How to Code Sepsis ICD 10?
Oct 01, 2021 · R65.21 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM R65.21 became effective on October 1, 2021. This is the American ICD-10-CM version of R65.21 - other international versions of ICD-10 R65.21 may differ.
What is ICD 10 code for sepsis?
code to type of kidney disease. ICD-10-CM Diagnosis Code R65.21 [convert to ICD-9-CM] Severe sepsis with septic shock. septicemia; Septic shock with acute organ dysfunction due to methicillin resistant staphylococcus aureus septicemia; Septic shock with acute organ dysfunction due to pneumococcal septicemia; Septic shock with acute organ dysfunction due …
How to code severe sepsis?
Oct 01, 2021 · Severe sepsis. 2016 2017 2018 2019 2020 2021 2022 Non-Billable/Non-Specific Code. R65.2 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail. The 2022 edition of ICD-10-CM R65.2 became effective on October 1, 2021.
Is sepsis always the principal diagnosis?
Oct 01, 2021 · A41.3 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM A41.3 became effective on October 1, 2021. This is the American ICD-10-CM version of A41.3 - other international versions of ICD-10 A41.3 may differ.

What is the ICD-10 code for severe sepsis with acute organ dysfunction?
Note: 'A' codes for Sepsis in ICD-10 include both the underlying infection (septicemia) and the body's inflammatory reaction. if organ dysfunction is present. If it is, you'll need to include a code from R65. 2-, Severe Sepsis.
Can sepsis be coded as primary diagnosis?
According to the guidelines above, sepsis would be the appropriate principal diagnosis if it is the reason the patient is admitted, and meets the definition of principal diagnosis.Dec 5, 2016
How do I code sepsis?
Coding sepsis requires a minimum of two codes: a code for the systemic infection (e.g., 038. xx) and the code 995.91, SIRS due to infectious process without organ dysfunction. If no causal organism is documented within the medical record, query the physician or assign code 038.9, Unspecified septicemia.
What are the codes to be reported when patient has sepsis and organ failure?
The coding of severe sepsis requires a minimum of two codes: first a code for the underlying systemic infection, followed by a code from subcategory R65. 2, Severe sepsis. If the causal organism is not documented, assign code A41. 9, Sepsis, unspecified organism, for the infection.Jul 19, 2017
What is the ICD 10 code for sepsis due to UTI?
The coding of severe sepsis with ICD-10 should include the source of infection, a UTI in this case, plus the code for severe sepsis....The ED coder would assign the following ICD-10 diagnosis codes:R65.21Severe sepsis with shockN39.0UTI, site not specifiedR30.0Dysuria4 more rows
Is severe sepsis a diagnosis?
Sepsis is the body's overwhelming and life-threatening response to infection that can lead to tissue damage, organ failure, and death. In other words, it's your body's overactive and toxic response to an infection. Like strokes or heart attacks, sepsis is a medical emergency that requires rapid diagnosis and treatment.
When is sepsis not the principal diagnosis?
Other instances when sepsis would not be selected as the principal diagnosis, even if it was POA include the scenario where sepsis is the result of a condition which is classified as a “medical complication” (such as being due to an indwelling urinary catheter or central line.Aug 16, 2018
When coding sepsis and severe sepsis which code should be sequenced first?
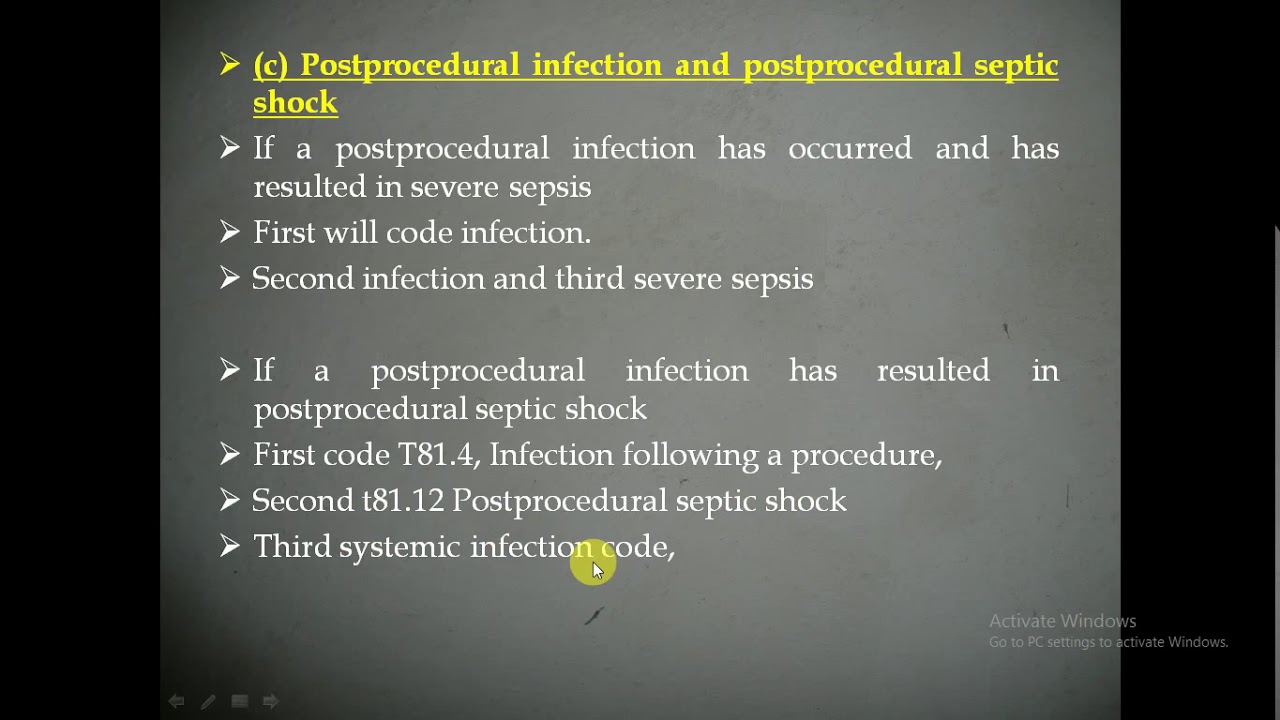
Coding tips: According to the guidelines, for all cases of documented septic shock, the code for the underlying systemic infection (i.e., sepsis) should be sequenced first, followed by code R65. 21 or T81.Jun 1, 2021
When do you code severe sepsis?
20, Severe sepsis. If the causal organism is not documented, assign code A41. 9, Sepsis, unspecified organism, for the infection. Additional code(s) for the associated acute organ dysfunction are also required.”
When do you code sepsis first?
When sepsis is present on admission and due to a localized infection (not a device or post procedural), the sepsis code is sequenced first followed by the code for the localized infection.Nov 8, 2019
Can you code SIRS and sepsis together?
11 Systemic inflammatory response syndrome (SIRS) of non-infectious origin with acute organ dysfunction). The guidelines in chapter 1 no longer make reference to SIRS with sepsis and severe sepsis.Aug 1, 2015
Why is severe sepsis not assigned?
For instance, if sepsis, pneumonia, and acute renal failure due to dehydration are documented, the code for severe sepsis may not be assigned because the acute renal failure is not stated as due to or associated with sepsis. If the documentation is unclear, query the physician.
What is the most common type of infection that leads to sepsis?
Localized Infection. Almost any type of infection can lead to sepsis. Infections that lead to sepsis most often start in the lung, urinary tract, skin, or gastrointestinal tract. When localized infections are contained, they tend to be self-limiting and resolve with antibiotics.
How does sepsis affect the body?
Sepsis is an extreme response to infection that develops when the chemicals the immune system releases into the bloodstream to fight infection cause widespread inflammation. This inflammation can lead to blood clots and leaky blood vessels, and without timely treatment, may result in organ dysfunction and then death. Severe cases of sepsis often result from a body-wide infection that spreads through the bloodstream, but sepsis can also be triggered by an infection in the lungs, stomach, kidneys, or bladder. Thus, it is not necessary for blood cultures to be positive to code sepsis (guideline I.C.1.d.1.a.i).
How to improve sepsis documentation?
To improve sepsis documentation, coding staff needs to work closely with clinical documentation improvement specialists (CDIs), and everyone must be clear on what documentation is needed to correctly code sepsis. A physician champion can be helpful to establish guidelines for the physicians and standard terminology to use when documenting sepsis. A coding tip sheet that includes various scenarios is a helpful tool for the coding department to standardize definitions and the interpretation of the coding guidelines. A regular audit of sepsis DRGs or sepsis as a secondary code can help to identify documentation issues and coders who need more education. Sepsis is never going to be easy to code, but with continuous education and teamwork across departments, the sepsis beast can be conquered.
What is septic shock?
Septic shock refers to circulatory failure associated with severe sepsis. It is a life-threatening condition that happens when the exaggerated response to infection leads to dangerously low blood pressure (hypotension). Septic shock is a form of organ failure.
When is a localized infection coded?
If the patient is admitted with a localized infection and the patient does not develop sepsis or severe sepsis until after the admission, the localized infection is coded first, followed by the appropriate codes for sepsis or severe sepsis, if applicable .
What is systemic infection?
A systemic infection can occur as a complication of a procedure or due to a device, implant, or graft. This includes systemic infections due to postoperative wound infections, infusions, transfusions, therapeutic injections, implanted devices, and transplants.
Popular Posts:
- 1. icd 10 code for postural hypotension
- 2. what is the icd 10 code for trig
- 3. icd 10 code for fractureof iliac crest
- 4. icd 10 code for chronic gingivitis, plaque induced
- 5. icd 10 code for sarcoid lung
- 6. icd 10 code for carbuncle
- 7. 2015 icd 10 code for restrained driver motor vehicle accident
- 8. icd 10 cm code for bitten by ants
- 9. 2021 icd 10 code for nasal congestion
- 10. icd 10 code for fish test