What is the ICD-10 code for nursing home placement?
What is the ICD-10 code for assisted living facility?
What is the ICD-10 code for awaiting placement?
What place of occurrence code is used to describe an assisted living facility?
What is the CPT code for skilled nursing?
What is the ICD-10 for abdominal pain?
What is the CPT code for inpatient admission?
What is the ICD-10 code for Transaminitis?
What is the CPT code for inpatient hospital?
How do you sequence ICD-10 codes?
Why do we also code Z codes when initially describing the location of accident or if it is during employment and other of trauma to the patient?
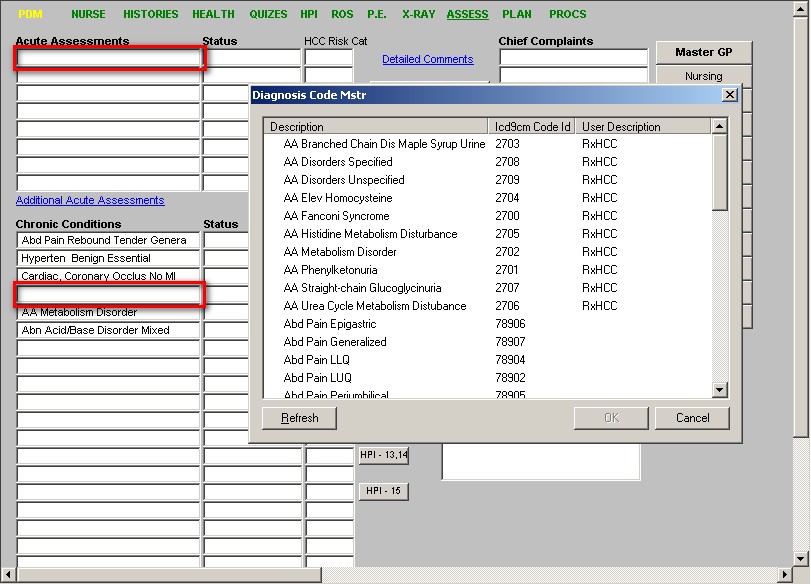
When determining the diagnosis code what is the first step?
- Step 1: Find the condition in the alphabetic index. Begin the process by looking for the main term in the alphabetic index. ...
- Step 2: Verify the code and identify the highest specificity. ...
- Step 3: Review the chapter-specific coding guidelines.
What is a S00 T88 code?
Most often, the condition will be classifiable to Chapter 19, Injury (S00-T88). Codes from Chapter 20 should be used to provide additional information as to the cause of the condition. These codes can answer questions regarding how the injury happened, the location of where it happened and if it was an accident or not.
Does Worker's Comp use ICD-9?
In the USA for all HIPAA-covered entities. So, entities like Worker’s Comp and No -fault may continue to use ICD-9, though CMS has strongly encouraged the transition for these entities as well because the ICD-9 Database will no longer be maintained.
What is the code for a crushing injury of the right shoulder and upper arm?
In cases like these, you will need to use an “x” as a placeholder. For example, S47.1 is the code for “Crushing injury of right shoulder and upper arm.”. It is only 4 characters, but requires a 7th character. In this case, the code would look like this: S47.1 x x A.
What is Chapter 20 code?
Chapter 20 contains codes called “External Causes of Morbidity (V00-Y99)” These codes classify environmental events and circumstances as the cause of injury, and other adverse effects. Where a code from this section is applicable, it is intended that it shall be used secondary to a code from another chapter of the Classification indicating the nature of the condition. Most often, the condition will be classifiable to Chapter 19, Injury (S00-T88). Codes from Chapter 20 should be used to provide additional information as to the cause of the condition. These codes can answer questions regarding how the injury happened, the location of where it happened and if it was an accident or not.
How long does it take to complete a comprehensive assessment for SNF?
When a patient is admitted to a SNF, the admitting physician must perform an initial comprehensive assessment within 30 days of the admission.
Who can provide care for SNF?
Qualified non-physician practitioners (NP, PA, CNS) can provide care for all subsequent SNF visits but the initial visit must be performed by the admitting physician, as governed by the Long-Term Care Regulations.
What is a skilled nursing facility?
Skilled nursing facilities (SNFs) are also commonly referred to as nursing homes. They offer care for different types of medical problems and patients such as: Skilled nursing care for patients who need injections, dressing changes, medication administration, IV therapy, etc. Rehabilitative care for patients who are recuperating from surgery, ...
Is SNF medically predictable?
It is medically predictable at the time of the hospital discharge they need covered care within a pre-determined time period and the care begins within that time. They need skilled nursing or rehabilitation services daily which, as a practical matter, can only be provided in a SNF on an inpatient basis.
Does SNF waive hospitalization?
Certain SNFs that have a relationship with Shared Savings Program (SSP) Accountable Care Organizations (ACOs) may waive the SNF 3-day rule. Occasionally, during a Public Health Emergency, a temporary waiver may be issued as well. Most MA plans waive the 3-day hospitalization requirement.
Does Medicare cover SNF days?
Medicare Advantage (MA), 1876 Cost, or Programs of All-Inclusive Care for the Elderly (PACE) Plans typically waive the 3-day hospitalization requirement. MA plans must cover the same number of SNF days Original Medicare covers, but they may cover more SNF days than Original Medicare.
When does SNF end?
The benefit period ends after the patient discharges from the hospital or has had 60 consecutive days of SNF skilled care.
Why do SNFs need to understand the benefit period concept?
SNFs must understand the benefit period concept because sometimes the SNF must submit claims even when they don’t expect payment. This ensures proper benefit period tracking in the Common Working File (CWF) (for more information, refer to the Special Billing Situations section). The CWF….
How long does SNF last?
The SNF benefit covers 100 days of care per episode of illness with an additional 60-day lifetime reserve. After 100 days, the SNF coverage during that benefit period “exhausts.” The next benefit period begins after patient hospital or SNF discharge for 60 consecutive days.
How long does SNF coverage last?
The benefit period ends after the patient discharges from the hospital or has had 60 consecutive days of SNF skilled care.
Popular Posts:
- 1. icd 10 code for left arm open wound
- 2. icd 10 code for lt foot ulcer
- 3. icd 10 code for known gluten allergy
- 4. icd code for weakness
- 5. icd 10 code for hemophilia c ?
- 6. icd 10 code for period pain
- 7. icd 10 code for elevated folate
- 8. what is the icd 10 code for acute systolic chf
- 9. icd 10 code for unexplained weight loss
- 10. icd-10 code for history of alcohol abuse