What are the new ICD 10 codes?
Feb 25, 2015 · Transitioning to ICD-10. The International Classification of Diseases, or ICD, is used to standardize codes for medical conditions and procedures. While most countries already use the 10th revision of these codes (or ICD-10), the United States has yet to adopt this convention. The Centers for Medicare & Medicaid Services (CMS) is working closely with all …
What is the CPT code for transition of care?
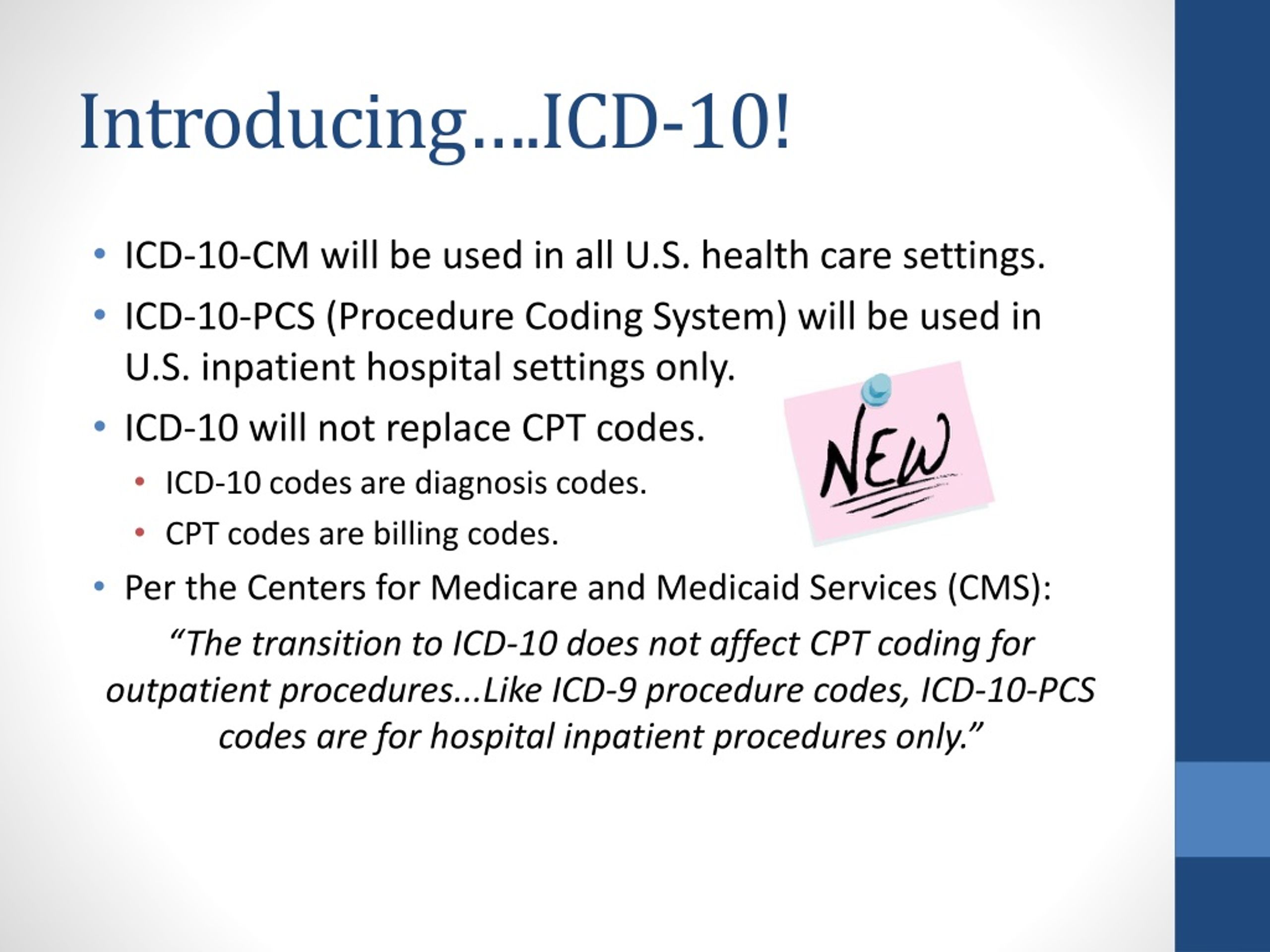
The transition to ICD-10 is coordinated by the Centers for Medicare & Medicaid Services (CMS) in the Department of Health and Human Services (HHS) and is mandatory throughout the country. ICD-10 codes are alpha-numeric and have different format than ICD-9 codes, thus, providing more detailed information.
What is transition of care?
Aug 19, 2014 · to comply with the transition to ICD-10, which means: l. All electronic transactions must use Version 5010 standards, which have been required since January 1, 2012. Unlike the older Version 4010/4010A standards, Version 5010 accommodates ICD-10 codes. l. ICD-10 diagnosis codes must be used for all health care services provided in
What does ICD - 10 stand for?
Oct 01, 2021 · Z71.89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z71.89 became effective on October 1, 2021. This is the American ICD-10-CM version of Z71.89 - other international versions of ICD-10 Z71.89 may differ.

What is the CPT code for transition of care?
The two CPT codes used to report TCM services are: CPT code 99495 – moderate medical complexity requiring a face-to-face visit within 14 days of discharge. CPT code 99496 – high medical complexity requiring a face-to-face visit within seven days of discharge.
What is DX code Z71 89?
Other specified counselingICD-10 code Z71. 89 for Other specified counseling is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is the ICD-10 code for new patient establishing care?
Z01. 89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z01. 89 became effective on October 1, 2021.
What is the ICD-10 code for palliative care?
Z51.5You should report ICD-10 code Z51. 5, “Encounter for palliative care,” in addition to codes for the conditions that affect your decision making.
What is diagnosis code Z51 81?
Encounter for therapeutic drug level monitoring. Z51. 81 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What does CPT code 99401 mean?
CPT 99401: Preventative medicine counseling and/or risk factor reduction intervention(s) provided to an individual, up to 15 minutes may be used to counsel commercial members regarding the benefits of receiving the COVID-19 vaccine.Sep 13, 2021
Can Z71 89 be primary diagnosis?
The code Z71. 89 describes a circumstance which influences the patient's health status but not a current illness or injury. The code is unacceptable as a principal diagnosis.
When should Z76 89 be used?
The code Z76. 89 is valid during the fiscal year 2022 from October 01, 2021 through September 30, 2022 for the submission of HIPAA-covered transactions. The ICD-10-CM code Z76.
Can Z79 899 be a primary diagnosis?
899 or Z79. 891 depending on the patient's medication regimen. That said, it was always a supporting diagnosis, never primary. It might be okay for primary for drug testing or something of the sort.Mar 7, 2019
What is DX code Z51 5?
Encounter for palliative care5: Encounter for palliative care.
How do you code end of life care?
CPT code 99497 is used for the first 30 minutes and pays about $86 for outpatient visits and $80 for inpatient visits. CPT code 99498 is used thereafter and provides payment of $75 for each additional 30-minute period.Jul 8, 2019
What is the CPT code for palliative care?
CPT code 99497* - first 30 minutesNon Facility$80.25CPT code 99498** - each additional 30 minutesNon Facility$70.39Facility$70.395 more rows
When did HIPAA change to electronic health care?
The Department of Health and Human Services (HHS) has mandated that all entities covered by the Health Insurance Portability and Accountability Act#N#External#N#file_external#N#(HIPAA) must all transition to a new set of codes for electronic health care transactions on October 1, 2015.
Is ICd 10 PCS better than ICd 9?
The granularity of ICD-10-CM and ICD-10-PCS is vastly improved over ICD-9-CM and will enable greater specificity in identifying health conditions. It also provides better data for measuring and tracking health care utilization and the quality of patient care.
What Is It?
How Are Non-Hipaa and Public Health Entities Affected?
Why Change?
- The periodic revisions of ICD-9-CM mirror changes in the medical and health care field. The U.S. has been using ICD-9-CM since 1979, and it is not sufficiently robust to serve the health care needs of the future. The content is no longer clinically accurate and has limited data about patients’ medical conditions and hospital inpatient procedures, the number of available codes is …
Code Set Differences
- ICD-9-CM codes are very different than ICD-10-CM/PCS code sets: 1. There are nearly 19 times as many procedure codes in ICD-10-PCS than in ICD-9-CM volume 3 2. There are nearly 5 times as many diagnosis codes in ICD-10-CM than in ICD-9-CM 3. ICD-10 has alphanumeric categories instead of numeric ones 4. The order of some chapters have changed, some titles have been ren…
Transition Deadline
- The transition to ICD-10-CM/PCS code sets will take effect on October 1, 2015 and all users will transition to the new code sets on the same date. For secondary users, this means that the data you receive will be coded in ICD-10-CM/PCS beginning on October 1, 2015. There will be some ICD-9-CM codes still circulating in the system for services provi...
Benefits to Public Health of The New Coding Sets
- Although the transition to ICD-10-CM/PCS codes sets will be a major change, there are significant advantages that the new coding system has over ICD-9-CM. Some noteworthy benefits include:
Popular Posts:
- 1. how to code icd 10 for leg ucchry
- 2. icd 10 dx code for urinary retention
- 3. icd 10 code for left knee medial collateral ligament sprain
- 4. icd 10 code for anastomotic site of colon biopsy
- 5. icd 9 code for adjustment disorder with mixed anxiety and depressed mood
- 6. icd 10 code for hx of crohn's disease
- 7. icd 10 code for dvt in left leg
- 8. icd 10 code for basal cell carcinoma in back of neck
- 9. icd 10 code for hemachezia
- 10. icd 10 code for general check up