What are the unusual ICD-10 codes?
Oct 01, 2021 · Z90.49 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z90.49 became effective on October 1, 2021. This is the American ICD-10-CM version of Z90.49 - other international versions of ICD-10 Z90.49 may differ.
How ICD 10 is different from ICD 9 codes?
Oct 01, 2021 · 2022 ICD-10-CM Diagnosis Code K90.81 Whipple's disease 2016 2017 2018 2019 2020 2021 2022 Billable/Specific Code K90.81 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM K90.81 became effective on October 1, 2021.
What are the new ICD 10 codes?
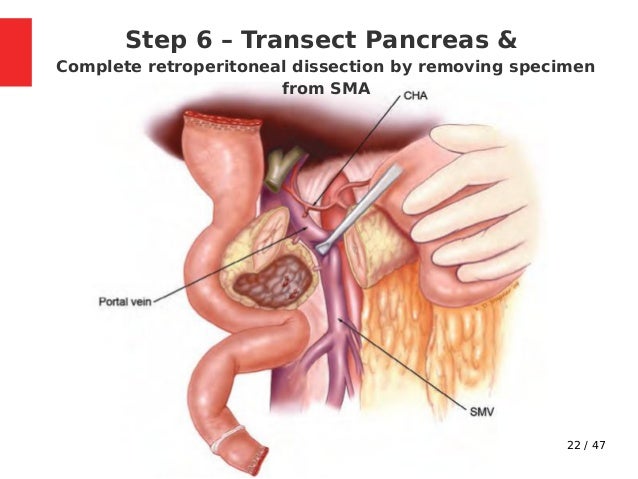
Apr 05, 2022 · AHA Coding Clinic ® for ICD-10-CM and ICD-10-PCS - 2019 Issue 1 Whipple Procedure. The Whipple procedure, also known as a pancreaticoduodenectomy, is a multipart surgery performed as a treatment primarily for people affected by pancreatic cancer. It may also be performed to treat tumors, cysts and other disorders of the pancreas, bile duct and ...
Where can one find ICD 10 diagnosis codes?
Oct 01, 2021 · 2022 ICD-10-CM Diagnosis Code Z98.89 2022 ICD-10-CM Diagnosis Code Z98.89 Other specified postprocedural states 2016 2017 - Converted to Parent Code 2018 2019 2020 2021 2022 Non-Billable/Non-Specific Code Z98.89 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail.

What is the ICD-10 code for status post procedure?
ICD-10-CM Code for Encounter for surgical aftercare following surgery on specified body systems Z48. 81.
What is the ICD-10 code for pancreatectomy?
Valid for SubmissionICD-10:Z90.410Short Description:Acquired total absence of pancreasLong Description:Acquired total absence of pancreas
How do you code status after cholecystectomy?
ICD-10-CM Code for Postcholecystectomy syndrome K91. 5.
What is the ICD-10-CM code for personal history of cholecystectomy?
- cholecystectomy - Z90. 49.
What is the CPT code for Whipple procedure?
Coding Whipple Procedures. Codes 48150 and 48152 describe the standard Whipple procedures, with partial pancreatectomy (subtotal), total removal of the duodenum, partial removal of the stomach, and anastomosis of the bile duct to the intestines and the stomach to the jejunum.Jul 1, 2010
What is a Whipple medical procedure?
The Whipple procedure (pancreaticoduodenectomy) is an operation to remove the head of the pancreas, the first part of the small intestine (duodenum), the gallbladder and the bile duct. The remaining organs are reattached to allow you to digest food normally after surgery.Jun 3, 2020
What is the ICD 10 code for status post Hartmann's procedure?
Valid for SubmissionICD-10:Z93.3Short Description:Colostomy statusLong Description:Colostomy status
What is the ICD 10 code for status post Hemicolectomy?
Z48. 815 - Encounter for surgical aftercare following surgery on the digestive system. ICD-10-CM.
What is the ICD 10 code for status post colon resection?
2022 ICD-10-CM Diagnosis Code Z48. 815: Encounter for surgical aftercare following surgery on the digestive system.
What is the ICD-10-CM code for status post thyroidectomy?
Valid for SubmissionICD-10:Z90.09Short Description:Acquired absence of other part of head and neckLong Description:Acquired absence of other part of head and neck
What is post cholecystectomy?
Post-cholecystectomy syndrome (PCS) is the term used to describe the persistence of biliary colic or right upper quadrant abdominal pain with a variety of gastrointestinal symptoms, which are similar to the features experienced by an individual before cholecystectomy.Feb 15, 2022
What is the ICD-10-CM code for laparoscopic cholecystectomy?
2022 ICD-10-CM Diagnosis Code Z53. 31: Laparoscopic surgical procedure converted to open procedure.
Why does the pancreas no longer make insulin?
In type 1 diabetes, the beta cells of the pancreas no longer make insulin because the body's immune system has attacked them. In type 2 diabetes, the pancreas loses the ability to secrete enough insulin in response to meals.
What is the function of the pancreas?
It produces juices that help break down food and hormones that help control blood sugar levels. Problems with the pancreas can lead to many health problems.
Is Z90.410 a POA?
Z90.410 is exempt from POA reporting - The Present on Admission (POA) indicator is used for diagnosis codes included in claims involving inpatient admissions to general acute care hospitals. POA indicators must be reported to CMS on each claim to facilitate the grouping of diagnoses codes into the proper Diagnostic Related Groups (DRG). CMS publishes a listing of specific diagnosis codes that are exempt from the POA reporting requirement. Review other POA exempt codes here.
What is ZES in medical terms?
Zollinger-Ellison syndrome (ZES) is characterized by severe peptic ulcer disease that results from non-beta islet cell tumors, gastrinomas, of the gastrointestinal tract. The mean age at presentation is 45 to 50 years, and men are affected more often than women.
Can fibrin patch reduce POPF?
Schindl and colleagues (2018) stated that the potential for a fibrin sealant patch to reduce the risk of post-operative pancreatic fistula (POPF) remains uncertain. In a multi-center study, these researchers examined if a fibrin sealant patch is able to reduce POPF in patients undergoing PD with pancreatojejunostomy. Subjects undergoing PD were randomized to receive either a fibrin patch (patch group) or no patch (control group), and stratified by gland texture, pancreatic duct size and neoadjuvant treatment. The primary end-point was POPF; secondary end-points included complications, drain-related factors and LOS. Risk factors for POPF were identified by logistic regression analysis. A total of 142 patients were enrolled; 45 of 71 patients (63 %) in the patch group and 40 of 71 (56 %) in the control group developed biochemical leakage or POPF (p = 0.392). Fistulas were classified as grade B or C in 16 (23 %) and 10 (14 %) patients, respectively (p = 0.277). There were no differences in post-operative complications (54 patients in patch group and 50 in control group; p = 0.839), drain amylase concentration (p = 0.494), time until drain removal (mean (S.D.) 11.6 (1.0) versus 13.3 (1.3) days; p = 0.613), fistula closure (17.6 (2.2) versus 16.5 (2.1) days; p = 0.740) and LOS (22.1 (2.2) versus 18.2 (0.9) days; p = 0.810) between the 2 groups. Multi-variable logistic regression analysis confirmed that obesity (OR 5.28, 95 % CI: 1.20 to 23.18; p = 0.027), soft gland texture (OR 9.86, 95 % CI: 3.41 to 28.54; p < 0.001) and a small duct (OR 5.50, 1.84 to 16.44; p = 0.002) were significant risk factors for POPF. A patch did not reduce the incidence of POPF in patients at higher risk. The authors concluded that the use of a fibrin sealant patch did not reduce the occurrence of POPF and complications after PD with pancreatojejunostomy.
Is MIPD superior to OPD?
However, whether MIPD is superior, equal or inferior to its conventional open pancreatoduodenectomy (OPD) is unclear. These investigators performed a comprehensive review of literature and meta-analysis of MIPD outcomes compared with open surgery. Studies published up to May 2017 were searched in PubMed, Embase, Cochrane Library, and Web of Science. Main outcomes were comprehensively reviewed and measured including conversion to open approach, operation time (OP), estimated blood loss (EBL), transfusion, length of hospital stay (LOS), overall complications, post-operative pancreatic fistula (POPF), delayed gastric emptying (DGE), post-pancreatectomy hemorrhage (PPH), re-admission, re-operation and reasons of pre-operative death, number of retrieved lymph nodes (RLN), surgical margins, recurrence, and survival. The software of Review Manage version 5.1 was used for meta-analysis. A total of 100 studies were included for systematic review and 26 (a total of 3,402 cases, 1,064 for MIPD, 2,338 for OPD) were included for meta-analysis. In the early years, most articles were case reports or non-control case series studies, while in the last 6 years high-volume and comparative researches were increasing gradually. Systematic review revealed conversion rates of MIPD to OPD ranged from 0 % to 40 %. The mean or median OP of MIPD ranged from 276 to 657 mins. The total POPF rates vary between 3.8 % and 50 % observed in all systematic reviewed studies. Meta-analysis demonstrated MIPD had longer OP (weighted mean difference [WMD] = 99.4 mins; 95 % CI: 46.0 to 152.8, p < 0.01), lower blood loss (WMD = -0.54 ml; 95 % CI: -0.88 to -0.20 ml; p < 0.01), lower transfusion rate (RR = 0.73, 95 % CI: 0.57 to 0.94, p = 0.02), shorter LOS (WMD = -3.49 days; 95 %CI: -4.83 to -2.15, p < 0.01). There was no significant difference in time to oral intake, post-operative complications, POPF, re-operation, re-admission, peri-operative mortality and number of retrieved lymph nodes. The authors concluded that the findings of this study demonstrated that MIPD was technically feasible and safe on the basis of historical studies; MIPD was associated with less blood loss, faster post-operative recovery, shorter length of hospitalization and longer operation time. Moreover, they stated that these findings need to be confirmed with robust prospective comparative studies and randomized clinical trials.
Popular Posts:
- 1. icd 10 code for periodic preventive exam
- 2. icd 10 code for elevated albumin globulin ratio
- 3. icd 10 code for right shoulder lipoma
- 4. icd 10 code for cervical cord syrinx
- 5. icd 10 code for osteoporosis of forarm
- 6. icd 10 code for screening std
- 7. 2017 icd 10 code for gestational diabetes
- 8. icd 10 code for nicm ef 20-25%
- 9. icd 10 cm code for mrsa sepsis
- 10. 2016 icd 10 code for chest pain.