Can you ever use an unspecified ICD-10 code?
In both ICD-9 and ICD-10, signs/symptoms and unspecified codes are acceptable and may even be necessary. In some cases, there may not be enough information to describe the patient's condition or no other code is available to use. Although you should report specific diagnosis codes when they are supported by the available documentation and clinical knowledge of the patient's health condition, in some cases, signs/symptoms or unspecified codes are the best choice to accurately reflect the ...
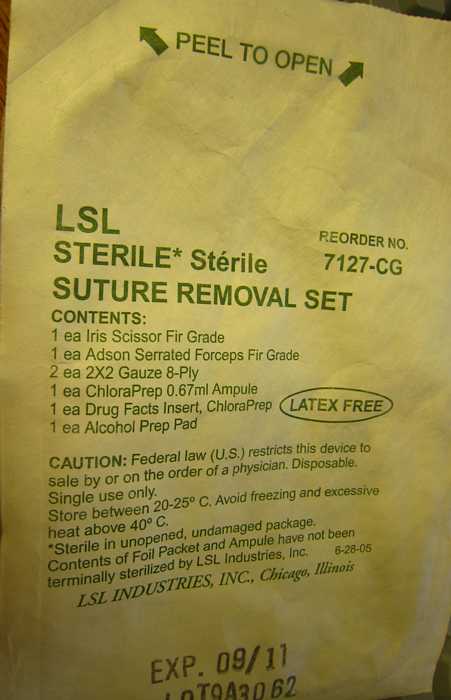
What is the procedure code for suture removal?
Tips for coding suture removal:
- Suture removal using general anaesthesia is very rare; hence coder has to verify medical record thoroughly before using CPTs 15850 and 15851
- Avoid typo error when using CPT 99024. This can get easily mistaken with CPT 99204 which is EM visit level code.
- When the suture removal is performed within the global period, it is bundled with the surgery code.
What ICD 10 cm code(s) are reported?
What is ICD-10-CM, ICD-10-PCS, CPT, and HCPCS?
- ICD-10-CM, ICD-10-PCS, CPT, and HCPCS. If you are new to medical coding, you may not know what these acronyms mean. ...
- Acronyms
- Code Sets and Their Definitions. The following are the definitions for each code set. CMS maintains this code set, except for dental services (D codes).
What is ICD 10 code for?
What is ICD-10. The ICD tenth revision (ICD-10) is a code system that contains codes for diseases, signs and symptoms, abnormal findings, circumstances and external causes of diseases or injury. The need for ICD-10. Created in 1992, ICD-10 code system is the successor of the previous version (ICD-9) and addresses several concerns.
What is the ICD-10 code for surgical aftercare?
81 for Encounter for surgical aftercare following surgery on specified body systems is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is the code Z76 89 for?
Persons encountering health services in other specified circumstancesZ76. 89 is a valid ICD-10-CM diagnosis code meaning 'Persons encountering health services in other specified circumstances'. It is also suitable for: Persons encountering health services NOS.
What is the ICD-10 code for wound care?
This article addresses the CPT/HCPCS and ICD-10 codes associated with L37228 Wound Care policy.
Can Z48 02 be a primary code?
The patient's primary diagnostic code is the most important. Assuming the patient's primary diagnostic code is Z48. 02, look in the list below to see which MDC's "Assignment of Diagnosis Codes" is first. That is the MDC that the patient will be grouped into.
Is Z76 89 a billable code?
Z76. 89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is a diagnostic code Z76 9?
ICD-10 code: Z76. 9 Person encountering health services in unspecified circumstances.
What is the ICD 10 code for surgical wound?
ICD-10 Code for Disruption of external operation (surgical) wound, not elsewhere classified, initial encounter- T81. 31XA- Codify by AAPC.
What is the ICD 10 code for non-healing surgical wound?
998.83 - Non-healing surgical wound | ICD-10-CM.
What is the ICD 10 code for surgical wound dehiscence?
T81. 31 - Disruption of external operation (surgical) wound, not elsewhere classified. ICD-10-CM.
What is the ICD-10 code for stitches?
Encounter for attention to dressings, sutures and drains ICD-10-CM Z48.
Is suture removal separately billable?
Suture Removal Is Rarely Reported Separately - AAPC Knowledge Center. HEALTHCON Regional 2022 | Stay Current. Stay Engaged. | Join today!
What is the ICD-10 code for retained suture?
Other mechanical complication of permanent sutures, initial encounter. T85. 692A is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM T85.
What is the ICD-10 code for annual physical exam?
Z00.00ICD-10 Code for Encounter for general adult medical examination without abnormal findings- Z00. 00- Codify by AAPC.
What is the ICD-10 code for new patient establishing care?
Code the initial visit as a new visit, and subsequent treatment visits as established with the E/M code 99211.
What is the ICD-10 code for lab review?
ICD-10 Code for Person consulting for explanation of examination or test findings- Z71. 2- Codify by AAPC.
What is the ICD-10 code for referral to specialist?
Encounter for other administrative examinations The 2022 edition of ICD-10-CM Z02. 89 became effective on October 1, 2021. This is the American ICD-10-CM version of Z02.
What is the CPT repair code for wound closure?
Each of these variables is specified in the CPT® repair codes. The repair can consist of sutures, staples, or tissue adhesive (for example, Dermabond), either singly or in combination with each other, or with adhesive strips. Wound closure using adhesive strips as the only repair material should be reported using the appropriate evaluation and management (E/M) code. Wounds repaired solely with Dermabond or other tissue adhesive are reported to Medicare with HCPCS Level II code G0168 Wound closure utilizing tissue adhesive (s) only. Commercial carriers allow simple repair codes (12001-12018). Let’s examine the three key elements that are crucial in determining the correct wound repair code.
What is a simple repair?
Simple repairs (12001-12021) are for superficial wounds with partial- or full-thickness damage to the skin (epidermis/dermis) and possibly the subcutaneous tissue. Deeper structures are not involved, and these repairs require only a simple one-layer closure. These straightforward repairs involve the skin; deeper layers, such as muscle, remain unaffected. Anesthesia and chemical or electrocauterization of wounds are included.
What is the final code selection?
Final code selection is based on the size of the repair. The length of the wound repaired must be measured and recorded in centimeters, whether curved, angular, or stellate. If the wound measurements are documented in inches or millimeters, instead of centimeters, convert the measurements to centimeters before selecting the appropriate code.
What is intermediate repair?
Intermediate repairs (12031-12057) involve a layered closure of one or more of the deeper layers of the subcutis and superficial (non-muscle) fascia, in addition to the skin (epidermal and dermal) closure. Wounds necessitating an intermediate repair are generally deeper or gaping, requiring suture placement inside the wound to approximate tissue layers below the skin. Per CPT®, “Single-layer closure of heavily contaminated wounds that have required extensive cleaning or removal of particulate matter also constitutes intermediate repair.” When searching the documentation for clues regarding complexity, statements such as “layered closure,” “extensive cleaning,” and/or “removal of debris” indicate an intermediate repair. Lack of these details or mention of a “single-layer closure” suggests a simple repair.
How to avoid coding mistakes?
Avoid common coding mistakes by remembering the three key components for coding wound repair correctly: complexity, location, and length. Detailed documentation is critical in determining these details, which ensures coding precision and proper payment for services rendered.
Can wound repair be reported separately?
Wound repair is often performed with other related procedures. Some of these related procedures can be separately reported, while others can’t or depend on specific circumstances. Here’s a breakdown of how to determine when separate reporting is warranted.#N#Never reported separately with wound repair:
Can a wound be repaired in a single session?
Often, the physician repairs several wounds in a single session. When multiple wounds are repaired, check if any repairs of the same classification (simple, intermediate, complex) are grouped to the same anatomic area. If so, per CPT® coding guidelines, the lengths of the wounds repaired should be added together and reported with a single, cumulative code. Do NOT combine wounds of different complexity or those that fall within separate anatomical location groupings.#N#When reporting wounds of differing severity and/or location, claim the most extensive code as the primary service and append modifier 59 Distinct procedural service to subsequent repair codes. Multiple procedure reductions will apply for the second and subsequent procedures, except for those reported using an add-on code.
How to ensure accurate coding for laceration repairs?
Experienced medical billing and coding service providers will ensure accurate coding for laceration repairs by considering the complexity, location and subcategory, size, and whether multiple repairs were performed. Comprehensive physician documentation is vital to determine the complexity and size of the repair (s). As there is a considerable difference between the payment for the various repair types, lack of proper documentation can affect coding precision and the provider’s reimbursement.
What is complex repair code?
A complex repair code is used to bill the most complicated surgical repair that a physician will perform on the integumentary system, though complex repair excludes the excision of benign or malignant lesions. Complex repair is billed when the physician performs more than layered closure. Additionally, if a benign lesion was removed before the wound repair procedure, a minimum of two surgical codes can be billed: one for the removal and one for the repair.
What is medical coding outsourcing?
Medical coding outsourcing is a practical option to negotiate the maze of laceration repair codes and guidelines.
Is suture removal reported separately?
The American Medical Association provides the following guidance on suture removal: Removal of sutures by the physician who originally placed them is not separately reportable since the removal is included in the initial laceration repair code.
Can a suture removal be charged?
If a provider has placed sutures for a patient and the patient returns to the same provider for the suture removal, then the visit for the suture removal cannot be charged, because the removal is included in the initial laceration repair code.
Is layered closure an intermediate repair?
A layered closure constitutes an intermediate repair and the intermediate repair code should be billed even if the physician does not specifically use the word “intermediate” in the documentation.
Can you code multiple lacerations?
You can code for all of them. When the patient has multiple lacerations of the same repair complexity on the same body part, coding is easy: You simply add the lengths of each wound together and choose the matching code.
Popular Posts:
- 1. 2018 icd 10 code for frequent falls
- 2. icd 10 code for hyperemesis
- 3. icd 10 code for aquired torsion dystonia
- 4. icd 9 code for on chemotherapy
- 5. icd 10 code for dm with ckd 4
- 6. icd 10 code for long term use of carvedilol
- 7. icd 10 code for la grade b esophagiis
- 8. icd 10 code for pathological fractures due to b cell lymphoma
- 9. icd-10 code for prp injection
- 10. icd 9 code for peroneal tendonitis