What is the ICD 10 code for lumbar synovial cyst?
500 results found. Showing 1-25: ICD-10-CM Diagnosis Code G96.191 [convert to ICD-9-CM] Perineural cyst. Cervical nerve root cyst; Lumbar nerve root cyst; Sacral nerve root cyst; Tarlov cyst; Thoracic nerve root cyst. ICD-10-CM Diagnosis Code G96.191. Perineural cyst. 2021 - New Code 2022 Billable/Specific Code.
What is a Tarlov cyst?
Oct 01, 2021 · 2021 - New Code 2022 Billable/Specific Code. G96.191 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM G96.191 became effective on October 1, 2021. This is the American ICD-10-CM version of G96.191 - other international versions of ICD-10 G96.191 may differ.
What is the ICD 10 code for thoracic nerve root cyst?
Oct 01, 2021 · M71.38 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM M71.38 became effective on October 1, 2021. This is the American ICD-10-CM version of M71.38 - other international versions of ICD-10 M71.38 may differ.
What is the ICD 10 code for lumbar puncture?
Oct 01, 2021 · G96.19 should not be used for reimbursement purposes as there are multiple codes below it that contain a greater level of detail. The 2022 edition of ICD-10-CM G96.19 became effective on October 1, 2021. This is the American ICD-10-CM version of G96.19 - other international versions of ICD-10 G96.19 may differ.
What is the ICD-10 code for Tarlov cyst?
What is Tarlov cyst?
What is the ICD-10 code for synovial cyst of lumbar facet joint?
What is another name for Tarlov cyst?
How are Tarlov cysts diagnosed?
What is a cyst at the base of the spine called?
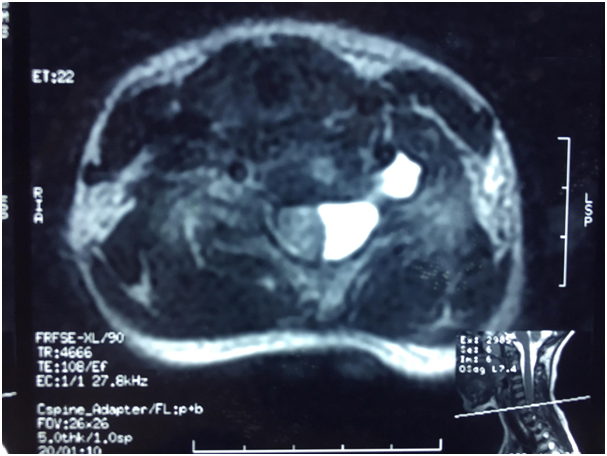
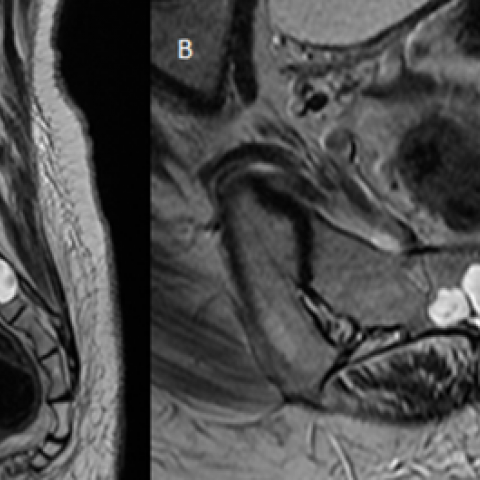
Tarlov cysts are fluid-filled nerve root cysts found most commonly at the sacral level of the spine – the vertebrae at the base of the spine. These cysts typically occur along the posterior nerve roots. Cysts can be valved or nonvalved.
What is the ICD-10 code for spinal cyst?
What is a lumbar facet cyst?
What is the ICD-10 code for synovial cysts?
Is Tarlov cyst a disability?
What is a subarachnoid cyst?
What is considered a large Tarlov cyst?
When will the ICD-10 G96.191 be released?
The 2022 edition of ICD-10-CM G96.191 became effective on October 1, 2021.
What is the A00-B99?
certain conditions originating in the perinatal period ( P04 - P96) certain infectious and parasitic diseases ( A00-B99) complications of pregnancy, childbirth and the puerperium ( O00-O9A)
Where are Tarlov cysts found?
TARLOV CYSTS-. perineurial cysts commonly found in the sacral region. they arise from the perineurium membrane within the spinal nerve roots. the distinctive feature of the cysts is the presence of spinal nerve root fibers within the cyst wall or the cyst cavity itself.
When is the ICd 10 code for G96.191?
G96.191 is new to ICD-10 code set for the FY 2021, effective October 1, 2020. The National Center for Health Statistics (NCHS) has published an update to the ICD-10-CM diagnosis codes which became effective October 1, 2020. This is a new and revised code for the FY 2021 (October 1, 2020 - September 30, 2021).
What is the G96.191 code?
G96.191 is a billable diagnosis code used to specify a medical diagnosis of perineural cyst. The code G96.191 is valid during the fiscal year 2021 from October 01, 2020 through September 30, 2021 for the submission of HIPAA-covered transactions.
What is a Tarlov cyst?
Seo and colleagues (2014) noted that Tarlov cysts (TCs – also known as perineurial cysts and sacral meningeal cysts) are lesions of the nerve root that are often observed in the sacral area . There is debate regarding whether symptomatic TCs should be treated surgically. These researchers presented the findings of 3 patients with symptomatic TCs who were treated surgically, and introduced sacral re-capping laminectomy. Patients complained of low back pain (LBP) and hypesthesia on lower extremities (LEs). These investigators operated with sacral re-capping technique for all 3 patients. The outcome measure was baseline visual analog scale (VAS) score and post-operative follow-up magnetic resonance images (MRIs). All patients were completely relieved of symptoms following operation. The authors concluded that although not sufficient to address controversies, the findings of this small case series introduced successful use of a particular surgical technique to treat sacral TC, with resolution of most symptoms and no sequelae.
What is lumbar spinal stenosis?
Pietrantonio and colleagues (2019) noted that lumbar spinal stenosis (LSS) is the most common spinal disease in the geriatric population , and is characterized by a compression of the lumbo-sacral neural roots from a narrowing of the lumbar spinal canal. LSS can result in symptomatic compression of the neural elements, requiring surgical treatment if conservative management fails. Different surgical techniques with or without fusion are current therapeutic options. These investigators reported the long-term clinical outcomes of patients who underwent bilateral laminotomy compared with total laminectomy for LSS. They retrospectively reviewed all the patients treated surgically by the senior author for LSS with total laminectomy and bilateral laminotomy with a minimum of 10 years of follow-up. Patients were divided into 2 treatment groups (total laminectomy, group 1; and bilateral laminotomy, group 2) according to the type of surgical decompression. Clinical outcomes measures included the VAS, the 36-Item Short-Form Health Survey (SF-36) scores, and the ODI. In addition, surgical parameters, re-operation rate, and complications were evaluated in both groups. A total of 214 patients met the inclusion and exclusion criteria (105 and 109 patients in groups 1 and 2, respectively). The mean age at surgery was 69.5 years (range of 58 to 77). Comparing pre- and post-operative values, both groups showed improvement in ODI and SF-36 scores; at final follow-up, a slightly better improvement was noted in the laminotomy group (mean ODI value of22.8, mean SF-36 value of 70.2), considering the worse pre-operative scores in this group (mean ODI value of 70, mean SF-36 value of 38.4) with respect to the laminectomy group (mean ODI of 68.7 versus mean SF-36 value of 36.3), but there were no statistically significant differences between the 2 groups. Significantly, in group 2 there was a lower incidence of re-operations (15.2 % versus 3.7 %, p = 0.0075). The authors concluded that bilateral laminotomy allowed adequate and safe decompression of the spinal canal in patients with LSS; this technique ensured a significant improvement in patients' symptoms, disability, and QOL. Clinical outcomes were similar in both groups, but a lower incidence of complications and iatrogenic instability has been shown in the long-term in the bilateral laminotomy group.
What is laminoplasty for cervical stenosis?
Laminoplasty (laminaplasty) may be indicated in patients with myelopathy and multiple-level cervical spondylosis, such as in congenital cervical stenosis. When cervical spinal stenosis is severe, various symptoms may develop which include pain, weakness in arms and/or legs and unsteadiness in the gait (myelopathy).
Can you use a maxilla fixation plate for laminoplasty?
Humadi and associates (2017) noted that in the late 1990s, spinal surgeons experimented by using maxilla-facial fixation plates as an alternative to sutures, anchors, and local spinous process autografts to provide a more rigid and lasting fixation for laminoplasty. This eventually led to the advent of laminoplasty mini-plates, which are currently used. In a systematic review and meta-analysis, these investigators compared laminoplasty techniques with plate and without plate with regard to functional outcome results. Qualitative and quantitative analyses were performed to evaluate the currently available studies in an attempt to justify the use of a plate in laminoplasty. The principal finding of this study was that there was no statistically significant difference in clinical outcome between the 2 different techniques of laminoplasty. The authors concluded that there is insufficient evidence in the literature to support one technique over the other, and hence, there is no evidence to support change in practice (using or not using the plate in laminoplasty); a RCT will give a better comparison between the 2 groups.
Does Aetna require vertebral corpectomy?
Aetna considers vertebral corpectomy (removal of half. Footnotes. * or more of vertebral body, not mere removal of osteophytes and minor decompression ) medically necessary in the treatment of one of the following: For tumors involving one or more vertebrae, or. Greater than 50 % compression fracture of vertebrae, or.
Is lumbar fusion a degenerative indication?
Yavin and colleagues (2017) noted that due to uncertain evidence, lumbar fusion for degenerative indications is associated with the greatest measured practice variation of any surgical procedure. These investigators summarized the current evidence on the comparative safety and efficacy of lumbar fusion, decompression-alone, or non-operative care for degenerative indications. They carried out a systematic review using PubMed, Medline, Embase, and the Cochrane Central Register of Controlled Trials (up to June 30, 2016). Comparative studies reporting validated measures of safety or efficacy were included. Treatment effects were calculated through DerSimonian and Laird random effects models. The literature search yielded 65 studies (19 RCTs, 16 prospective cohort studies, 15 retrospective cohort studies, and 15 registries) enrolling a total of 302,620 patients. Disability, pain, and patient satisfaction following fusion, decompression-alone, or non-operative care were dependent on surgical indications and study methodology. Relative to decompression-alone, the risk of re-operation following fusion was increased for spinal stenosis (relative risk [RR] 1.17, 95 % CI: 1.06 to 1.28) and decreased for spondylolisthesis (RR 0.75, 95 % CI: 0.68 to 0.83). Among patients with spinal stenosis, complications were more frequent following fusion (RR 1.87, 95 % CI: 1.18 to 2.96). Mortality was not significantly associated with any treatment modality. The authors concluded that positive clinical change was greatest in patients undergoing fusion for spondylolisthesis while complications and the risk of re-operation limited the benefit of fusion for spinal stenosis. The relative safety and efficacy of fusion for chronic LBP suggested careful patient selection is needed.
Is laminoplasty effective for cervical kyphosis?
Qian and colleagues (2018) noted that the efficacy of laminoplasty in patients with cervical kyphosis is controversial. These investigators examined the impact of the initial pathogenesis on the clinical outcomes of laminoplasty in patients with cervical kyphosis. A total of 137 patients with CSM or OPLL underwent laminoplast y from April 2013 to May 2015. Subjects were divided into the following 4 groups: lordosis with CSM (LC), kyphosis with CSM (KC), lordosis with OPLL (LO), and kyphosis with OPLL (KO). The clinical outcome measures included the VAS and mJOA scores, ROM, and the cervical global angle (CGA). The mean VAS and mJOA scores improved significantly in all groups after surgery. The changes in VAS and mJOA scores were significantly smaller, and the JOA recovery rate was significantly lower, in the KC group than in the LC and KO groups. The mean change in the CGA was greatest in the KC group (greater than 8° towards kyphosis). The pre-operative ROM was negatively correlated with the change in CGA and the JOA recovery rate in the KO and KC groups. The authors concluded that laminoplasty is suitable for patients with cervical lordosis and those with mild cervical kyphosis and OPLL, but is not recommended for patients with kyphosis and CSM, particularly those with a large ROM pre-operatively. This study had several drawbacks. First, it was a retrospective study. Second, it was limited to a single institution. Third, a relatively small number of patients were involved, and the follow-up duration was short. These researchers plan to conduct a further study involving a larger number of patients and a longer follow-up.
Popular Posts:
- 1. icd 10 code for right diabetic foot ulcer with osteomyelitis
- 2. icd 10 code for e952.0
- 3. icd 10 code for loose toenail
- 4. icd 10 code for heavy fever
- 5. icd-10 code for thoracic outlet syndrome
- 6. icd 10 code for diabetic macular edema left eye
- 7. icd 10 code for fx right proximal 5th metacarpal
- 8. icd 10 code for abnormal potassium level
- 9. icd 10 code for acute situational anxiety
- 10. icd-10 code for stomalgia