| Aetna | Cigna | |
|---|---|---|
| Modifier | Commercial: -GT or -95 Medicare Advantage: -95 | -GQ, -GT, or -95 (all three accepted) -CS *Must use appropriate ICD-10 code (Z03.818 or Z20.828 |
| Cost-share waiver | Yes | Yes |
| Covers cost-share | Yes | Yes |
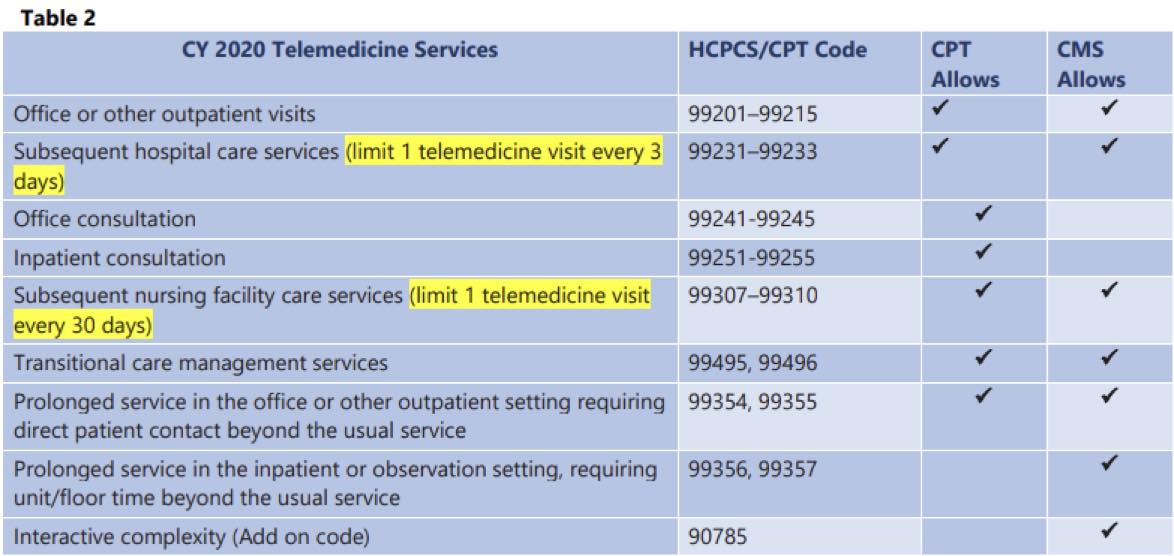
What is the CPT code for telemedicine?
Apr 29, 2020 · Code 99201-99215 – This is a 15-20 minutes’ outpatient office visit for either new or already established patients. The GT Modifier helps in keeping a track and lets them know that the visit has taken place virtually on this telemedicine platform. This in turns helps in keeping and maintaining a record.
How should telehealth visits be coded?
Apr 28, 2020 · (8 days ago) Most common ICD 10 Codes for Telemedicine Service Providers. Health (7 days ago) E&M Code and GT Modifier: Code 99201-99215 – This is a 15-20 minutes’ outpatient office visit for either new or already established patients.
Does Medicare require audio-video for telehealth visits?
Most common ICD 10 Codes for Telemedicine Service Providers (7 days ago) E&M Code and GT Modifier: Code 99201-99215 – This is a 15-20 minutes’ outpatient office visit for either new or already established patients. The GT Modifier helps in keeping a track and lets them know that the visit has taken place virtually on this telemedicine platform.
Can I Bill for Telehealth/telemedicine services outside the global period?
Apr 13, 2020 · Also, some Medicare-aged patients are resisting and/or refusing the video chat option. This means that the visit is now telemedicine, not telehealth, and a phone call code, 99441-99443, is the only option between your physician and/or QHP. The visit would need to be timed and still include consent, to report a phone call.
When will CMS update telehealth?
Original story posted on: April 13, 2020. As CMS continues to update their policies on telehealth during the COVID-19 pandemic and the Public Health Emergency, ICD10monitor is here to continue to keep you informed on these changes.
Who is Terry Fletcher?
Terry Fletcher, BS, CPC, CCC, CEMC, CCS, CCS-P, CMC, CMSCS, CMCS, ACS-CA, SCP-CA, QMGC, QMCRC, is a healthcare coding consultant, educator, and auditor with more than 30 years of experience. Terry is a past member of the national advisory board for AAPC, past chair of the AAPCCA, and an AAPC national and regional conference educator. Terry is the author of several coding and reimbursement publications, as well as a practice auditor for multiple specialty practices around the country. Her coding and reimbursement specialties include cardiology, peripheral cardiology, gastroenterology, E&M auditing, orthopedics, general surgery, neurology, interventional radiology, and telehealth/telemedicine. Terry is a member of the ICD10monitor editorial board and a popular panelist on Talk Ten Tuesdays.
How often should I use ICd 10 code Z13.89?
Clinicians should use the ICD-10 code Z13. 89 when billing for telehealth CPT code 96127. Generally, it can be used up to four times a year with four units per visit. However, each insurance company establishes its own limits, so it’s best to check with the individual insurance payer for their rules.
What is the CPT code for psychotherapy?
CPT codes 90839 and 90840 can be used for psychotherapy provided in crisis sessions. While 90839 covers a 60-minute session, 90840 is used as an add-on code for each additional 30 minutes. Both codes need to be listed on the billing form.
What is CPT code 99091?
CPT code 99091 can be billed when using remote patient monitoring (RPM) with clients via telehealth. RPM refers to a range of technologies used to monitor clients’ behaviors or bodily processes outside of the clinician’s office. RPM has many potential benefits, including: 1 improving convenience and access to healthcare for the client 2 improving healthcare efficiency 3 having clients take an active role in the own healthcare 4 helping clinicians to detect problems earlier
Do insurance companies require prior authorization for telehealth?
Some insurance companies do not require prior authorization or medical records to support the need for some of these additional telehealth services because they are meant to be a generic screening tool applied to a large patient population to identify mental health issues. However, it’s best to check with the individual insurance companies about their requirements before billing for this service to be safe.

Popular Posts:
- 1. icd 10 code for osteomyelitis foot unspecified
- 2. icd 9 code for ivc filter
- 3. icd 10 code for rapid afib
- 4. icd 10 code for comfort care measures
- 5. icd 10 code for acute frontal sinusitis
- 6. icd 10 data code for personal history of colon cancer
- 7. icd 9 code for screening for the tanner
- 8. icd 10 code for tetralogy of fallot:
- 9. icd 10 code for aortic occlusion
- 10. icd 10 code for gastric bypass restriction loss