ICD-10 Codes Indicating Trigger Point Injections M79 – Other and unspecified soft tissue disorders, not elsewhere classified M79.0 – Rheumatism, unspecified
How do I find the ICD 10 code for trigger point injections?
For a list of ICD-10-CM codes that may support medical necessity for trigger point injections, be sure to look up 20552 or 20553 in findacode.com and on the code page click on the tab titled "Cross-A-Code" for a list of Medicare-approved ICD-10-CM codes that support medical necessity for these codes.
When to request medical records for a trigger point diagnosis?
This contractor may request records when it is apparent that patients are requiring a significant number of injections to manage their pain. These are the only covered ICD-10-CM codes that support medical necessity. This A/B MAC will assign the following ICD-10-CM codes to indicate the diagnosis of a trigger point.
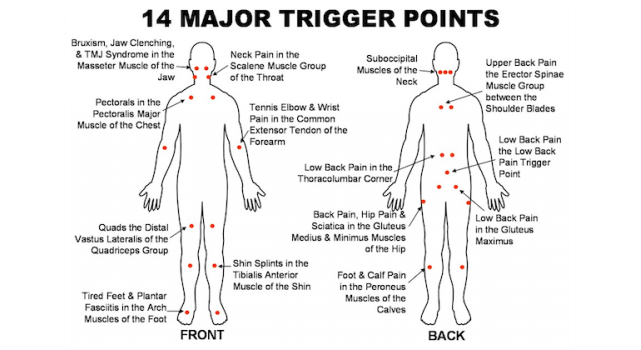
What is a trigger point in the upper back?
Trigger points are focal areas of muscle spasm, (often located in the upper back and shoulder areas) that develops when a small portion of myofascia (the tissue covering the muscle) tightly contracts to itself by cutting off its blood supply and preventing the underlying muscle from working properly.
Can I bill Medicare for trigger point injections (LCD)?
This Billing and Coding Article provides billing and coding guidance for Local Coverage Determination (LCD) L35010, Trigger Point Injections. Please refer to the LCD for reasonable and necessary requirements. Notice: It is not appropriate to bill Medicare for services that are not covered (as described by the entire LCD) as if they are covered.
What is a trigger point injection?
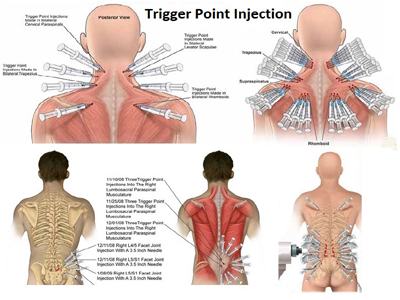
Trigger point injections are a pain management treatment that involves injecting a local anesthetic, sometimes combined with a steroid medication, into a trigger point to relax muscles and relieve pain.
Can you bill an office visit with a trigger point injection?
The office visit is allowed and should be billed with the modifier -25 because the decision to give the injections was made after the examination.
How do you document trigger point injections?
When coding for trigger point injections, the documentation must include the site of the injection, the total number of injections and the number of muscles involved. In addition, documentation must also support that various conservative therapies have been tried and failed.
How do you code a bilateral trigger point injection?
HOW TO BILL BILATERAL TRIGGER POINT INJECTION20552 Injection(s); single or multiple trigger point(s), 1 or 2 muscle(s)20553 Injection(s); single or multiple trigger point(s), 3 or more muscles.
What is the CPT code for trigger point injections?
Group 1CodeDescription20552INJECTION(S); SINGLE OR MULTIPLE TRIGGER POINT(S), 1 OR 2 MUSCLE(S)20553INJECTION(S); SINGLE OR MULTIPLE TRIGGER POINT(S), 3 OR MORE MUSCLES
Will Medicare pay for trigger point injections?
Medicare does not cover Prolotherapy. Its billing under the trigger point injection code is a misrepresentation of the actual service rendered. When a given site is injected, it will be considered one injection service, regardless of the number of injections administered.
What is the ICD 10 code for trigger point?
20553-Injection(s); single or multiple trigger point(s), 3 or more muscles.
What diagnosis covers trigger point injections?
A Medicare beneficiary must be diagnosed with myofascial pain syndrome (MPS), which is a chronic pain disorder, in order for Medicare to cover trigger point injections. A doctor or provider will review the beneficiary's medical history and complete an exam of the patient to make this diagnosis.
What are trigger point injections in back?
A trigger point injection is an outpatient procedure designed to reduce or relieve the back pain caused by trigger points, which are small knots that form in muscles or in the fascia tissue leading to pain caused by muscle irritation (myofascial pain).
What is the difference between 20550 and 20551?
CPT code 20550 defines an injection to the tendon sheath; CPT code 20551 defines an injection to the origin/insertion site of a tendon. CPT code 20550 is frequently used for a trigger finger injection, where the injection is administered to the tendon sheath.
Where are trigger point injections?
A trigger point injection can help soothe muscle pain, especially in your arms, legs, lower back and neck. It also can be used to treat fibromyalgia, tension headaches and myofascial pain. Trigger points are painful “knots” in your muscles. They form when a muscle can't relax.
What is the ICD 10 code for myofascial pain?
ICD-10-CM Code for Myalgia M79. 1.
How do you bill for lidocaine injection?
To bill for lidocaine, report J3490 [Unclassified drugs]. Lidocaine would be included as a supply with code 58999 and therefore not separately billable.
When can you bill for lidocaine?
You cannot bill the drug since it can only be billed if administered IV, therefor you cannot bill the admin code either. Administration of a local anesthetic is inclusive to the procedure.
Is CPT code 20550 covered by Medicare?
General Guidelines for claims submitted to or Part A or Part B MAC: Claims for the injection of collagenase clostridium histolyticum should be submitted with CPT code 20550. CPT code 20550 should be reported once per cord injected regardless of how many injections per session.
Does CPT 20553 need a modifier?
Key point to remember! - these 2 CPT Codes 20552, 20553 DO NOT NEED A MODIFIER!
How many CPT codes are there for trigger point injections?
There are two CPT ® codes for Trigger point injections:
What is trigger point injection?
Trigger point injection therapy is a common procedure performed by pain management specialists, orthopedic surgeons, physical medicine and rehab and other specialties. Trigger point injection therapy is used for the treatment of myofascial pain syndrome (MPS). According to the American Society of Regional Anesthesia and Pain Medicine.
How many trigger point injections are needed in a year?
There is no peer-reviewed literature to substantiate more than four trigger point injections in a year”.
How many sets of injections are needed for pain?
Up to 4 sets of injections are considered medically necessary to diagnose the origin of the patient’s pain and to achieve a therapeutic effect; additional sets of trigger point injections are not considered medically necessary if not clinical response is achieved.
What is the CPT code for MPS?
There are two CPT ® codes for Trigger point injections: 20552-Injection (s); single or multiple trigger point (s), 1 or 2 muscle (s) ...
Is dry needling of trigger point investigational covered by all payers?
Most payers consider dry needling of trigger point investigational and not covered by all payers.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
What is a trigger point in a muscle?
Those knots are referred to as trigger points and they can be very painful. As a matter of fact, a trigger point (TP) in one area can cause surrounding muscles to tighten or spasm, increasing pain and discomfort for the patient. Over-the-counter pain medications, anti-inflammatories, or even a good massage, may help to alleviate some symptoms, ...
How many injections are in 20552?
Three injections were given into the right shoulder (no specific muscle noted). This is counted as 1 unit of 20552. Four injections into the right gluteus maximus and two into the right biceps femoris were administered is counted as two muscles or 20552.
How many injections were given into the right shoulder?
Three injections were given into the right shoulder (no specific muscle noted). This is counted as 1 unit of 20552.
What is L33912 in billing?
This First Coast Billing and Coding Article for Local Coverage Determination (LCD) L33912 Inject ion of Trigger Points provides billing and coding guidance for diagnosis limitations that support diagnosis to procedure code automated denials. However, services performed for any given diagnosis must meet all of the indications and limitations stated in the LCD, the general requirements for medical necessity as stated in CMS payment policy manuals, any and all existing CMS national coverage determinations, and all Medicare payment rules.
What is the medical record for injections?
The medical record must clearly indicate the number of injections given per session and the site (s) injected. Furthermore, the medical record must clearly document the medical necessity for repeated injections of trigger point (s). When frequent injections are required, the medical record must reflect the reason for repeated injections.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Can a CPT/HCPCS be billed with a CPT/HCPCS?
Note: The contractor has identified the Bill Type and Revenue Codes applicable for use with the CPT/HCPCS codes included in this article. Providers are reminded that not all CPT/HCPCS codes listed can be billed with all Bill Type and/or Revenue Codes listed. CPT/HCPCS codes are required to be billed with specific Bill Type and Revenue Codes. Providers are encouraged to refer to the CMS Internet-Only Manual (IOM) Pub. 100-04, Medicare Claims Processing Manual, for further guidance.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
When will the ICd 10-CM M79.1 be released?
The 2022 edition of ICD-10-CM M79.1 became effective on October 1, 2021.
What is the medical term for pain in the neck, shoulders, back, hips, and legs?
M60.-) (my-al-juh) pain in a muscle or group of muscles. A chronic disorder of unknown etiology characterized by pain, stiffness, and tenderness in the muscles of neck, shoulders, back, hips, arms, and legs. Other signs and symptoms include headaches, fatigue, sleep disturbances, and painful menstruation.
What is a thoracic myofascial pain syndrome?
Clinical Information. (my-al-juh) pain in a muscle or group of muscles. A chronic disorder of unknown etiology characterized by pain, stiffness, and tenderness in the muscles of neck, shoulders, back, hips, arms, and legs.
How often should trigger point injections be performed?
It is expected that trigger point injections would not usually be performed more often than three sessions in a three month period. If trigger point injections are performed more than three sessions in a three month period, the reason for repeated performance and the substances injected should be evident in the medical record and available to the Contractor upon request.
Which section of the Social Security Act excludes routine physical examinations?
Title XVIII of the Social Security Act, Section 1862 (a) (7). This section excludes routine physical examinations.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Popular Posts:
- 1. icd 10 code for hpv infection
- 2. icd 10 code for history of carcinoma of large intestine
- 3. icd 10 code for wellness exam without abnormal findings
- 4. icd 9 code for choking episode
- 5. icd 10 code for low testosterone syndrome
- 6. icd 10 code for 2nd metacarpal fracture
- 7. icd 10 code for medication refill request
- 8. 2016 icd 10 code for stepped into a hole
- 9. icd-10 code for ischemic bowel unspecified
- 10. icd 10 code for prominent frenum