Can pre-existing conditions be listed as additional diagnosis codes?
Pre-existing and chronic conditions and history codes may also be included as additional codes as long as the examination is for administrative purposes and note focused on any particular condition. 13,505 Columbia, MO 2 #9 According to the guidelines and examples in the ICD10 book, it's acceptable to list other diagnosis codes.
What is the ICD 10 code for secondary diagnosis?
The coding guidelines state that chronic conditions or additional diagnoses found upon examination of a patient during a routine health exam can be coded as secondary diagnoses. Chapter 21 of the ICD 10 book states that nonspecific abnormal findings are coded using R70-R94.
When should a diagnosis code not be used during an exam?
The codes are not to be used if the examination is for diagnosis of a suspected condition or for treatment purposes. In such cases the diagnosis code is used. During a routine exam, should a diagnosis or condition be discovered, it should be coded as an additional code.
What do you code as complications in DX?
You code only complaints and symptoms or definitive DX for the encounter plus any chronic conditions that are managed controlled or treated or any mentions as complicating factors. You must log in or register to reply here.
What is code Z71 89?
ICD-10 code Z71. 89 for Other specified counseling is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is the ICD 10 code Z13 89?
Code Z13. 89, encounter for screening for other disorder, is the ICD-10 code for depression screening.
What is the ICD 10 code for critical care?
99291Code 99291 is used for critical care, evaluation, and management of a critically ill or critically injured patient, specifically for the first 30-74 minutes of treatment. It is to be reported only once per day, per physician or group member of the same specialty.
What is ICD 10 code for medication management?
ICD-10-PCS GZ3ZZZZ is a specific/billable code that can be used to indicate a procedure.
What is code Z12 39?
39 (Encounter for other screening for malignant neoplasm of breast). Z12. 39 is the correct code to use when employing any other breast cancer screening technique (besides mammogram) and is generally used with breast MRIs.
What is Z13 40?
ICD-10 code Z13. 40 for Encounter for screening for unspecified developmental delays is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What qualifies for critical care time?
To bill critical care time, emergency physicians must spend 30 minutes or longer on patient care. Used to report the additive total of the first 30-74 minutes of critical care performed on a given date. Critical care time totaling less than 30 minutes is reported using the appropriate E/M code.
How do you code critical care services?
Critical care codes 99291 (evaluation and management of the critically ill or critically injured patient, first 30-74 minutes) and 99292 (critical care, each additional 30 minutes) are used to report the total duration of time spent by a provider providing critical care services to a critically ill or critically ...
What counts as critical care?
Critical care is medical care for people who have life-threatening injuries and illnesses. It usually takes place in an intensive care unit (ICU). A team of specially-trained health care providers gives you 24-hour care. This includes using machines to constantly monitor your vital signs.
What does diagnosis code Z51 81 mean?
ICD-10 code Z51. 81 for Encounter for therapeutic drug level monitoring is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is the ICD-10 Z51 81?
Z51. 81 Encounter for therapeutic drug level monitoring - ICD-10-CM Diagnosis Codes.
What is diagnosis code Z79 899?
ICD-10 Codes for Long-term TherapiesCodeLong-term (current) use ofZ79.899other drug therapyH – Not Valid for Claim SubmissionZ79drug therapy21 more rows•Aug 15, 2017
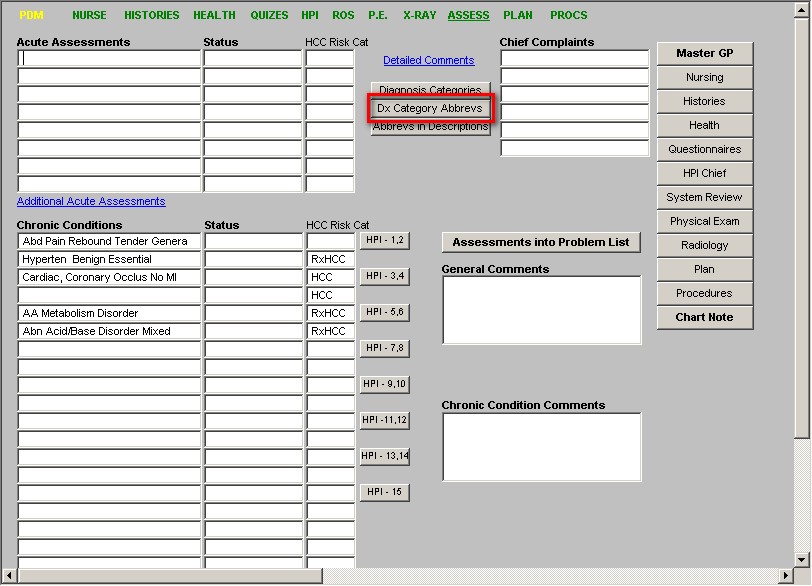
How to code chronic conditions?
Employing best practices and adhering to Medicare guidelines for documenting and coding chronic conditions can help ensure revenue optimization, as well as enhance quality of care. Here are a few essential practices that should be followed: 1 All pertinent information should be included in the provider’s progress notes. Report everything from the office visit that affects the plan of care for the chronic condition. 2 Chronic conditions must be coded annually with the highest level of specificity. 3 Patients must be evaluated by a medical doctor, a DO, a nurse practitioner, or an advanced practice provider during a face-to-face visit. 4 All chronic conditions should be discussed and documented when meeting with a new patient. If the condition does not affect the patient’s care six months from the initial visit, there is no need to report it again. 5 Document only confirmed diagnoses, not suspected conditions. 6 Do not cut and paste the patient’s problem list and transfer it into the progress notes. Providers must link the chronic condition with the care plan by evaluating, assessing, monitoring, or treating the condition in some way, documenting care they provided or plan to provide. If chronic conditions are not linked to the care plan and a data validation audit occurs, the code will be removed and not counted as part of the patient’s risk adjustment factor. 7 Progress notes must be signed by the provider for chronic conditions to count for an office visit.
Why is coding important in value based care?
First, it provides the necessary information in the patients’ records to make sure physicians are proactively monitoring and managing all ongoing chronic conditions. Not only does this enable high-quality, ...
What is risk adjustment in Medicare?
The goal of risk adjustment is to pay Medicare Advantage and prescription drug programs accurately and fairly by adjusting payments for enrollees based on demographics and health status.
What percentage of HCCs are not complications or comorbidities?
Chronic conditions can be resource-intensive, so they may have an impact on the population health risk adjustment model when they have none on the inpatient model. Forty percent of HCCs are neither complications or comorbidities (CCs) nor major CCs (MCCs). (For the CMS-HCC model, go online to ...
Is I73.9 a HCC?
Although I73.9, peripheral vascular disease, unspecified lives in HCC 108, if what you really have is a patient with atherosclerosis of a leg with ulceration, you should really be in HCC 106 – which, according to the hierarchy, should yield a risk adjustment factor of 1.461 instead of 0.298.
What is Z00 code?
The Z00 codes allow for abnormal findings with the code choice for with abnormal findings. That is not the same as a patient that presents with symptoms. And as you stated if the patient presents with a problem you cannot use the Z00 codes.
Can you use a Z code on an ICD10 exam?
Under Chapter 21, section 13 it states that you don't use the Z codes if the exam is for diagnosis of a suspected condition. In such cases the diagnosis code is used.
Can you use Z00 codes on a patient?
That is not the same as a patient that presents with symptoms. And as you stated if the patient presents with a problem you cannot use the Z00 codes. The codes are not to be used if the examination is for diagnosis of a suspected condition or for treatment purposes. In such cases the diagnosis code is used.
When to use condition code xx8?
Condition code only applicable on a xx8 type of bill. Use when canceling a claim for reasons other than the Medicare ID or provider number. Use when canceling a claim to repay a payment. Condition code only applicable to a xx8 type of bill.
When to use D9?
When you are only changing the admit date use condition code D9. Use used when the original claim shows Medicare on the primary payer line and now the adjustment claim shows Medicare on the secondary payer line. Use D9 when adjusting primary payer to bill for conditional payment.

Popular Posts:
- 1. icd 10 code for rheumatic tricuspid regurgitation
- 2. icd 10 code for fluoxetine poisoning
- 3. icd code for bronchial asthma
- 4. icd-10 code for ddd unspecified
- 5. icd 10 code for arterial disease with left leg gangrene
- 6. icd 9 code for oropharyngeal ulcer
- 7. icd 10 code for dehydration complicating pregnancy
- 8. icd 10 code for coronary artery quadruple bypass graft
- 9. icd 10 code for flank pain right side
- 10. preop icd 10 code for pulmonary function test