dysuria4 more rows
What is the ICD 10 code for pseudomonas infection?
ICD-10 code: B96. 5 Pseudomonas (aeruginosa) as the cause of diseases classified to other chapters - gesund.bund.de.
How do you code Urosepsis in icd10?
Urosepsis is actually coded urinary tract infection (599.0) in ICD 9. But, in ICD 10 is has no diagnosis code for urosepsis. ICD 10 does not consider urosepsis as disease or disorder. Hence urosepsis should not be coded in ICD 10, only sepsis should be reported with ICD 10 diagnosis codes.Aug 2, 2019
What is the diagnosis code for sepsis?
A41.9A41. 9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
Can sepsis be primary diagnosis?
According to the guidelines above, sepsis would be the appropriate principal diagnosis if it is the reason the patient is admitted, and meets the definition of principal diagnosis.Dec 5, 2016
What is the ICD-10 code for E coli UTI?
2 for Escherichia coli [E.
What is the ICD-10 code for urinary retention?
ICD-10 | Retention of urine, unspecified (R33. 9)
What is aeruginosa infection?
aeruginosa infections include bloodstream infections, pneumonia, urinary tract infections, and surgical wound infections. These infections typically affect people who are ill in the hospital, particularly those with weakened immune systems from diseases or long-term treatments.Dec 1, 2020
What is the ICD 10 code for severe sepsis?
The coding of severe sepsis requires a minimum of two codes: first a code for the underlying systemic infection, followed by a code from subcategory R65. 2, Severe sepsis. If the causal organism is not documented, assign code A41. 9, Sepsis, unspecified organism, for the infection.Jul 19, 2017
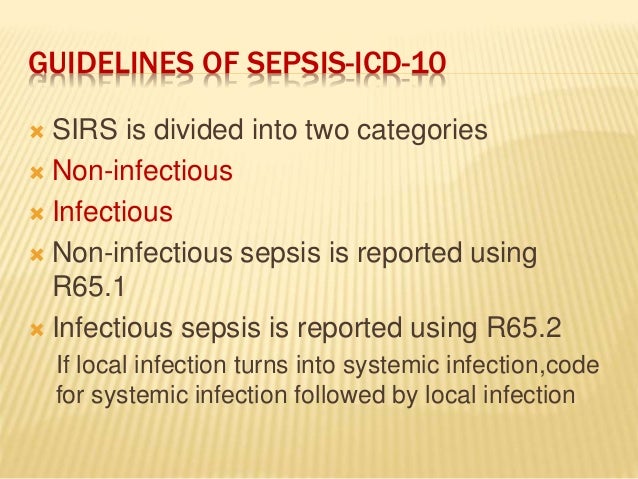
Can you code SIRS and sepsis together?
3, p. 4), when a patient has SIRS and a localized infection, sepsis can no longer be coded and an ICD-10-CM code for sepsis cannot be assigned unless the physician specifically documents sepsis.Jun 1, 2021
When is sepsis not the principal diagnosis?
Other instances when sepsis would not be selected as the principal diagnosis, even if it was POA include the scenario where sepsis is the result of a condition which is classified as a “medical complication” (such as being due to an indwelling urinary catheter or central line.Aug 16, 2018
What is the ICd 10 code for sepsis?
A41.52 is a billable diagnosis code used to specify a medical diagnosis of sepsis due to pseudomonas. The code A41.52 is valid during the fiscal year 2021 from October 01, 2020 through September 30, 2021 for the submission of HIPAA-covered transactions.#N#The ICD-10-CM code A41.52 might also be used to specify conditions or terms like pseudomonas septicemia with skin involvement, sepsis caused by pseudomonas aeruginosa, sepsis due to pseudomonas, septic shock co-occurrent with acute organ dysfunction due to pseudomonas or severe sepsis with acute organ dysfunction due to pseudomonas.
What are the different types of septic shock?
The following clinical terms are approximate synonyms or lay terms that might be used to identify the correct diagnosis code: 1 Pseudomonas septicemia with skin involvement 2 Sepsis caused by Pseudomonas aeruginosa 3 Sepsis due to Pseudomonas 4 Septic shock co-occurrent with acute organ dysfunction due to Pseudomonas 5 Severe sepsis with acute organ dysfunction due to Pseudomonas
What is post-procedural sepsis?
Post-procedural Sepsis and Sepsis Due to a Device, Implant, or Graft. A systemic infection can occur as a complication of a procedure or due to a device, implant, or graft. This includes systemic infections due to wound infection, infusions, transfusions, therapeutic injections, implanted devices, and transplants.
Why is severe sepsis not assigned?
For instance, if severe sepsis, pneumonia, and acute renal failure due to dehydration are documented, the code for severe sepsis may not be assigned because the acute renal failure is not stated as due to or associated with sepsis. If the documentation is unclear, query the physician.
What is the term for a lab finding of infectious organisms in the blood?
Bacteremia . Bacteremia is a lab finding of infectious organisms in the blood. The patient has no clinical signs of sepsis or SIRS. Bacteremia may be transient, or may lead to sepsis. When a patient’s blood cultures are positive and not believed to be a contaminant, the patient is usually treated with antibiotics.
When to query a physician for sepsis?
You must query the physician when the term “sepsis syndrome” is documented as a final diagnosis. Know when to Query. Sepsis is a complicated condition to code, and it is often necessary to query the physician to code the case correctly.
Can you code for sepsis?
Documentation issues: You can code for sepsis when the physician documents the term “sepsis.”. Documentation should be consistent throughout the chart. Occasionally, during an extended length of stay, sepsis may resolve quickly and the discharging doctor may not include the diagnosis of sepsis on the discharge summary.
Is sepsis a systemic infection?
term “sepsis” must also be documented to code a systemic infection. This is a major change from ICD-9-CM. If the term “sepsis” is not documented with “SIRS” when it’s due to a localized infection, you must ask for clarification from the physician.
Is septic shock documented without sepsis?
Documentation issues: The term “septic shock” is occasionally documented without the term “sepsis.”. According to the guidelines, for all cases of septic shock the code for the underlying systemic infection is sequenced first, followed by R65.21 Severe sepsis with septic shock or T81.12- Postprocedural septic shock.
What are the infections that affect the secretion and elimination of urine?
Infections affecting stuctures participating in the secretion and elimination of urine: the kidneys, ureters, urinary bladder and urethra. Inflammatory responses of the epithelium of the urinary tract to microbial invasions. They are often bacterial infections with associated bacteriuria and pyuria.
What is a UTI after a procedure?
Uti (urinary tract infection) after procedure. Clinical Information. A bacterial infectious process affecting any part of the urinary tract, most commonly the bladder and the urethra. Symptoms include urinary urgency and frequency, burning sensation during urination, lower abdominal discomfort, and cloudy urine.
How to tell if you have a UTI?
if you think you have a uti, it is important to see your doctor. Your doctor can tell if you have a uti by testing a sample of your urine. Treatment with medicines to kill the infection will make it better, often in one or two days.
What is the second most common type of infection in the body?
The urinary system consists of the kidneys, ureters, bladder and urethra. Infections of the urinary tract (utis) are the second most common type of infection in the body. You may have a uti if you notice.
Why is severe sepsis not assigned?
For instance, if sepsis, pneumonia, and acute renal failure due to dehydration are documented, the code for severe sepsis may not be assigned because the acute renal failure is not stated as due to or associated with sepsis. If the documentation is unclear, query the physician.
What is the most common type of infection that leads to sepsis?
Localized Infection. Almost any type of infection can lead to sepsis. Infections that lead to sepsis most often start in the lung, urinary tract, skin, or gastrointestinal tract. When localized infections are contained, they tend to be self-limiting and resolve with antibiotics.
How does sepsis affect the body?
Sepsis is an extreme response to infection that develops when the chemicals the immune system releases into the bloodstream to fight infection cause widespread inflammation. This inflammation can lead to blood clots and leaky blood vessels, and without timely treatment, may result in organ dysfunction and then death. Severe cases of sepsis often result from a body-wide infection that spreads through the bloodstream, but sepsis can also be triggered by an infection in the lungs, stomach, kidneys, or bladder. Thus, it is not necessary for blood cultures to be positive to code sepsis (guideline I.C.1.d.1.a.i).
How to improve sepsis documentation?
To improve sepsis documentation, coding staff needs to work closely with clinical documentation improvement specialists (CDIs), and everyone must be clear on what documentation is needed to correctly code sepsis. A physician champion can be helpful to establish guidelines for the physicians and standard terminology to use when documenting sepsis. A coding tip sheet that includes various scenarios is a helpful tool for the coding department to standardize definitions and the interpretation of the coding guidelines. A regular audit of sepsis DRGs or sepsis as a secondary code can help to identify documentation issues and coders who need more education. Sepsis is never going to be easy to code, but with continuous education and teamwork across departments, the sepsis beast can be conquered.
What is septic shock?
Septic shock refers to circulatory failure associated with severe sepsis. It is a life-threatening condition that happens when the exaggerated response to infection leads to dangerously low blood pressure (hypotension). Septic shock is a form of organ failure.
When is a localized infection coded?
If the patient is admitted with a localized infection and the patient does not develop sepsis or severe sepsis until after the admission, the localized infection is coded first, followed by the appropriate codes for sepsis or severe sepsis, if applicable .
What are the symptoms of a localized infection?
Documentation issues: A patient with a localized infection usually presents with tachycardia, leukocytosis, tachypnea, and/or fever. These are typical symptoms of any infection. It is up to the clinical judgment of the physician to decide whether the patient has sepsis.
Popular Posts:
- 1. icd 10 code for exertional sob
- 2. icd 10 code for bmi 95
- 3. icd 10 cm code for klebsiella pneumo
- 4. icd 10 code for coccyx pain
- 5. icd 10 code for rosacea dermatitis with conjunctivitis left eye
- 6. icd 10 code for postoperative pneumoperitoneum
- 7. icd-10 code for post tussive emesis
- 8. icd 10 code for copd with bronchitis
- 9. icd 10 code for large hiatal hernia
- 10. icd 10 code for lymphangiectasia of duodenum