What is the ICD 10 code for sepsis?
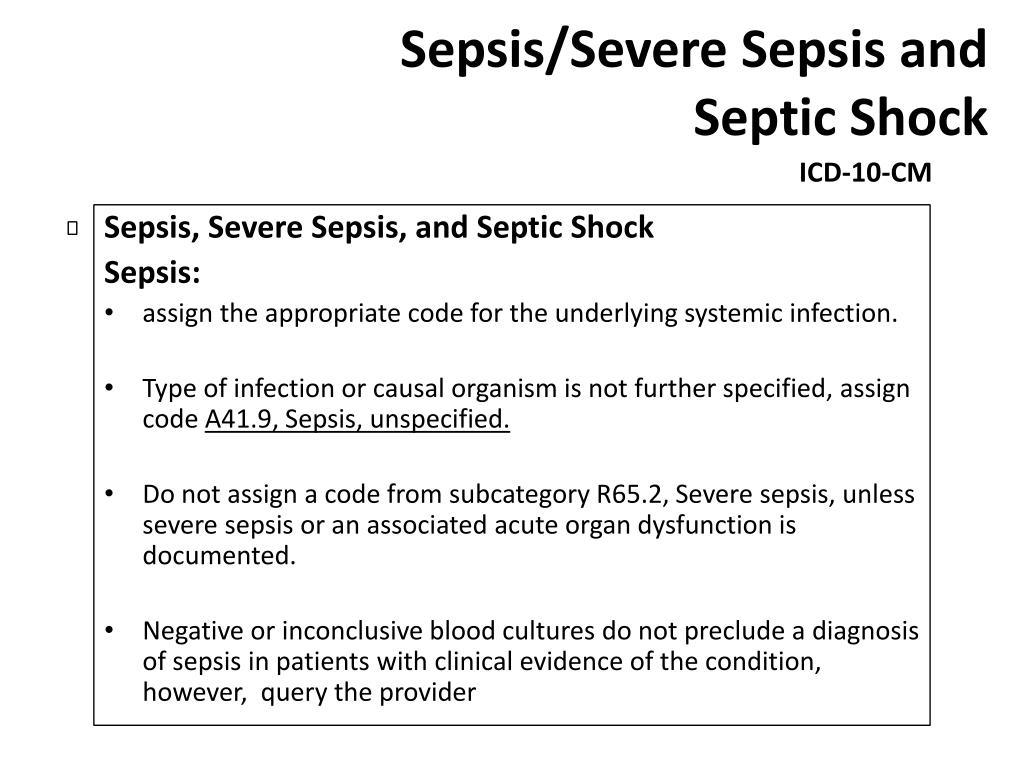
Sepsis, unspecified organism 1 A41.9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. 2 The 2020 edition of ICD-10-CM A41.9 became effective on October 1, 2019. 3 This is the American ICD-10-CM version of A41.9 - other international versions of ICD-10 A41.9 may differ.
What is the ICD 10 code for delirium tremens?
When a type 2 excludes note appears under a code it is acceptable to use both the code (F05) and the excluded code together. delirium tremens alcohol-induced or unspecified ( ICD-10-CM Diagnosis Code F10.231. Alcohol dependence with withdrawal delirium 2016 2017 2018 2019 Billable/Specific Code.
How do you code severe sepsis with pneumonia and dehydration?
For instance, if severe sepsis, pneumonia, and acute renal failure due to dehydration are documented, the code for severe sepsis may not be assigned because the acute renal failure is not stated as due to or associated with sepsis. If the documentation is unclear, query the physician. “Multi-organ dysfunction” is not coded.
What is the ICD 10 code for sepsis with cellulitis?
ICD-10-CM, as it does in ICD-9-CM. Septic shock is combined into code R65.21. Example: A patient is admitted with cellulitis and abscess of the left leg, severe sepsis, septic shock, and acute renal failure and encephalopathy due to the sepsis. A41.9
How do you code Delirium?
If the delirium is due to a physical or neurological condition, then assign a code for the specific condition documented followed by code 293.0 for acute delirium, 293.89 for chronic delirium, 293.1 for subacute delirium, or 293.9 for unspecified delirium.
What is the ICD-10 code for Delirium of unclear cause?
Delirium due to known physiological condition The 2022 edition of ICD-10-CM F05 became effective on October 1, 2021.
What is the 2021 ICD-10 code for sepsis?
ICD-10 code A41. 9 for Sepsis, unspecified organism is a medical classification as listed by WHO under the range - Certain infectious and parasitic diseases .
What is the ICD-10 code for Severe sepsis?
ICD-10 code R65. 21 for Severe sepsis with septic shock is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
What is the ICD-10 code for acute delirium?
ICD-10 code F05 for Delirium due to known physiological condition is a medical classification as listed by WHO under the range - Mental, Behavioral and Neurodevelopmental disorders .
What is the condition delirium?
Delirium is a state of mental confusion that can happen if you become medically unwell. It is also known as an 'acute confusional state'. Medical problems, surgery and medications can all cause delirium. It often starts suddenly, but usually lifts when the condition causing it gets better.
Can sepsis be coded as primary diagnosis?
According to the guidelines above, sepsis would be the appropriate principal diagnosis if it is the reason the patient is admitted, and meets the definition of principal diagnosis.
When do you code sepsis?
Coding sepsis requires a minimum of two codes: a code for the systemic infection (e.g., 038. xx) and the code 995.91, SIRS due to infectious process without organ dysfunction. If no causal organism is documented within the medical record, query the physician or assign code 038.9, Unspecified septicemia.
When coding sepsis and severe sepsis which code should be sequenced first?
Coding tips: According to the guidelines, for all cases of documented septic shock, the code for the underlying systemic infection (i.e., sepsis) should be sequenced first, followed by code R65. 21 or T81.
How do you code severe sepsis without septic shock?
Two codes, at a minimum, are needed to report severe sepsis without septic shock. Chapter-specific guidelines state, “First code for the underlying systemic infection, followed by a code R65. 20, Severe sepsis. If the causal organism is not documented, assign code A41.
What constitutes severe sepsis?
Severe sepsis occurs when one or more of your body's organs is damaged from this inflammatory response. Any organ can be affected, your heart, brain, kidneys, lungs, and/or liver. The symptoms you can experience are based on which organ or organs that are affected.
Do you code sepsis with septic shock?
For cases of septic shock, a minimum of two codes is needed to report severe sepsis with septic shock. Chapter-specific guidelines state, “First code for the underlying systemic infection, followed by R65. 21, septic shock. If the causal organism is not documented, assign code A41.
How do you code severe sepsis?
The coding of severe sepsis requires a minimum of two codes: first a code for the underlying systemic infection, followed by a code from subcategory R65. 2, Severe sepsis. If the causal organism is not documented, assign code A41. 9, Sepsis, unspecified organism, for the infection.
How do you code UTI with sepsis?
A41. 51 (Sepsis due to Escherichia coli), and N39. 0 (Urinary tract infection, site not specified) would be reported as additional diagnoses.
What is the meaning of the code for sepsis?
Sepsis means potentially fatal condition caused when the body responses to the presence of infection or organisms in the blood. Choose the appropriate “A” code from the alphabetical index to indicate sepsis with type of infection or causal organism, if the doctor documents “Sepsis with type of infection or causal organism”.
What is the code for severe sepsis with septic shock?
Severe sepsis with septic shock: Septic shock means severe sepsis associated with circulatory failure. Assign the code in the same above format (severe sepsis) as it represents the type of acute organ dysfunction. But here, we will report a code R65.21 (which indicates severe sepsis with septic shock) instead of R65.20 (severe sepsis).
What is the A41.9 code?
If the doctor documents “Sepsis” but the type of infection or causal organism is not specified, then will assign the A41.9 code, which indicates Sepsis, unspecified organism.
What is septic shock with acute organ dysfunction due to?
Septic shock with acute organ dysfunction due to group a streptococcus. Septic shock with acute organ dysfunction due to group b streptococcus. Septic shock with acute organ dysfunction due to meningococcal septicemia.
What is septic shock?
Septic shock with acute organ dysfunction. Septic shock with acute organ dysfunction due to anaerobic septicemia. Septic shock with acute organ dysfunction due to chromobacterium. Septic shock with acute organ dysfunction due to coagulate-negative staphylococcu.
What is post-procedural sepsis?
Post-procedural Sepsis and Sepsis Due to a Device, Implant, or Graft. A systemic infection can occur as a complication of a procedure or due to a device, implant, or graft. This includes systemic infections due to wound infection, infusions, transfusions, therapeutic injections, implanted devices, and transplants.
Why is severe sepsis not assigned?
For instance, if severe sepsis, pneumonia, and acute renal failure due to dehydration are documented, the code for severe sepsis may not be assigned because the acute renal failure is not stated as due to or associated with sepsis. If the documentation is unclear, query the physician.
What are the discharge diagnoses?
The discharge diagnoses were influenza with pneumonia bacterial superinfection, positive for pseudomonas, as well as acidosis, asthma exacerbation, hypoxemia, and chronic bronchitis. Sepsis and SIRS were not mentioned on the discharge summary, and are mentioned only sporadically throughout the progress notes.
When to add R65.2-?
If the patient has severe sepsis, add R65.2- with the codes for specific organ dysfunctions.
When to query a physician for sepsis?
You must query the physician when the term “sepsis syndrome” is documented as a final diagnosis. Know when to Query. Sepsis is a complicated condition to code, and it is often necessary to query the physician to code the case correctly.
Can you code for sepsis?
Documentation issues: You can code for sepsis when the physician documents the term “sepsis.”. Documentation should be consistent throughout the chart. Occasionally, during an extended length of stay, sepsis may resolve quickly and the discharging doctor may not include the diagnosis of sepsis on the discharge summary.
Is sepsis a systemic infection?
term “sepsis” must also be documented to code a systemic infection. This is a major change from ICD-9-CM. If the term “sepsis” is not documented with “SIRS” when it’s due to a localized infection, you must ask for clarification from the physician.

Popular Posts:
- 1. icd 10 code for cerebellar hemangioblastoma
- 2. icd 10 code for right medial malleolus fracture
- 3. icd 10 code for abnormal imaging
- 4. icd 10 code for volar ganglion cyst
- 5. icd 10 code for s/p surgery l hip
- 6. icd 10 cm code for left upper extremity wrist pain
- 7. icd 10 code for film copies
- 8. icd 10 code for r elbow dermatitis due to spider bite
- 9. icd 10 code for spinal muscular atrophy type 1
- 10. icd 10 code for right index finger mucous cyst