What ICD 10 code will cover CMP?
ICD-10-CM Diagnosis Code O99.844 Bariatric surgery status complicating childbirth 2016 2017 2018 2019 2020 2021 2022 Billable/Specific Code Maternity Dx (12-55 years)
What is the ICD 10 diagnosis code for?
Oct 01, 2021 · 2022 ICD-10-CM Diagnosis Code Z98.89 2022 ICD-10-CM Diagnosis Code Z98.89 Other specified postprocedural states 2016 2017 - Converted to Parent Code 2018 2019 2020 2021 2022 Non-Billable/Non-Specific Code Z98.89 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail.
What is the diagnosis code for post op?
colonization status ( Z22.-) ICD-10-CM Diagnosis Code Z01.41. Encounter for routine gynecological examination. gynecologic examination status-post hysterectomy for malignant condition (Z08); screening cervical pap smear not a part of a routine gynecological examination (Z12.4); Encounter for general gynecological examination with or without cervical smear; …
What is ICD 10 code for?
Oct 01, 2015 · The following ICD-10-CM codes have been added to the list of ICD-10-CM codes that support medical necessity, Group 1 codes: K50.00, K50.90, K51.90, K51.911, K51.912, K51.913, K51.914, and K51.918, in response to an external inquiry.

What is the ICD-10 code for status post procedure?
ICD-10-CM Code for Encounter for surgical aftercare following surgery on specified body systems Z48. 81.
When do you code Z98 890?
Code Classification 890 is a billable diagnosis code used to specify a medical diagnosis of other specified postprocedural states. The code Z98. 890 is valid during the fiscal year 2022 from October 01, 2021 through September 30, 2022 for the submission of HIPAA-covered transactions.
What is diagnosis code Z98 89?
Not Valid for SubmissionICD-10:Z98.89Short Description:Other specified postprocedural statesLong Description:Other specified postprocedural states
What is the ICD-10 code for status post endarterectomy?
Valid for SubmissionICD-10:Z98.62Short Description:Peripheral vascular angioplasty statusLong Description:Peripheral vascular angioplasty status
What is the ICD-10 code for status post lithotripsy?
Z87. 442 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z87. 442 became effective on October 1, 2021.
What is the ICD-10 code for status post discectomy?
2022 ICD-10-CM Diagnosis Code M96. 1: Postlaminectomy syndrome, not elsewhere classified.
What is the ICD-10 code for status post Cranioplasty?
ICD-10-CM Code for Encounter for surgical aftercare following surgery on the nervous system Z48. 811.
What is the ICD-10 code for ASHD?
I25. 10 - Atherosclerotic Heart Disease of Native Coronary Artery Without Angina Pectoris [Internet]. In: ICD-10-CM. Centers for Medicare and Medicaid Services and the National Center for Health Statistics; 2018.
What is the ICD-10 code for status post laminectomy?
M96.1ICD-10-CM Code for Postlaminectomy syndrome, not elsewhere classified M96. 1.
Is endarterectomy the same as angioplasty?
Carotid endarterectomy is the standard treatment for atherosclerotic stenosis of the internal carotid artery. Carotid angioplasty is gaining increasing popularity as a less invasive technique in symptomatic patients with severe (>70%) carotid artery stenosis especially in those with significant co-morbidities.Jan 15, 2007
What is the ICD 10 code for status post stent?
ICD-10-CM Code for Presence of coronary angioplasty implant and graft Z95. 5.
What is meant by endarterectomy?
Definition of endarterectomy : surgical removal of the inner layer of an artery when thickened and atheromatous or occluded (as by intimal plaques)
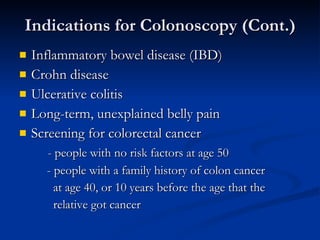
What is a screening colonoscopy?
General definitions of procedure indications from various specialty societies , including the ACA: * A screening colonoscopy is done to look for disease, such as cancer, and treat early conditions, if indicated, in people without symptoms. * A diagnostic colonoscopy is done to confirm or rule out a condition in a person who is symptomatic ...
What is colonoscopy procedure?
Definition of Terms Colonoscopy: A colonoscopy is a procedure that permits the direct examination of the mucosa of the entire colon by using a flexible lighted tube. The procedure is done with sedation in a hospital outpatient department, in a clinic , or an office facility. During the colonoscopy a doctor can biopsy and remove pre – cancerous ...
What is a provider policy?
A provider also can be a place where medical care is given, like a hospital, clinic, or lab.This policy informs them about when a service may be covered.
Is colonoscopy a screening test?
This guideline applies only to people of average risk. Colonoscopy is only one of the screening tests that can be used. This benefit coverage guideline provides general information about how the health plan decides whether a colonoscopy is covered under the preventive or diagnostic (medical) benefits.
What is an incomplete colonoscopy?
Colonoscopy is the most widely used screening modality for the detection and removal of colon polyps and for the prevention of colorectal cancer. Incomplete colonoscopy rates vary from 4% to 25% and are associated with higher rates of interval proximal colon cancer.
What modifier is used for a failed procedure?
Submit CPT modifier 53 with surgical codes or medical diagnostic codes when the procedure is discontinued because of extenuating circumstances. This modifier is used to report services or procedure when the services or procedure is discontinued after anesthesia is administered to the patient.
What is the 52 modifier?
Modifier -52 (reduced services) indicates that a service was partially reduced or eliminated at a physician's discretion, per the CPT Manual. When a physician performs a bilateral procedure on one side only, append modifier -52.
What is a TC modifier?
Modifier TC is used when only the technical component of a procedure is being billed when certain services combine both the professional and technical portions in one procedure code. Use modifier TC when the physician performs the test but does not do the interpretation.
What is modifier 73 used for?
Modifier -73 is used by the facility to indicate that a surgical or diagnostic procedure requiring anesthesia was terminated due to extenuating circumstances or to circumstances that threatened the well being of the patient after the patient had been prepared for the procedure (including procedural pre-medication when
What is the difference between modifier 52 and 53?
By definition, modifier 53 is used to indicate a discontinued procedure and modifier 52 indicates reduced services. In both the cases, a modifier should be appended to the CPT code that represents the basic service performed during a procedure.
What is modifier 50 used for?
CPT Modifier 50 Bilateral Procedures – Professional Claims Only. Modifier 50 is used to report bilateral procedures that are performed during the same operative session by the same physician in either separate operative areas (e.g. hands, feet, legs, arms, ears), or one (same) operative area (e.g. nose, eyes, breasts).
What is the code for colonoscopy?
To report screening colonoscopy on a patient not considered high risk for colorectal cancer, use HCPCS code G0121 and diagnosis code Z12.11 ( encounter for screening for malignant neoplasm of the colon ).
What is a colonoscopy screening?
As such, “screening” describes a colonoscopy that is routinely performed on an asymptomatic person for the purpose of testing for the presence of colorectal cancer or colorectal polyps. Whether a polyp or cancer is ultimately found does not ...
What are the global periods for colonoscopy?
Typically, procedure codes with 0, 10 or 90-day global periods include pre-work, intraoperative work, and post-operative work in the Relative Value Units (RVUs) assigned . As a result, CMS’ policy does not allow for payment of an Evaluation and Management (E/M) service prior to a screening colonoscopy. In 2005, the Medicare carrier in Rhode Island explained the policy this way:
Does Medicare cover colonoscopy?
However, diagnostic colonoscopy is a test performed as a result of an abnormal finding, sign or symptom. Medicare does not waive the co-pay and deductible when the intent of the visit is to perform a diagnostic colonoscopy. Medicare waives the deductible but not the co-pay when a procedure scheduled as a screening is converted to a diagnostic ...
Is E/M covered by Medicare?
Medicare defines an E/M prior to a screening colonoscopy as routine, and thus non-covered. However, when the intent of the visit is a diagnostic colonoscopy an E/M prior to the procedure ordered for a finding, sign or symptom is a covered service.
What does PT mean in CPT?
The PT modifier ( colorectal cancer screening test, converted to diagnostic test or other procedure) is appended to the CPT ® code.
Can you remove polyps at screening colonoscopy?
It is not uncommon to remove one or more polyps at the time of a screening colonoscopy. Because the procedure was initiated as a screening the screening diagnosis is primary and the polyp (s) is secondary. Additionally, the surgeon does not report the screening colonoscopy HCPCS code, but reports the appropriate code for the diagnostic or therapeutic procedure performed, CPT ® code 45379—45392.
What is the ICd 10 code for a mapped ICd 9?
The General Equivalency Mapping (GEM) crosswalk indicates an approximate mapping between the ICD-10 code Z98.890 its ICD-9 equivalent. The approximate mapping means there is not an exact match between the ICD-10 code and the ICD-9 code and the mapped code is not a precise representation of the original code.
What is the code for inpatient admissions to general acute care hospitals?
The code is exempt from present on admission (POA) reporting for inpatient admissions to general acute care hospitals. The code Z98.890 describes a circumstance which influences the patient's health status but not a current illness or injury. The code is unacceptable as a principal diagnosis.
Is Z98.890 a POA?
Z98.890 is exempt from POA reporting - The Present on Admission (POA) indicator is used for diagnosis codes included in claims involving inpatient admissions to general acute care hospitals. POA indicators must be reported to CMS on each claim to facilitate the grouping of diagnoses codes into the proper Diagnostic Related Groups (DRG). CMS publishes a listing of specific diagnosis codes that are exempt from the POA reporting requirement. Review other POA exempt codes here.
Popular Posts:
- 1. icd 10 code for superficial injury left leg
- 2. icd 10 code for running
- 3. icd 10 code for adverse effect of penicillin
- 4. icd 10 code for right arm bacteremia
- 5. icd 10 code for plantar fascial fibromatosis left foot
- 6. icd 10 dx code for atv accident
- 7. icd 1 code for pushed out of vehicle
- 8. icd code 10 for dyspepsia
- 9. icd 10 code for pancreatic cancer
- 10. icd-10 code for ercp with stone removal