Is Stage 3 necrotic decubitus ulcer of left heel associated with diabetes?
The provider's final diagnostic statement states, "stage 3 necrotic decubitus ulcer of left heel associated with diabetic neuropathy and peripheral vascular disease." Because the provider documented an association between diabetes and a decubitus ulcer, which condition would be sequenced as the principal diagnosis?
What is the ICD 10 code for pressure ulcer Stage 3?
Pressure ulcer stage 3 of right lower leg Pressure ulcer stage 3 of toes ICD-10-CM L89.893 is grouped within Diagnostic Related Group (s) (MS-DRG v38.0): 573 Skin graft for skin ulcer or cellulitis with mcc
What is the ICD 10 code for pressure ulcer left heel?
The coder would then report ICD-10-CM code L89.623 (pressure ulcer of left heel, stage 3), as a secondary diagnosis. The coder would assign codes E11.51 (Type 2 diabetes mellitus with diabetic peripheral angiopathy without gangrene) and E11.40 (Type 2 diabetes mellitus with neurological complications) as additional diagnoses.
What is a decubitus ulcer?
The etymology of the term “decubitus ulcer” is from the Latin, decumbere, which means “to lie down,” and thus it really relates to patients who are recumbent.
What is a Stage 3 Pressure ulcer?
Stage 3 bedsores (also known as stage 3 pressure sores, pressure injuries, or decubitus ulcers) are deep and painful wounds in the skin. They are the third of four bedsore stages. These sores develop when a stage 2 bedsore penetrates past the top layers of skin but has yet not reached muscle or bone.
What is the ICD-10 code for left decubitus ulcer?
ICD-10 code L89. 62 for Pressure ulcer of left heel is a medical classification as listed by WHO under the range - Diseases of the skin and subcutaneous tissue .
How do you report a Pressure ulcer of the left heel Stage 3 in ICD-10-CM?
The coder would then report ICD-10-CM code L89. 623 (pressure ulcer of left heel, stage 3), as a secondary diagnosis.
How do you code decubitus ulcers?
“Two codes are needed to completely describe a pressure ulcer: A code from subcategory 707.0, Pressure ulcer, to identify the site of the pressure ulcer and a code from subcategory 707.2, Pressure ulcer stages.
What is the difference between a Pressure ulcer and a non-Pressure ulcer?
The term “non-pressure ulcer” was coined to designate a primary mechanism other than shear or pressure. If there is poor circulation, such as that caused by venous or arterial insufficiency or excessive moisture or trauma, a patient may develop a non-pressure ulcer.
Is a diabetic ulcer a Pressure ulcer or non-Pressure ulcer?
Diabetic ulcers may look similar to pressure ulcers; however, it is important to note that they are not the same thing. As the name may imply, diabetic ulcers arise on individuals who have diabetes, and the foot is one of the most common areas affected by these skin sores.
What is the ICD-10 code for pressure ulcer?
Pressure ulcer of unspecified site, unspecified stage L89. 90 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM L89. 90 became effective on October 1, 2021.
What is ICD-10 code for Left foot Pain?
ICD-10 code M79. 672 for Pain in left foot is a medical classification as listed by WHO under the range - Soft tissue disorders .
How many codes are required to code a pressure ulcer site and stage?
two separate codesIf a patient is admitted to an inpatient hospital with a pressure ulcer at one stage and it progresses to a higher stage, two separate codes should be assigned: one code for the site and stage of the ulcer on admission and a second code for the same ulcer site and the highest stage reported during the stay.
When the pressure ulcer stage is not documented how should the stage be coded?
When the stage of the pressure ulcer is not documented, the appropriate ICD-10-CM code for unspecified stage (L89. –9) should be assigned. If the documentation is not clear whether pressure ulcer is current or being treated, you should ask the provider.
WHO may document the stage of pressure ulcers?
Rugg reemphasizes that providers or another clinician—such as a wound care nurse—can document the stages. ICD-10 guidelines for POA are clear, according to Robin. The physician provider is responsible for documenting the diagnosis of a pressure ulcer.
Is a Kennedy Terminal ulcer A pressure ulcer?
A study found that 62.5% of people in hospice care had pressure ulcers in their last 2 weeks of life. Many of these pressure ulcers may actually be Kennedy terminal ulcers. Shape. Kennedy ulcers have been described as butterfly-shaped, pear-shaped, or irregularly-shaped.
What is the sequence of a pressure ulcer?
The sequence depends on the pressure ulcer being treated. If all the pressure ulcers are being treated, sequence the code for the most severe pressure ulcer first. Example: A patient with a stage 3 pressure ulcer on her left heel and a stage 2 pressure ulcer of her left hip is scheduled for debridement.
What is an unstageable ulcer?
An unstageable ulcer is when the base of the ulcer is covered in eschar or slough so much that it cannot be determined how deep the ulcer is. This diagnosis is determined based on the clinical documentation. This code should not be used if the stage is not documented.
What is pressure ulcer?
Pressure ulcers are areas of damaged skin and tissue developing as a result of compromised circulation. When a patient stays in one position without movement, the weight of the bones against the skin inhibits circulation and causes an ulceration of the tissue. Pressure ulcers usually form near the heaviest bones (buttocks, hips, and heels).
Where do pressure ulcers form?
Pressure ulcers usually form near the heaviest bones (buttocks, hips, and heels). There are stages of pressure ulcers that identify the extent of the tissue damage. Stage 1—Persistent focal erythema. Stage 2—Partial thickness skin loss involving epidermis, dermis, or both.
Can a pressure ulcer get worse?
If the pressure ulcer is healed completely , a code is not reported for the pressure ulcer. There are some cases where the pressure ulcer will get worse during the course of the admission. For example, the patient is admitted for treatment of a stage 2 ulcer that progresses to stage 3.
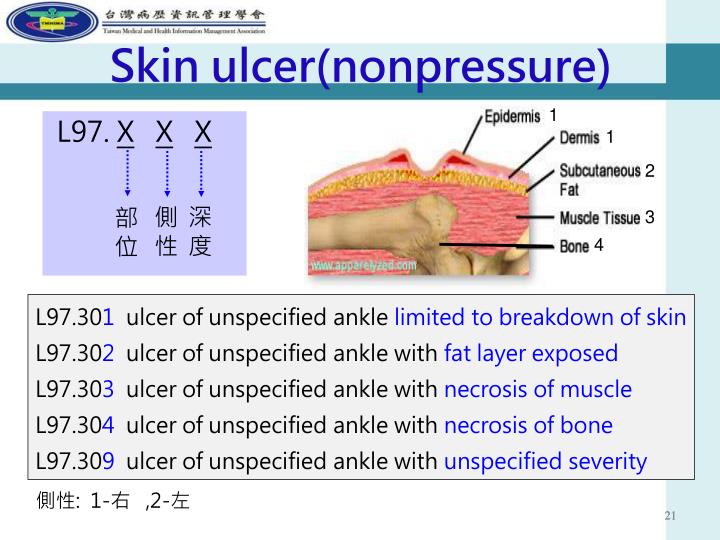
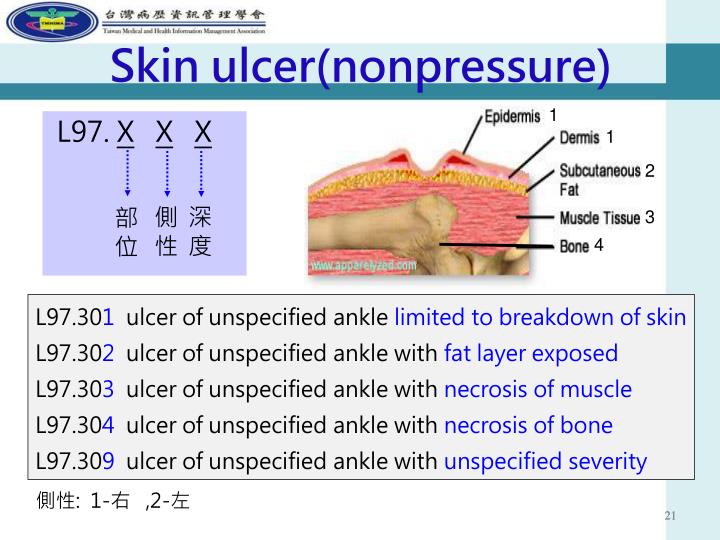
What are the different types of ulcers?
Non-pressure chronic ulcer of lower limb, not elsewhere classified L97- 1 chronic ulcer of skin of lower limb NOS 2 non-healing ulcer of skin 3 non-infected sinus of skin 4 trophic ulcer NOS 5 tropical ulcer NOS 6 ulcer of skin of lower limb NOS
What is a type 2 exclude note?
A type 2 excludes note indicates that the condition excluded is not part of the condition it is excluded from but a patient may have both conditions at the same time. When a type 2 excludes note appears under a code it is acceptable to use both the code ( L97) and the excluded code together.
Why was gangrenous pressure ulcer admitted?
The primary reason for the admission was for treatment of the gangrenous pressure ulcer. This was not a diabetic ulcer. Diabetic ulcers typically involve the foot and toes. Pressure ulcers develop in tissue near bony prominences, such as the elbows, tailbone, greater trochanters, or heels.
Does diabetes mellitus cause pressure ulcers?
Although diabetes mellitus may increase the risk of pressure ulcers because of its association with neuropathy and angiopathy, ICD- 10-CM doesn’t classify pressure ulcers the same way as diabetic ulcers.
What is the L89 code for a pressure ulcer?
Pressure injuries with skin breakdown are considered pressure ulcers. An additional L89 code specifies the stage (depth of tissue injury) and the anatomical site. Pressure ulcers form in sites that experience shear or pressure, typically in tissue overlying bony prominences such as elbows, the sacrum, hips, or heels.
What causes diabetic foot ulcers?
A “diabetic foot ulcer,” which is caused exclusively by hyperglycemia, in the absence of neuropathy or ischemia, is a rarity. That term almost always refers to an ulcer on the foot of a diabetic that derives from neuro/ischemic etiology, as opposed to being strictly and principally due to pressure injury.
What happens when blood sugar is low?
Poorly controlled blood sugars weaken the small blood vessel walls and predispose patients to arteriosclerosis. This impairs the circulation and causes ischemia of the soft tissues, especially of the lower extremities. Many diabetics have both diabetic peripheral neuropathy and angiopathy.
Why do diabetics get ulcers?
The American Podiatric Medical Association adds that “ (diabetic foot) ulcers form due to a combination of factors , such as lack of feeling in the foot, poor circulation, foot deformities, irritation (such as friction or pressure), and trauma, as well as duration of diabetes .”. They go on to note that “vascular disease can complicate a foot ulcer, ...
Why are pressure ulcers considered a patient safety indicator?
Pressure ulcers are deemed patient safety indicators and hospital acquired conditions because a concerted program for prevention and treatment can prevent them and protect our patients from iatrogenic harm. The diagnosis of a “pressure ulcer” may trigger prevalence and incident reporting.
Can diabetes cause heel ulcers?
Heel ulcers, however, are usually a consequence of a pressure injury, although it is also possible to have another mechanism cause a non-pressure injury involving the heel. Diabetes may accelerate or complicate the injury. Neuropathy results in malum perforans pedis (a.k.a. bad perforating foot) ulcers.
Is diabetes mellitus a secondary condition?
There are medical diagnoses that predispose patients to develop secondary conditions. Diabetes mellitus is a pervasive endocrinopathy whereby hyperglycemia affects every organ and system in the body, including the nerves and blood vessels. It makes a patient more prone to infection and poor healing.
Popular Posts:
- 1. icd 9 code for h69.91
- 2. icd 10 code for failed ercp
- 3. icd 10 code for synechiae of the right nasal cavity
- 4. icd-9 code for radiation induced proctitis
- 5. icd 10 code for t10-t11 diskitis.
- 6. icd 10 code for abdominal cramping in pregnancy
- 7. icd 10 code for marital discord
- 8. icd 10 code for xray
- 9. icd 10 code for i71.4
- 10. icd-10 code for previous lumbar stenosis