What is marginal keratitis ICD 10?
Marginal Keratitis - ICD-10 H16.39 (Other Interstitial and Deep Keratitis) Other names: Staphylococcal Marginal Keratitis; Catarrhal infiltrates. Marginal keratitis is an inflammatory disease of the peripheral cornea, characterized by peripheral stromal infiltrates which are often associated with epithelium break down and ulceration.
What causes marginal keratitis (staphylococcal infection)?
Marginal keratitis is thought to be the product of an inflammatory reaction against staphylococcal antigens (rather than a direct staphylococcal infection of the cornea).
What is another name for staphylococcal keratitis?
Other names: Staphylococcal Marginal Keratitis; Catarrhal infiltrates. Marginal keratitis is an inflammatory disease of the peripheral cornea, characterized by peripheral stromal infiltrates which are often associated with epithelium break down and ulceration.
Is marginal keratitis a type III hypersensitivity reaction?
Marginal keratitis is thought to be the product of an inflammatory reaction against staphylococcal antigens (rather than a direct staphylococcal infection of the cornea). The presence of bacterial antigens in the peripheral area of the cornea possibly triggers a type III hypersensitivity reaction,...
What is staph marginal keratitis?
Marginal keratitis, sometimes referred to as staphylococcal marginal keratitis, is an inflammation of the outer edge of the cornea. The cornea is the clear dome- shaped window in the front of the eye. Its main job is to help focus light as it enters the eyes.
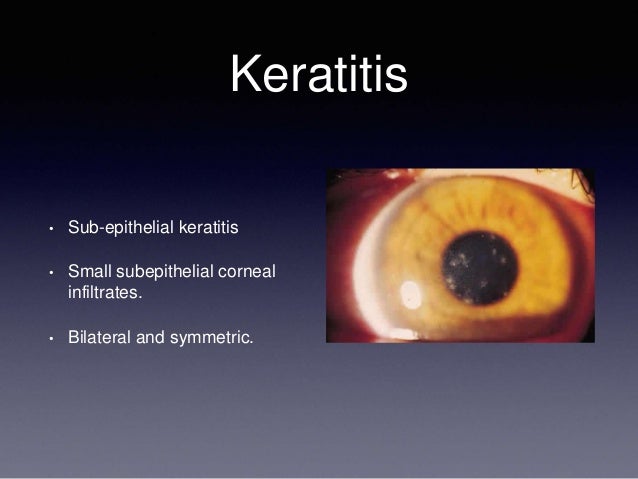
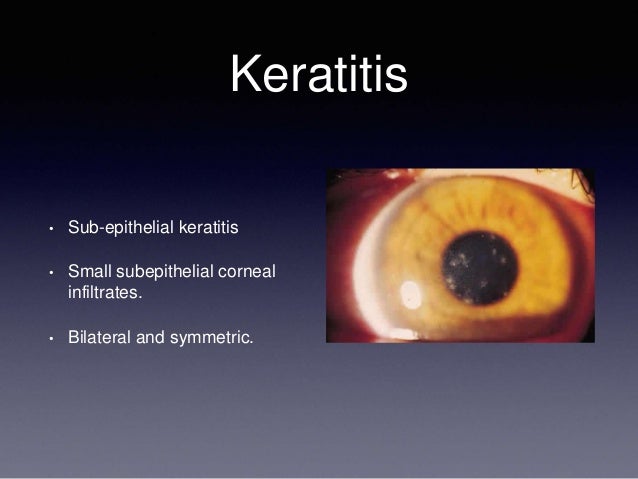
What is marginal keratitis?
Marginal keratitis is an inflammatory disease of the peripheral cornea, characterized by peripheral stromal infiltrates which are often associated with epithelium break down and ulceration.
What is the ICD 10 code for bacterial keratitis?
Unspecified interstitial keratitis, bilateral H16. 303 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM H16. 303 became effective on October 1, 2021.
What is the ICD 10 code for exposure keratitis?
ICD-10 code H16. 21 for Exposure keratoconjunctivitis is a medical classification as listed by WHO under the range - Diseases of the eye and adnexa .
What is infectious keratitis?
Bacterial keratitis is an infection of the cornea (the clear dome covering the colored part of the eye) that is caused by bacteria. It can affect contact lens wearers, and also sometimes people who do not wear contact lenses. Types of bacteria that commonly cause bacterial keratitis include: Pseudomonas aeruginosa.
What is a marginal eye ulcer?
A marginal ulcer is a small ulcer on the front part of your eye, the cornea. The cornea is the clear 'window' of the eye'. An 'ulcer' is a shallow crater, similar in appearance to a crater on the surface of the moon.
How is infectious keratitis diagnosed?
Your doctor will examine your eyes with a special instrument called a slit lamp. It provides a bright source of light and magnification to detect the character and extent of keratitis, as well as the effect it may have on other structures of the eye.
What is unspecified keratitis?
Diseases of the eye and adnexa A disorder characterized by inflammation to the cornea of the eye. Inflammation of the cornea. Inflammation of the cornea.
How common is bacterial keratitis?
Epidemiology, regarding contact lenses as significant risk factor for bacterial corneal infections, is very significant. The annual incidence of ulcerative keratitis in contact lens wearers is 4–21 per 10,000 daily wear and extended wear soft contact lens wearers.
What is ICD 10 code for eye irritation?
H53. 141 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM H53.
What is the ICD 10 code for corneal abrasion?
The general ICD-10 code to describe the initial evaluation of a patient with a corneal abrasion using ICD-10 is: S05. 02XA – Injury of conjunctiva and corneal abrasion without foreign body, left eye, initial encounter.
What does Lagophthalmos mean?
Lagophthalmos is the incomplete or defective closure of the eyelids. The inability to blink and effectively close the eyes leads to corneal exposure and excessive evaporation of the tear film.
What causes keratitis of the eye?
Noninfectious keratitis can be caused by a relatively minor injury, by wearing your contact lenses too long or by a foreign body in the eye. Infectious keratitis can be caused by bacteria, viruses, fungi and parasites.
Can you go blind from keratitis?
Corneal scarring is the most common complication of keratitis, which can lead to vision loss. If keratitis is not treated in a timely manner, the infection could go through the cornea and spread to other areas of the eye leading to possible blindness.
What is keratitis and how is it treated?
Keratitis caused by fungi typically requires antifungal eyedrops and oral antifungal medication. Viral keratitis. If a virus is causing the infection, antiviral eyedrops and oral antiviral medications may be effective. Other viruses need only supportive care such as artificial tear drops.
Is Marginal keratitis self limiting?
Marginal keratitis is a self-limiting, common inflammatory condition that most often occurs secondary to staphylococcal blepharoconjunctivitis (ie, an overgrowth of Staphylococcus in the margins of the eyelid and conjunctiva), but may also be associated with other conditions including meibomitis, and rosacea.
What is marginal keratitis?
S. marginal keratitis is a sometimes-chronic inflammatory keratitis that occurs in the cornea’s periphery and can cause epithelial breakdown and ulcer development. It is often linked with contact lens contamination from MGD and blepharitis.
Can O.D.s diagnose marginal keratitis?
While not clinically challenging, we, as O.D.s must be able to diagnose marginal keratitis, as it’s a common issue seen in clinic. Also, it’s important to remember adjunctive lid hygiene treatments to make this sometime-chronic infection a less frequent nuisance. OM
Popular Posts:
- 1. icd-10 code for left otitis media
- 2. icd 10 code for spinal surgery
- 3. 2017 icd 10 code for metalic foreign bodies foot
- 4. icd-10 code for right frontal intracranial hemorrhage with edema, mass effect with midline shift
- 5. icd 10 code for hip flexor strain
- 6. icd 10 code for wound dehiscence right upper thigh
- 7. icd 10 code for face laceration
- 8. icd code for muscle cramps
- 9. icd 10 cm code for a right and left heart catheterization
- 10. icd code for death due to cancer