Chronic kidney disease, unspecified
- N18.9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2022 edition of ICD-10-CM N18.9 became effective on October 1, 2021.
- This is the American ICD-10-CM version of N18.9 - other international versions of ICD-10 N18.9 may differ.
What is the ICD 10 code for unspecified kidney failure?
Unspecified kidney failure 1 N19 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. 2 The 2021 edition of ICD-10-CM N19 became effective on October 1, 2020. 3 This is the American ICD-10-CM version of N19 - other international versions of ICD-10 N19 may differ.
What is the latest version of the ICD 10 for kidney transplant?
Kidney transplant failure. The 2019 edition of ICD-10-CM T86.12 became effective on October 1, 2018. This is the American ICD-10-CM version of T86.12 - other international versions of ICD-10 T86.12 may differ.
What is the ICD 10 code for end stage renal disease?
End stage renal disease. N18.6 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2020 edition of ICD-10-CM N18.6 became effective on October 1, 2019. This is the American ICD-10-CM version of N18.6 - other international versions of ICD-10 N18.6 may differ.
What is the CPT code for chronic kidney disease?
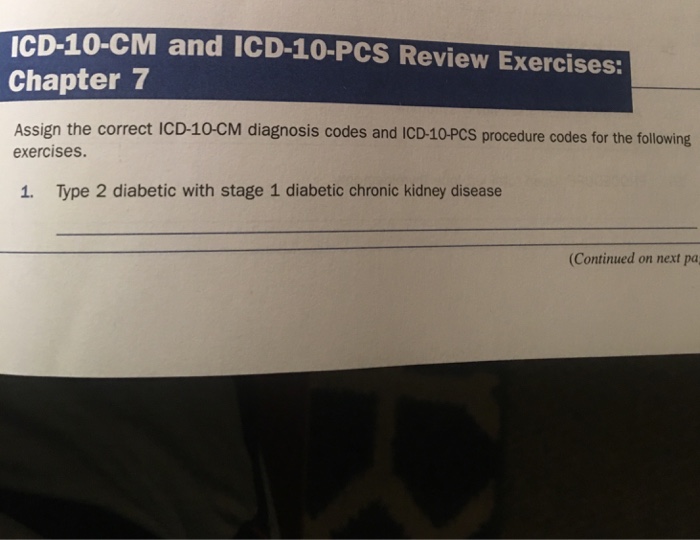
Code First any associated: diabetic chronic kidney disease (E08.22, E09.22, E10.22, E11.22, E13.22) hypertensive chronic kidney disease (I12.-, I13.-) Use Additional code to identify kidney transplant status, if applicable, (Z94.0) Chronic kidney disease (CKD)
What is transient acute renal failure?
“Transient AKI” was defined as a return to baseline SCr within 3 days post-AKI and “Persistent AKI” was defined as renal dysfunction without recovery within 3 days.
What is unspecified renal failure?
A condition in which the kidneys stop working and are not able to remove waste and extra water from the blood or keep body chemicals in balance. Acute or severe renal failure happens suddenly (for example, after an injury) and may be treated and cured.
What is the ICD-10 diagnosis code for AKI?
Acute kidney failure, unspecified.
What is the ICD-10 code for worsening renal function?
Abnormal results of kidney function studies The 2022 edition of ICD-10-CM R94. 4 became effective on October 1, 2021.
What are the 3 types of acute renal failure?
Acute renal failure (ARF) can be divided into three main types: perennial, renal, and postrenal.
What is the diagnosis code for renal failure?
ICD-10-CM code N28. 9 is reported to capture the acute renal insufficiency. Based on your documentation, acute kidney injury/failure (N17.
How do I code acute on chronic renal failure?
The ICD-10 code range for Acute kidney failure and chronic kidney disease N17-N19 is medical classification list by the World Health Organization (WHO).
What is I10 diagnosis?
ICD-Code I10 is a billable ICD-10 code used for healthcare diagnosis reimbursement of Essential (Primary) Hypertension.
Is acute kidney injury the same as kidney failure?
Acute kidney injury (AKI), also known as acute renal failure (ARF), is a sudden episode of kidney failure or kidney damage that happens within a few hours or a few days. AKI causes a build-up of waste products in your blood and makes it hard for your kidneys to keep the right balance of fluid in your body.
What is the difference between ICD-10 code N18 31 and N18 32?
N18. 31- Chronic Kidney Disease- stage 3a. N18. 32- Chronic Kidney Disease- stage 3b.
Can you code E11 22 and N18 9?
6).” Code N18. 9 is not included in this range of codes and provides no further specificity. In this case, only E11. 22 would be needed for DM with CKD of unspecified stage.
Is renal insufficiency the same as chronic kidney disease?
Chronic renal insufficiency causes a slow loss of renal function. It is basically the end stage of chronic renal disease, which means the patient often requires dialysis treatment.
What is the ICd 10 code for renal failure?
ICD 10 features multiple codes for renal failure as compared to ICD 9. The order of listing in ICD 10 is as follows: N00-N99 Diseases of the genitourinary system › N17-N19 Acute kidney failure and chronic kidney disease. It is important to note that ICD 10 distinguishes between acute renal insufficiency and acute kidney injury/acute renal failure. There are additional codes to specify traumatic and non-traumatic kidney injury. Acute kidney disease and acute renal insufficiency cannot be reported as acute renal failure.
What happens if you don't treat CKD?
A problem that affects over twenty six million Americans, CKD (Chronic kidney disease) if not treated in time can lead to acute kidney injury or acute renal failure. Your kidney filters excess fluids, salt and waste from your blood.
What causes CKD?
Causes of CKD. The leading cause of CKD is diabetes. However, there are a number of factors that can lead to acute renal failure. Reduced blood flow to your kidneys due to conditions like low blood pressure, dehydration, burns, injury, hemorrhage, serious illness, septic shock and surgery can cause damage leading to acute renal failure.
What causes clotting in the blood vessels in the kidney?
Clotting in the blood vessels within the kidney due to conditions like idiopathic thrombocytopenic thrombotic purpura (ITTP), malignant hypertension, hemolytic uremic syndrome, transfusion reaction, and scleroderma can also lead to acute renal failure.
Can kidney failure be life threatening?
The loss of the filtering ability of your kidney, leads to accumulation of waste material and electrolytes in your body, eventually leading to acute renal failure which can be life threatening. However, proper and timely treatment can reverse the damage and help you recover from the problem.
What is a pre renal disease?
A disorder characterized by the acute loss of renal function and is traditionally classified as pre-renal (low blood flow into kidney), renal (kidney damage) and post-renal causes (ureteral or bladder outflow obstruction).
What is a clinical syndrome characterized by a sudden decrease in glomerular filtration rate?
Clinical syndrome characterized by a sudden decrease in glomerular filtration rate, usually associated with oliguria and always associated with biochemical consequences of the reduction in glomerular filtration rate such as a rise in blood urea nitrogen (bun) and serum creatinine concentrations.
When will ICD-10 N17.9 be released?
The 2022 edition of ICD-10-CM N17.9 became effective on October 1, 2021.
When will the ICd 10 T86.12 be released?
The 2022 edition of ICD-10-CM T86.12 became effective on October 1, 2021.
What is the secondary code for Chapter 20?
Use secondary code (s) from Chapter 20, External causes of morbidity, to indicate cause of injury. Codes within the T section that include the external cause do not require an additional external cause code. Type 1 Excludes.
What is renal failure?
A disorder characterized by gradual and usually permanent loss of kidney function resulting in renal failure.
What is the end stage of renal insufficiency?
The end-stage of chronic renal insufficiency. It is characterized by the severe irreversible kidney damage (as measured by the level of proteinuria) and the reduction in glomerular filtration rate to less than 15 ml per min (kidney foundation: kidney disease outcome quality initiative, 2002). These patients generally require hemodialysis or kidney transplantation.
Why is my kidney unable to remove waste?
This damage may leave kidneys unable to remove wastes. Causes can include genetic problems, injuries, or medicines. You are at greater risk for kidney disease if you have diabetes, high blood pressure, or a close family member with kidney disease. chronic kidney disease damages the nephrons slowly over several years.
What is kidney impairment?
Impairment of health or a condition of abnormal functioning of the kidney.
When will the ICd 10 N18.9 be released?
The 2022 edition of ICD-10-CM N18.9 became effective on October 1, 2021.
What is the function of kidneys?
Their main job is to filter wastes and excess water out of your blood to make urine. They also keep the body's chemical balance, help control blood pressure, and make hormones.chronic kidney disease (ckd) means that your kidneys are damaged and can't filter blood as they should.
What type of diabetes causes hypertension concurrent with end stage renal disease?
Hypertension concurrent and due to end stage renal disease on dialysis due to type 2 diabetes mellitus
When will the 2022 ICd-10-CM N18.6 be released?
The 2022 edition of ICD-10-CM N18.6 became effective on October 1, 2021.
What type of kidney disease is associated with hyperparathyroidism?
Chronic kidney disease due to type 2 diabetes mellitus with hyperparathyroidism due to end stage renal disease on dialysis
What does the title of a manifestation code mean?
In most cases the manifestation codes will have in the code title, "in diseases classified elsewhere.". Codes with this title are a component of the etiology/manifestation convention. The code title indicates that it is a manifestation code.
What is renal failure?
Renal disease usually results from damage to one of four major structures of the kidney: the tubules, the glomeruli, the interstitium, or the intrarenal blood vessels. Renal disease is classified as acute or chronic.
What is renal insufficiency?
It’s generally accepted that renal insufficiency (593.9 Unspecified disorder of the kidney and ureter) refers to the early stages of renal impairment, determined by mildly abnormal elevated values of serum creatinine or BUN, or diminished creatinine clearance.
What is AKI in medical terms?
Renal disease is classified as acute or chronic. Today, the term acute kidney injury (AKI) replaces the term acute renal failure (ARF). AKI equates to an abrupt decline in renal function, associated with a 50-80 percent mortality rate. The etiologies for AKI are often described as pre-, intra-, or post-renal.
What causes intra renal AKI?
Causes of intra-renal AKI are usually due to diseases of the renal vessels, diseases of the renal microcirculation and glomeruli, effects of ischemia or nephrotoxic drugs, and/or tubo-interstitial inflammation.
What is the GFR of urine?
The rate of ultrafiltration through the glomerulus depends on many variables. The glomerular filtration rate (GFR) is often used as a measure of renal health. It’s normally greater than (>) 60.
What is the kidney system?
Physiology is the key to better diagnosis coding. The renal system consists of two kidneys (each of which usually has an adrenal gland perched on top), two ureters, a bladder, and a urethra. This article focuses on renal failure and the physiology behind code selection.
What is a chronic kidney disease?
Chronic kidney disease is defined as either kidney damage or < 60 mL/min/1.73 m 2 for ≥ 3 months. Kidney damage is defined as pathologic abnormalities or markers of damage, including abnormalities in blood or urine tests or imaging studies.

Popular Posts:
- 1. icd 10 code for thyroiditis
- 2. icd-10 code for portal gastropathy
- 3. icd 9 code for vascular site hematoma
- 4. icd 10 code for pelvic vascular congestion
- 5. icd 10 cm code for r clavicle pain
- 6. icd 9 code for three-vessel coronary artery disease
- 7. icd 10 code for low grade squamous intraepithelial lesion
- 8. icd 10 code for swelling in breast
- 9. icd 10 code for counseling on how to use a nebulizer
- 10. icd 10 code for chronic cervical spine pain