What is the ICD 10 code for sialoadenitis?
Sialoadenitis. K11.2 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail. The 2019 edition of ICD-10-CM K11.2 became effective on October 1, 2018. This is the American ICD-10-CM version of K11.2 - other international versions of ICD-10 K11.2 may differ.
What is the ICD 10 code for lumbago with sciatica right side?
ICD-10-CM Code for Lumbago with sciatica, right side M54.41 ICD-10 code M54.41 for Lumbago with sciatica, right side is a medical classification as listed by WHO under the range - Dorsopathies. Subscribe to Codify and get the code details in a flash. Request a Demo 14 Day Free Trial Buy Now
What is a sequela in ICD 10?
The ICD-10-CM guidelines define a sequela as “the residual effect (condition produced) after the acute phase of an illness or injury has terminated.” The general coding guidelines in ICD-10-CM for coding of sequelae are essentially the same as coding of late effects in ICD-9-CM and are as follows:
What is Sialoendoscopy for the diagnosis of obstructive sialadenitis?
Maresh et al (2011) stated that sialoendoscopy is a new technology being used at a limited number of institutions for the diagnosis and management of obstructive sialadenitis.

What is sialadenitis of submandibular gland?
Submandibular sialadenitis is inflammation of the submandibular gland, which is caused by salivary stasis that leads to retrograde seeding of bacteria from the oral cavity. Sialadenosis is a benign,non-inflammatory swelling of salivary glands usually associated with metabolic conditions.
Is Parotitis the same as sialadenitis?
Classically, HIV parotitis is either asymptomatic or a non-painful swelling, which is not characteristic of sialadenitis. Some common bacterial causes are S. aureus, S. pyogenes, viridans streptococci and H.
What is the meaning of sialadenitis?
A salivary gland infection is also called sialadenitis and is caused by bacteria or viruses. A salivary stone or other blockage of the salivary gland duct can contribute to an acute infection. Chronic inflammation of a salivary gland can cause it to stop functioning.
What is Sialoadenitis unspecified?
Sialadenitis refers to the inflammation of a salivary gland, which produces saliva to aid in digestion. The condition is most common among elderly adults and mostly affects the parotid and submandibular glands.
What is the ICD 10 code for parotitis?
K11. 20 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM K11.
What causes acute sialadenitis?
What Causes Sialadenitis? Sialadenitis can be caused by a viral infection (such as mumps), bacterial infection, or an autoimmune disease such as Sjogren's syndrome (see below). Bacterial infections can happen when the flow of saliva is blocked due to stones in the salivary duct or a narrowing of the duct.
What causes Sialadenosis?
Sialadenosis usually occurs in association with a variety of conditions including diabetes mellitus, alcoholism,[4] endocrine disorders, pregnancy, drugs, bulimia,[5] eating disorders, idiopathic, ect. Most patients present were between 40 and 70 years of age.
What antibiotics treat sialadenitis?
Initial treatment for sialadenitis is with antibiotics active against S. aureus (eg, dicloxacillin, 250 mg orally 4 times a day, a 1st-generation cephalosporin, or clindamycin), modified according to culture results. With the increasing prevalence of methicillin-resistant S.
What causes inflammation of the salivary glands?
The most common cause of swollen salivary glands, salivary stones are buildups of crystallized saliva deposits. Sometimes salivary stones can block the flow of saliva. When saliva can't exit through the ducts, it backs up into the gland, causing pain and swelling.
What is the correct code for an acute recurrent Sialoadenitis?
22.
How can you tell the difference between a lymph node and a submandibular gland?
0:542:37Parotid Gland and Submandibular Triangle - Lymph Nodes - YouTubeYouTubeStart of suggested clipEnd of suggested clipOne is typically anterior to the submandibular gland. Which you can see here. And then you will haveMoreOne is typically anterior to the submandibular gland. Which you can see here. And then you will have and note that the lymph node is typically darker than and separate from the gland.
How is Sialolithiasis treated?
The classic treatment of sialolithiasis is antibiotics and anti-inflammatory agents, hoping for a spontaneous stone expression through the papilla. In cases of submandibular stones located close to Wharton papillae, a marsupialization (sialodochoplasty) is performed and the stone removed.
What is the treatment for parotitis?
Medical Care. Most episodes of chronic parotitis are treated symptomatically. Sialogogues, local heat, gentle massage of the gland from posterior to anterior, and hydration provide variable symptomatic relief. When pus is expressed from the Stensen duct, culture and sensitivity studies guide antibiotic selection.
What are the symptoms of parotitis?
SymptomsFace pain.Fever.Headache.Sore throat.Loss of appetite.Swelling of the parotid glands (the largest salivary glands, located between the ear and the jaw)Swelling of the temples or jaw (temporomandibular area)
Which virus causes parotitis?
Viral parotitis can be caused by paramyxovirus (mumps), Epstein-Barr virus, coxsackievirus, and influenza A and parainfluenza viruses. Acute suppurative parotitis is generally caused by Staphylococcus aureus, Streptococcus species, and rarely, gram-negative bacteria.
What antibiotics treat parotitis?
For health care associated parotitis, broad spectrum antibiotics are recommended as mentioned in Table 3. Cefoxitin, imipenem, ertapenem, the combination of a penicillin plus beta-lactamase (amoxicillin/clavulanate, ampicillin/sulbactam) will provide adequate coverage.
What is the most common cause of sialadenitis of the submandibular gland (SMG?
Sproll and colleagues (2019) noted that sialolithiasis is the most common cause of chronic sialadenitis of the submandibular gland (SMG). Symptomatic superficial lobe stones are often treated by submandibulectomy. A gland-preserving operation allows for transoral stone removal through endoscopically assisted sialolithotomy. These investigators provided clinical and sonographical follow-up data in patients who underwent sialolithotomy under general anesthesia. A total of 60 patients treated for superficial lobe sialolithiasis of SMG were included in this study. All received transoral sialolithotomy under general anesthesia. Follow-up was carried out via standardized patient questionnaires, clinical examination, and B-mode and color Doppler sonography. Mean patient age was 48.9 years; 56.6 % of right and 43.4 % of left SMG were affected. Mean follow-up was 45 months; 55 of 59 detected stones could be removed. Mean operation time was 71 mins; 3.3 % of patients reported recurrent episodes of post-operative pain and 10 % felt recurrent episodes of gland swelling. Persistent post-operative lingual nerve hypesthesia was described in 1 patient. No facial nerve damages occurred. Salivary flow rates remained reduced in most of the affected glands upon stone removal. Sonographical follow-up data of the previously affected SMG after intra-oral endoscopy-assisted sialolithotomy showed a regular gland size in 70.8 % of cases, a parenchyma free of inflammation in 93.8 %, and without signs of fibrosis in 72.9 % of cases; 68.7 % of patients showed a regular structure of Wharton's duct at time of follow-up. In total, 89.6 % of patients were diagnosed stone-free within both glands on follow-up. No case needed subsequent submandibulectomy. The authors concluded that sialolithotomy of Wharton's duct for removal of stones from the SMG's superficial lobe is a promising alternative to submandibulectomy.
What glands are affected by sialolithiasis?
Stones are rarely found in the sublingual gland. The higher frequency of sialolithiasis in the submandibular gland is associated with several factors: the pH of saliva (alkaline in the submandibular gland, acidic in the parotid gland); the viscosity of saliva (more mucous in the submandibular gland); and the anatomy of the Wharton’s duct (the duct of the submandibular salivary gland opening into the mouth at the side of the frenum linguaean is an “uphill course”).
What is the treatment for salivary gland obstruction?
Sialo-irrigation of the salivary gland is an effective procedure for treating inflammation and providing symptomatic relief. This procedure can be employed for the treatment of sialolithiasis using the back pressure of instilled saline. Sialo-irrigation under ultrasound (US) guidance allows for dynamic studies showing real-time images during diagnostic or surgical procedure and can be used for the removal of sialoliths. Furthermore, it can also be used to remove primitive sialoliths and microliths by washing out the ductal system, which prevents the recurrence of sialoliths. These researchers proposed a minimally invasive technique for sialolithiasis using US-guided sialo-irrigation.
What is the treatment for sialolithiasis?
Sialendoscopy combined with pneumatic lithotripsy for the treatment of sialolithiasis
Is a sialendoscopy necessary for chronic sialadenitis?
Aetna considers sialendoscopy (diagnostic or therapeutic) medically necessary for the management of chronic sialadenitis and sialolithiasis.
Is sialendoscopy safe?
Lele and colleagues (2019) noted that sialendoscopy has emerged as a safe, effective and minimally invasive technique for management of obstructive and inflammatory salivary gland disease. The investigators analyzed outcomes of sialendoscopy and steroid irrigation in patients with sialadenitis without sialoliths. They performed a retrospective analysis of patients who underwent interventional sialendoscopy with steroid irrigation from 2013 to 2016, for the treatment of sialadenitis without sialolithiasis. A total of 22 patients underwent interventional sialendoscopy with ductal dilation and steroid irrigation for the treatment of sialadenitis without any evidence of sialolithiasis. Conservative measures had failed in all; 11 patients had symptoms arising from the parotid gland, 4 patients had symptoms arising from the submandibular gland, while 6 patients had symptoms in both parotid and submandibular glands; 1 patient complained of only xerostomia without glandular symptoms. The mean age of the study group which included 1 male and 21 females was 44.6 years (range of 3 to 86 years); 4 patients had autoimmune disease, while 7 patients had a history of radioactive iodine therapy. No identifiable cause for sialadenitis was found in the remaining 11 patients. The mean follow-up period was 378.9 days (range of 16 to 1,143 days). All patients underwent sialendoscopy with ductal dilation and steroid irrigation; 12 patients showed a complete response (CR) and 9 patients had a partial response (PR), while 1 patient reported no response. Only 3 patients needed repeat sialendoscopy. The authors concluded that the combination of sialendoscopy with ductal dilation and steroid irrigation was a safe and effective therapeutic option for patients with sialadenitis without sialoliths refractory to conservative measures. These researchers stated that prospective studies with a larger case-series are needed to establish its role as a definitive therapeutic option.
What is the ICD-10 code for stenosis of the carotid artery?
I65.2 is a non-billable ICD-10 code for Occlusion and stenosis of carotid artery. It should not be used for HIPAA-covered transactions as a more specific code is available to choose from below.
What is the billable I65.21?
Billable - I65.21 Occlusion and stenosis of right carotid artery
Do you include decimal points in ICD-10?
DO NOT include the decimal point when electronically filing claims as it may be rejected. Some clearinghouses may remove it for you but to avoid having a rejected claim due to an invalid ICD-10 code, do not include the decimal point when submitting claims electronically.
What does the S in the injury code mean?
The ‘S’ is added only to the injury code, not the sequela code. The seventh character ‘S’ identifies the injury responsible for the sequela. The specific type of sequela (e.g. scar) is sequenced first, followed by the injury code.”.
What is the code for scar contractures?
Rationale: Scar contractures due to burn injury are reported with code L90.5 that is the first-listed or principal diagnosis and the burn injury is reported as a secondary code to identify the cause of the sequela.
When is the sequela code expanded?
The sequela code may also be expanded at the fourth, fifth, or sixth character levels to include the manifestation
What is the S93.412S?
S93.412S Sprain of calcaneofibular ligament of the left ankle, sequela
What is the ICD-10 contact?
is: The ICD-10 consists of: an alphabetical index to diseases and nature of injury, external causes of injury, table of drugs and chemicals (Volume 3), and. description, guidelines, and coding rules (Volume 2).
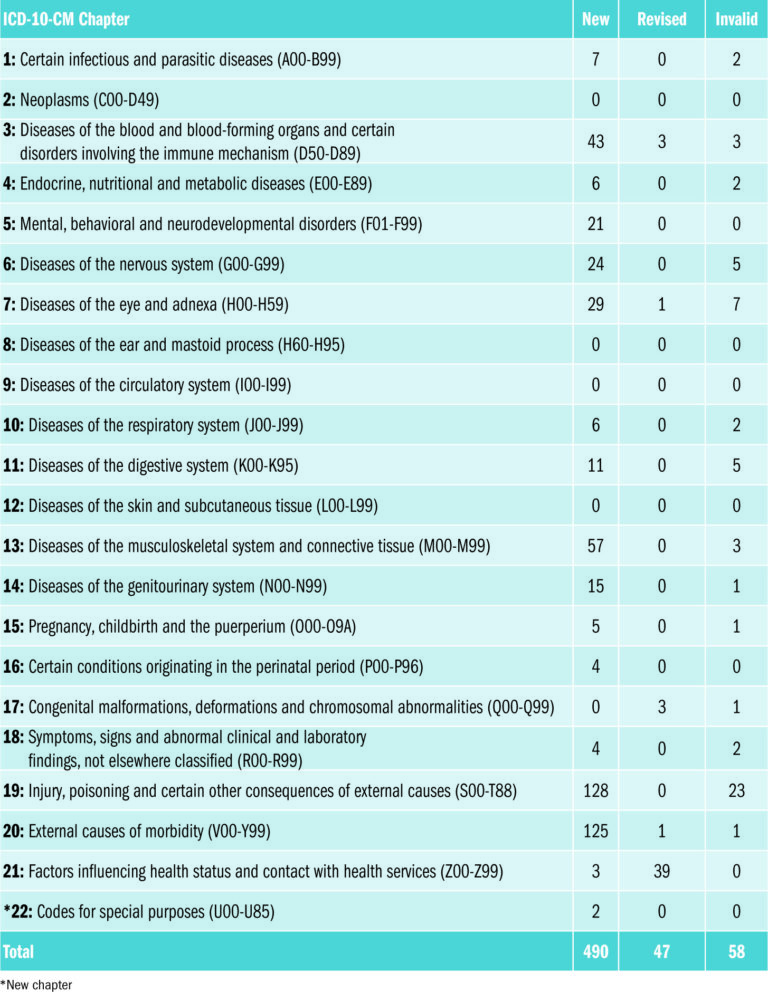
How does the 10th ICD-10 differ from the 9th ICD-10?
The Tenth Revision (ICD-10) differs from the Ninth Revision (ICD-9) in several ways although the overall content is similar: First, ICD-10 is printed in a three-volume set compared with ICD-9’s two-volume set. Second, ICD-10 has alphanumeric categories rather than numeric categories. Third, some chapters have been rearranged, some titles have changed, and conditions have been regrouped. Fourth, ICD-10 has almost twice as many categories as ICD-9. Fifth, some fairly minor changes have been made in the coding rules for mortality.
Popular Posts:
- 1. icd 10 cm code for dysplastic nevus
- 2. icd 10 code for vestibular vertigo
- 3. icd 10 code for high muscle tone
- 4. icd code for transgender
- 5. icd 10 code for sinus
- 6. icd 10 code for gsw to abdomen
- 7. icd 10 code for t cell large granular lymphoma
- 8. icd 10 code for lamotrigine level
- 9. icd code for x ray
- 10. icd 10 code for follow up after hospitalization