| ICD-10: | Z96.82 |
|---|---|
| Short Description: | Presence of neurostimulator |
| Long Description: | Presence of neurostimulator |
Why I passed on the spinal cord stimulator?
Oct 01, 2021 · Z96.82 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z96.82 became effective on October 1, 2021. This is the American ICD-10-CM version of Z96.82 - other international …
Do I need a spinal cord stimulator?
Oct 01, 2021 · Z45.42 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z45.42 became effective on October 1, 2021. This is the American ICD-10-CM version of Z45.42 - other international …
What are spinal cord stimulators and how do they work?
ICD-10-CM (diagnosis) Coding Guide for Spinal Cord Stimulation. NM-339101-AA SEP2015 Page 1 of 4. ICD-10-CM (diagnosis) Coding Guide for Spinal Cord Stimulation. On October 1, 2015 CMS will implement the ICD-10-Clinical Modification (ICD-10-CM) code set and the ICD-10-Procedure …
Does spinal cord have pain receptors?
Apr 16, 2021 · This is the doctors notes for the procedure and Dx: CPT-4 and ICD-10 codes for Spinal Cord Stimulator pulse generator (battery) replacement, for a diagnosis of Spinal cord …
What is the ICD-10 code for presence of spinal stimulator?
How do you code a spinal cord stimulator?
What is a neurostimulator implant?
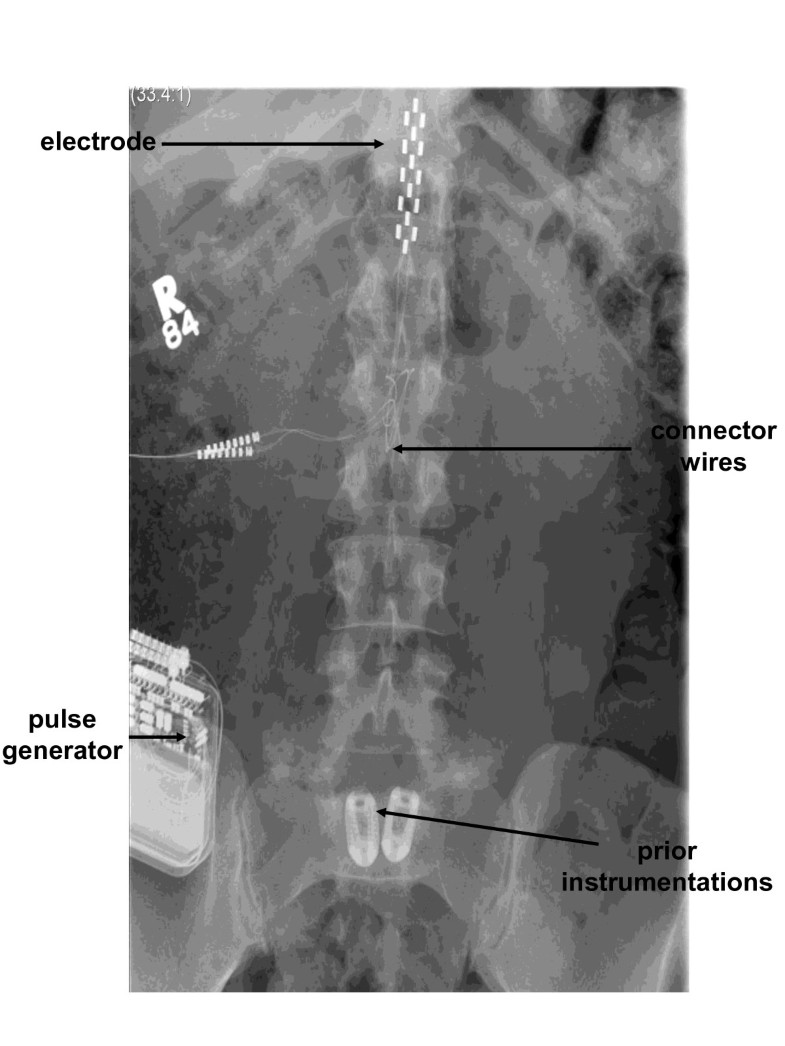
What is a neurostimulator electrode array?
What is the difference between CPT 63685 and 63688?
What is included in CPT code 63685?
Where is a spinal cord stimulator placed?
Is a spinal cord stimulator the same as a TENS unit?
What is the difference between neuromodulation and neurostimulation?
What are three primary components of stimulation?
What is procedure code 64555?
What is procedure code 63655?
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS), the federal agency responsible for administration of the Medicare, Medicaid and the State Children's Health Insurance Programs, contracts with certain organizations to assist in the administration of the Medicare program. Medicare contractors are required to develop and disseminate Articles. CMS believes that the Internet is an effective method to share Articles that Medicare contractors develop. While every effort has been made to provide accurate and complete information, CMS does not guarantee that there are no errors in the information displayed on this web site. THE UNITED STATES GOVERNMENT AND ITS EMPLOYEES ARE NOT LIABLE FOR ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION, PRODUCT, OR PROCESSES DISCLOSED HEREIN. Neither the United States Government nor its employees represent that use of such information, product, or processes will not infringe on privately owned rights. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information, product, or process.
What is a local coverage article?
Local Coverage Articles are a type of educational document published by the Medicare Administrative Contractors (MACs). Articles often contain coding or other guidelines that are related to a Local Coverage Determination (LCD).
What is a bill and coding article?
Billing and Coding articles provide guidance for the related Local Coverage Determination (LCD) and assist providers in submitting correct claims for payment. Billing and Coding articles typically include CPT/HCPCS procedure codes, ICD-10-CM diagnosis codes, as well as Bill Type, Revenue, and CPT/HCPCS Modifier codes. The code lists in the article help explain which services (procedures) the related LCD applies to, the diagnosis codes for which the service is covered, or for which the service is not considered reasonable and necessary and therefore not covered.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
What does "you" mean when acting on behalf of an organization?
If you are acting on behalf of an organization, you represent that you are authorized to act on behalf of such organization and that your acceptance of the terms of this agreement creates a legally enforceable obligation of the organization. As used herein, “you” and “your” refer to you and any organization on behalf of which you are acting.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
What information is needed for a patient's medical record?
Every page of the record must be legible and include appropriate patient identification information (e.g., complete name, dates of service [s]). The documentation must include the legible signature of the physician or non-physician practitioner responsible for and providing the care to the patient.
What is coding for Medicare?
The coding includes information on the diagnosis and procedure codes applicable to all sites-of-service to be used when billing, along with Medicare National Average payment rates. For specific coding assistance with your facility, please contact your local Health Economic Manager. The codes in the documents below are up to date through:
Is Medtronic a recommendation?
Medtronic provides this information for your convenience only. It is not intended as a recommendation regarding clinical practice. It is the responsibility of the provider to determine coverage and submit appropriate codes, modifiers, and charges for the services rendered.
What is CPT code 63663?
CPT code 63663 (revision of a percutaneously implanted system) would only be used if a previous permanent (internalized system) array of neurostimulator electrodes had been percutaneously placed, and is now being revised or replaced to improve efficacy.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS), the federal agency responsible for administration of the Medicare, Medicaid and the State Children's Health Insurance Programs, contracts with certain organizations to assist in the administration of the Medicare program. Medicare contractors are required to develop and disseminate Articles. CMS believes that the Internet is an effective method to share Articles that Medicare contractors develop. While every effort has been made to provide accurate and complete information, CMS does not guarantee that there are no errors in the information displayed on this web site. THE UNITED STATES GOVERNMENT AND ITS EMPLOYEES ARE NOT LIABLE FOR ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION, PRODUCT, OR PROCESSES DISCLOSED HEREIN. Neither the United States Government nor its employees represent that use of such information, product, or processes will not infringe on privately owned rights. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information, product, or process.
What is the CPT code for spinal neurostimulator?
CPT codes 63650, 63655, and 63661-63664 describe the operative placement, revision, replacement, or removal of the spinal neurostimulator system components to provide spinal electrical stimulation.
What is the L36035?
This First Coast Billing and Coding Article for Local Coverage Determination (LCD) L36035 Spinal Cord Stimulation for Chronic Pain provides billing and coding guidance for frequency limitations as well as diagnosis limitations that support diagnosis to procedure code automated denials. However, services performed for any given diagnosis must meet all of the indications and limitations stated in the LCD, the general requirements for medical necessity as stated in CMS payment policy manuals, any and all existing CMS national coverage determinations, and all Medicare payment rules.
What does "you" mean when acting on behalf of an organization?
If you are acting on behalf of an organization, you represent that you are authorized to act on behalf of such organization and that your acceptance of the terms of this agreement creates a legally enforceable obligation of the organization. As used herein, “you” and “your” refer to you and any organization on behalf of which you are acting.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
What is the minimum reduction of pain in a trial?
Documentation must include evidence to support a successful trial was performed with at least a 50% reduction of target pain, or 50% reduction of analgesic medications, and should show some element of functional improvement.
Popular Posts:
- 1. icd 10 code for peripheral vascular occlusive disease
- 2. icd 10 cm code for recurrent moderate mdd
- 3. icd-10 code for quadriplegia due to spinal cord injury
- 4. icd 10 cm code for endometrial carcinoma
- 5. icd 9 code for urinary retention due to foley
- 6. 2015 icd 10 code for laceration right toe first digi
- 7. icd 9 code for acute on chronic respiratory failure due to sarcolosis involovin the lung.
- 8. icd 10 code for ibs with constipation and diarrhea
- 9. icd-10 code for coccydynia
- 10. icd 10 code for accident to the head