Code 99495 requires moderately complex medical decision-making and a face-to-face visit within 14 days. Code 99496 requires highly complex medical decision-making and a face-to-face visit within seven days. Transitional care management (TCM
Turner Classic Movies
Turner Classic Movies is an American movie-oriented pay-TV network operated by Warner Bros. Entertainment, a subsidiary of AT&T's WarnerMedia. Launched in 1994, TCM is headquartered at Turner's Techwood broadcasting campus in the Midtown business district of Atlan…
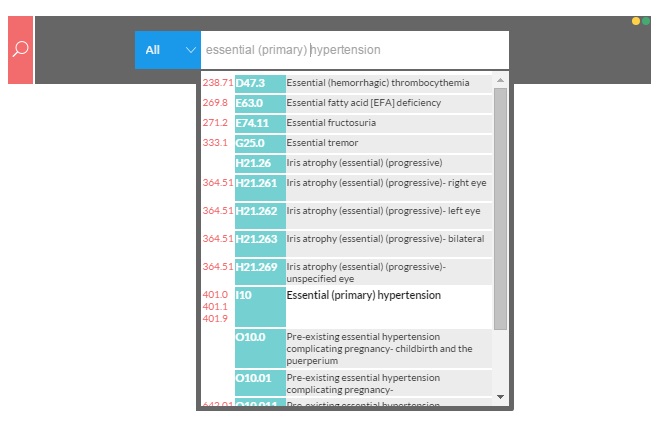
What are the new ICD 10 codes?
Jul 08, 2019 · One of those services is transition care management (TCM). These CPT® codes allow for reimbursement of the care provided when patients transition from an acute care or hospital setting back into the community setting (home, domiciliary, rest home, assisted living). TCM commences upon date of discharge and then for the next 29 days.
What is the CPT code for transition of care?
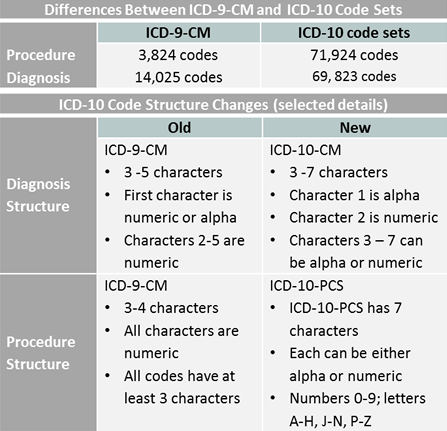
Feb 25, 2015 · Transitioning to ICD-10. The International Classification of Diseases, or ICD, is used to standardize codes for medical conditions and procedures. While most countries already use the 10th revision of these codes (or ICD-10), the United States has yet to adopt this convention. The Centers for Medicare & Medicaid Services (CMS) is working closely with all …
What is transition of care?
Aug 19, 2014 · to comply with the transition to ICD-10, which means: l. All electronic transactions must use Version 5010 standards, which have been required since January 1, 2012. Unlike the older Version 4010/4010A standards, Version 5010 accommodates ICD-10 codes. l. ICD-10 diagnosis codes must be used for all health care services provided in
What does ICD - 10 stand for?
How to Transition Your Primary Care Practice ICD-10 Coding Guidelines Physicians who assign their own codes must—at a minimum—read the CDC’s 2015 ICD-10-CM Official Guidelines for Coding and Reporting. This docu-ment is a treasure trove of information that includes little known facts about the new coding system physicians could easily ...
What is the CPT code for transition of care?
The two CPT codes used to report TCM services are: CPT code 99495 – moderate medical complexity requiring a face-to-face visit within 14 days of discharge. CPT code 99496 – high medical complexity requiring a face-to-face visit within seven days of discharge.
What is DX code Z71 89?
Other specified counselingICD-10 code Z71. 89 for Other specified counseling is a medical classification as listed by WHO under the range - Factors influencing health status and contact with health services .
What is the ICD-10 code for new patient establishing care?
Z01. 89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z01. 89 became effective on October 1, 2021.
Can Z71 89 be used as a primary diagnosis?
The code Z71. 89 describes a circumstance which influences the patient's health status but not a current illness or injury. The code is unacceptable as a principal diagnosis.
What is diagnosis code Z51 81?
2022 ICD-10-CM Diagnosis Code Z51. 81: Encounter for therapeutic drug level monitoring.
What does CPT code 99401 mean?
CPT 99401: Preventative medicine counseling and/or risk factor reduction intervention(s) provided to an individual, up to 15 minutes may be used to counsel commercial members regarding the benefits of receiving the COVID-19 vaccine.Sep 13, 2021
What is R53 83?
ICD-10 | Other fatigue (R53. 83)
What is establish care?
What is establishing care? Establishing care happens when a patient chooses a single provider to be their primary source of medical care. It sets up patients to have a consistent and trusted source for all their primary care medical needs.Sep 23, 2021
What diagnosis code should be billed with 99497?
99497, Advance care planning including the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified health care professional; first 30 minutes, face-to-face with the patient, family member(s), and/or surrogate.Mar 28, 2016
What is the ICD-10 code for consultation?
Z71. 0 - Person encountering health services to consult on behalf of another person. ICD-10-CM.
What is the ICD-10 code for palliative care?
Z51.5You should report ICD-10 code Z51. 5, “Encounter for palliative care,” in addition to codes for the conditions that affect your decision making.
What is Table 2 in ICD-10?
Table 2 is an excerpt from a code map for an internal medicine practice. The top 20 diagnosis codes by frequency as a primary or secondary diagnosis from the previous ten months were identified, and then mapped to the equivalent ICD-10 codes. Depending on the complexity of your practice, it may be more appropriate to identify the top 50 or even top 100 codes to map.
How does ICD-10 affect practice?
ICD-10 could affect many aspects of your practice’s workflow. You will need to evaluate your current workflow to look for areas where you need to make updates or changes and identify potential delays.
What is the ICD-10 for cerebral infarction?
ICD-10 requires far more detail in terms of the location of an injury or condition. For example, a patient presents with a cerebral infarction due to an embolism. Physicians must document precisely where the embolism occurred, including laterality as well as the specific artery (i.e., in the pre- cerebral artery, carotid artery, basilar artery, vertebral artery, middle cerebral artery, anterior cerebral artery, posterior cerebral artery, or cerebellar artery).
Who is Lea Chatham?
Lea Chatham is the content marketing manager at Kareo, responsible for developing educational resources to help small medical practices improve their businesses. She joined Kareo after working at a small integrated health system for more than five years developing marketing and educational tools and events for patients. Prior to that, Lea was a marketing coordinator for Medical Manager Health Systems, WebMD Practice Services, Emden, and Sage Software. She specializes in simplifying information about healthcare and healthcare technology for physicians, practice staff, and patients.
How long does it take to see a reduction in productivity?
Many experts are suggesting that you should expect to see a reduction in productivity and revenue for about three months of up to 50% (and some say as much as six months). You’re a small business with bills to pay so you need to plan for a potential loss of revenue. If you can’t pay your rent, utilities, and employees, it will be hard to keep the doors open.
Who is Lisa Eramo?
Lisa Eramo is a freelance writer/editor specializing in health information management, medical coding, and healthcare regulatory topics. She began her healthcare career as a referral specialist for a well-known cancer center. Lisa went on to work for several years at a healthcare publishing company. She regularly contributes to healthcare publications, websites, and blogs, including the AHIMA Journal and AHIMA Advantage. Her areas of focus are medical coding, and ICD-10 in particular, clinical documentation improve-ment, and healthcare quality/efficiency.
What is kareo software?
Kareo is the only cloud-based medical office software and services platform purpose-built for small practices. At Kareo, we believe that, with the right tools and support, small practices can do big things. We offer an integrated solution of products and services designed to help physicians get paid faster, find new patients, run their business smarter,
What is the CPT code for transitional care management?
The CPT® guidelines for transitional care management (TCM) codes 99495 and 99496 seem straightforward, initially, but the details are trickier than is commonly recognized. Here’s what you need to know to report these services appropriately.
Who is Michael Warner?
Michael Warner, DO, CPC, CPCO, CPMA, AAPC Fellow, is an associate professor at Touro University California, president of non-profit Patient Advocacy Initiatives, alternate advisor on AMA RUC, and an AAPC National Advisory Board member. At Touro, he is conducting a series of research projects with the online tool www.PreHx.com to determine evidence-based best practices to accommodate a patient-authored medical history and improve data gathering flow.
What is the CCM code for Medicare?
Other reasonable and necessary Medicare services like chronic care management (CCM) may be reported during the 30 day period, with the exception of those services that cannot be reported according to CPT guidance and Medicare HCPCS codes G0181 and G0182.
What is Medicare 99495?
Codes 99495 and 99496 are used to report physician or qualified non-physician practitioner care management services for a patient following the patient’s discharge from an inpatient hospital, partial hospital, observation status in a hospital, skilled nursing facility/nursing facility, or community mental health center to the patient’s community healthcare setting, including home, domiciliary, rest home, or assisted living.
How long does it take to report TCM?
CPT guidance for TCM services states that only one individual may report TCM services and only once per patient within 30 days of discharge. Another TCM may not be reported by the same individual or group for any subsequent discharge (s) within 30 days.
How long does it take to communicate with a patient after discharge?
Both TCM codes require communication with the patient or caregiver within two business days (not calendar days) of discharge. Specifically, CPT guidelines state, “The contact may be direct (face-to-face), telephonic, or by electronic means [e.g., e-mail].”.
Popular Posts:
- 1. icd-10 code for attention to cast cast removal
- 2. icd 10 code for sputum production
- 3. icd 10 code for hyperactivity
- 4. icd 10 code for discomfort
- 5. icd 10 cm code for right ankle sprain
- 6. icd 10 code for neuropathy in association with injury
- 7. icd-10-cm code for obstructive prostate with urinary retention
- 8. icd-10 code for left knee medial meniscus tear
- 9. icd code for twin pregnancy
- 10. icd 10 code for pth