Full Answer
What is the ICD 10 code for no diagnosis?
Person with feared health complaint in whom no diagnosis is made. Z71.1 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
How do you code a diagnosis that is suspected?
Do not code diagnoses documented as “probable”, “suspected,” “questionable,” “rule out,” or “working diagnosis” or other similar terms indicating uncertainty. Rather, code the condition (s) to the highest degree of certainty for that encounter/visit, such as symptoms, signs, abnormal test results, or other reason for the visit.
Do Doctors follow ICD-10 coding rules for abnormal sign/symptom?
Neither the primary care physician nor the surgeon followed ICD-10 coding rules and coded the abnormal sign/symptom. Instead, they coded the suspected diagnosis.
Which ICD 10 code should not be used for reimbursement purposes?
Z03.82 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail. The 2022 edition of ICD-10-CM Z03.82 became effective on October 1, 2021.
What is a Z00-Z99?
Categories Z00-Z99 are provided for occasions when circumstances other than a disease, injury or external cause classifiable to categories A00 -Y89 are recorded as 'diagnoses' or 'problems'. This can arise in two main ways:
What does "type 1 excludes" mean?
A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition.
What is the code for primary malignancy?
When a primary malignancy has been previously excised or eradicated from its site and there is no further treatment directed to that site and there is no evidence of any existing primary malignancy, a code from category Z85, Personal history of malignant neoplasm, should be used to indicate the former site of the malignancy .
When to use a malignant neoplasm code?
Use a malignant neoplasm code if the patient has evidence of the disease, primary or secondary, or if the patient is still receiving treatment for the disease. If neither of those is true, then report personal history of malignant neoplasm.
What is an uncertain diagnosis?
Uncertain diagnosis. Do not code diagnoses documented as “probable”, “suspected,” “questionable,” “rule out,” or “working diagnosis” or other similar terms indicating uncertainty. Rather, code the condition (s) to the highest degree of certainty for that encounter/visit, such as symptoms, signs, abnormal test results, or other reason for the visit. ...
What is the code for alleged child rape?
If the suspected case is an alleged rape or sexual abuse that is ruled out, Z04.42 (encounter for examination and observation following alleged child rape) should be used. Again, the code from category T76 would not be reported.
What is Y07 code?
A perpetrator code (Y07) is reported when the person who performed the abuse/neglect is known. For suspected but not confirmed cases, the perpetrator is not reported. The code identifies the relationship between the perpetrator and the victim.
What is encounter for examination?
This category is to be used when a person without a diagnosis is suspected of having an abnormal condition, without signs or symptoms, which requires study, but after examination and observation, is ruled-out.
What does "type 1 excludes" mean?
It means "not coded here". A type 1 excludes note indicates that the code excluded should never be used at the same time as Z04.71. A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition.
What happens if diagnostic testing confirms a diagnosis?
If diagnostic testing confirms a diagnosis, report the definitive diagnosis rather than the signs and symptoms that prompted the test. If the definitive diagnosis fails to present a complete picture of the patient’s condition, you may assign additional signs and symptoms codes.
Why is it important to coding uncertain diagnoses?
Coding Uncertain Diagnoses. Accurate diagnosis coding is crucial for patient care and compliant, optimal reimbursement. In the outpatient setting, you should never assign a diagnosis unless that diagnosis has been confirmed by diagnostic testing, or is otherwise certain. Uncertain diagnoses include those that are:
What is an uncertain diagnosis?
Uncertain diagnoses include those that are: If you are unable to determine a definitive diagnosis, you should document and code for the signs, symptoms, abnormal test result (s), or other conditions that prompted the patient encounter.
Is HIV an exception?
HIV Is an Exception. HIV is an exception to the above rule: HIV is the only condition that must be confirmed if it is to be reported in the in-patient setting. Confirmation does not require documentation of positive serology or culture for HIV.
What is an uncertain diagnosis?
A: Uncertain diagnoses are those that at the time of discharge are still being documented as “probable,” “suspected,” “likely,” “questionable,” “possible,” “still to be ruled out,” or other similar terminology. At the time of discharge means that the condition in question upon admission must still be thought to be a diagnosis in question ...
Why should a coder query the physician?
In this case, the coder should query the physician to clarify that the diagnosis of pneumonia was ruled out . The coder should not assume that the condition was ruled out because it is not listed in the final diagnoses.
What is the code for avian influenza?
Avian influenza, novel influenza or other identified influenza-“ suspected”, “possible”, or “probable” avian influenza, novel influenza, or other identified influenza would be coded to category J11 , “Influenza due to unidentified influenza virus.”. The above guidance is for inpatient cases only.
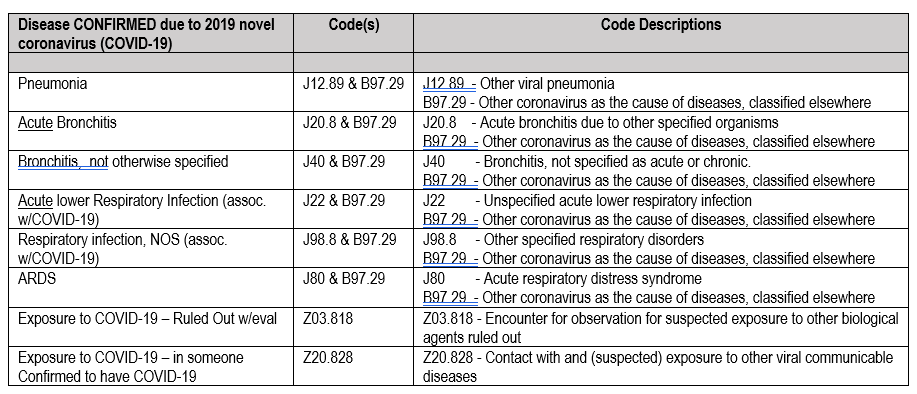
Can you code a Zika virus?
A: Yes , there are a few exceptions for specific diagnoses/areas of coding. Such as: Zika virus- if the documentation in the record is “suspected,” “possible” or “probable” Zika then only the symptoms or contact with codes (Z20.828) would be coded. Only confirmed cases of Zika virus are coded.
Popular Posts:
- 1. icd 10 code for calcific constrictive pericarditis
- 2. icd 10 cm code for ski sensatrion
- 3. icd 10 code for chronic inflammation and fibrosis
- 4. 2015 icd 10 code for small bowel dilatation
- 5. icd 10 code for muscle spasms unspecified
- 6. icd-10-cm code for history mastectomy
- 7. icd 10 code for cholesteatoma
- 8. icd 10 code for left below knee amputation wound
- 9. icd 9 code for medial epicondylitis
- 10. icd 10 code for ac joint separation