What is the best treatment for a diabetic foot ulcer?
Treatment
- Debridement. Debridement should be carried out in all chronic wounds to remove surface debris and necrotic tissues.
- Off-loading. Off-loading of the ulcer area is extremely important for the healing of plantar ulcers. ...
- Dressings. ...
- Growth Factors. ...
- Bioengineered Skin Substitutes. ...
- Extracellular Matrix Proteins. ...
- Negative-Pressure Wound Therapy. ...
How is a diagnosis of diabetes mellitus confirmed?
- Symptoms are present and fasting blood test result is at or above 7.0mmol/L or a random blood test result is at or above 11.1mmol/L
- HbA1c blood test result is at or above 6.5% (48 mmol/mol)
- There have been no symptoms and two abnormal blood glucose tests (as above) on separate days.
How to prevent and treat diabetic foot ulcers?
- Maintain healthy blood sugar levels through a healthy diet and by taking medications as instructed by your doctor.
- Keep your blood pressure within a healthy range.
- Avoid alcohol and tobacco.
What is the prognosis of diabetic ulcers?
Diabetic foot ulcers can take several weeks to heal. Ulcers may take longer to heal if your blood sugar is high and if constant pressure is applied to the ulcer. Remaining on a strict diet and off-loading pressure from your feet is the most effective way to allow your foot ulcers to heal.
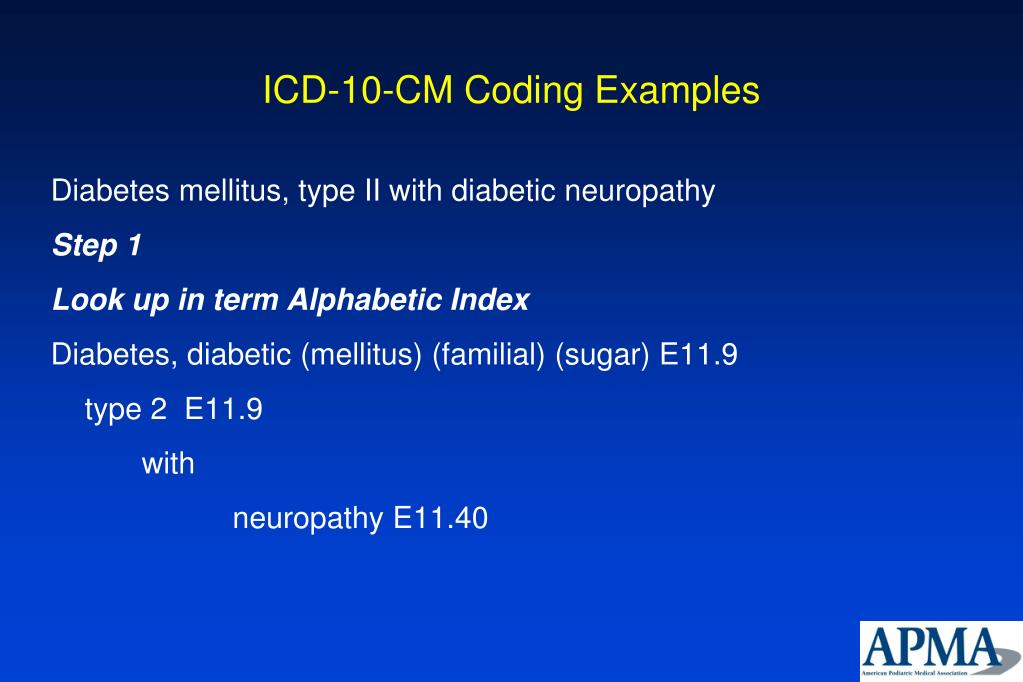
What is the ICD-10 code for diabetic foot ulcer?
ICD-10 Code for Type 2 diabetes mellitus with foot ulcer- E11. 621- Codify by AAPC.
What is the ICD-10 code for ulcer of foot?
ICD-10-CM Code for Non-pressure chronic ulcer of other part of unspecified foot with unspecified severity L97. 509.
Is a diabetic foot ulcer a pressure ulcer?
Skin necrosis and gangrene are also included in the current system as ulcers.” This definition is similar to that of the EPUAP, all-inclusive and, as such, any pressure ulcer on the foot of a person with diabetes is a diabetic foot ulcer — as is any traumatic wound, including a thermal or chemical injury.
What is the ICD-10 code for diabetic foot ulcer left foot?
529: Non-pressure chronic ulcer of other part of left foot with unspecified severity.
What is the ICD-10 diagnosis code for right foot ulcer?
ICD-10 Code for Non-pressure chronic ulcer of other part of right foot with unspecified severity- L97. 519- Codify by AAPC.
What is a diabetic foot ulcer?
A diabetic foot ulcer is an open sore or wound that occurs in approximately 15 percent of patients with diabetes, and is commonly located on the bottom of the foot. Of those who develop a foot ulcer, six percent will be hospitalized due to infection or other ulcer-related complication.
How do you code a diabetic with a pressure ulcer?
The coder would then report ICD-10-CM code L89. 623 (pressure ulcer of left heel, stage 3), as a secondary diagnosis. The coder would assign codes E11. 51 (Type 2 diabetes mellitus with diabetic peripheral angiopathy without gangrene) and E11.
Is a diabetic ulcer considered a stasis ulcer?
There are four (4) common types of skin ulcers: venous stasis ulcers, arterial ulcers, diabetic neuropathic ulcers and pressure ulcers. Three (3) of these ulcer types are exclusively lower-extremity wounds located on the foot, ankle and lower leg: venous stasis ulcers, arterial ulcers, and diabetic neuropathic ulcers.
What is the difference between a pressure ulcer and a non pressure ulcer?
The term “non-pressure ulcer” was coined to designate a primary mechanism other than shear or pressure. If there is poor circulation, such as that caused by venous or arterial insufficiency or excessive moisture or trauma, a patient may develop a non-pressure ulcer.
Whats the difference between a pressure ulcer and a diabetic ulcer?
While diabetic patients can get pressure ulcers due to abuse or neglect in a nursing home, diabetic ulcers may appear in areas that are not typically subject to extended pressure—such as the bottoms of the feet when a resident has been lying down. In these cases, a diagnosis of a diabetic ulcer is more apt.
What is the ICD 10 code for diabetic foot ulcer with osteomyelitis?
The primary diagnosis of L97. 522 is appropriate based on what you stated is documented of the wound appearance and measurements. With the detail from the x-ray, add a secondary diagnosis of acute osteomyelitis billed under ICD-10 code M86. 18 (other acute osteomyelitis, other site) since you also stated osteomyelitis.
When do you code E11 69?
ICD-10-CM Code for Type 2 diabetes mellitus with other specified complication E11. 69.
What is a pressure ulcer on the foot?
Bedsores — also called pressure ulcers and decubitus ulcers — are injuries to skin and underlying tissue resulting from prolonged pressure on the skin. Bedsores most often develop on skin that covers bony areas of the body, such as the heels, ankles, hips and tailbone.
Is Leg ulcer A pressure ulcer?
Venous skin ulcers are caused by poor circulation in the legs caused by damaged valves that prevent blood from flowing the wrong way, allowing blood to pool in the legs. Pressure ulcers, on the other hand, are caused by sustained pressure on an area of the body, which cuts off blood flow.
What is a pressure ulcer?
(PREH-sher UL-ser) Damage to an area of the skin caused by constant pressure on the area for a long time. This pressure can lessen blood flow to the affected area, which may lead to tissue damage and tissue death.
What does diabetic foot ulcer look like?
If the ulcer is at an advanced stage, it should be obvious. A foot ulcer looks like a round red crater in the skin bordered by thickened callused skin. Severe ulcers can be deep enough to expose tendons or bones. However, other symptoms may not be easy to identify or could be an indication of another problem.
What is a diabetic foot ulcer?
Regarded as the most common reason for hospital stays among people with diabetes, a diabetic foot ulcer (DFU) is an open sore caused by neuropathic (nerve) and vascular (blood vessel) complications of the disease. Typically located on the plantar surface, or bottom/top of toes, pad of foot, or heel of foot, these complex, ...
How many people with diabetes have foot ulcers?
According to the American Podiatric Medical Association (APMA), approximately 15 percent of people with diabetes suffer from foot ulcers. Of those who develop a foot ulcer, about 6 percent will be hospitalized due to serious infections or other ulcer-related complications.
How are foot ulcers defined?
Typically, foot ulcers are defined by the appearance of the ulcer, the ulcer location, and the way the borders and surrounding skin of the ulcer look. There are different types of diabetic foot ulcers –
How many parts are there in the podiatry billing process?
9 Parts of The Podiatry Billing Process
What are the risk factors for ulcers?
The most common risk factors for ulcer formation include – diabetic neuropathy, structural foot deformity, kidney disease, obesity and peripheral arterial occlusive disease. The condition can be effectively prevented if the underlying conditions causing it are diagnosed early and treated correctly.
What is the most common foot injury leading to lower extremity amputation?
Diabetic ulcers are the most common foot injuries leading to lower extremity amputation. The blog provides a detailed overview of the condition with the ICD-10 codes.
How many amputations are there for diabetics?
The risk of foot ulceration and limb amputations increases with age and duration of diabetes. In the United States, about 82,000 amputations are performed each year on persons with diabetes; half of those ages 65 years or older. Treatment for diabetic foot ulcers varies depending on their causes.
What does "type 1 excludes" mean?
It means "not coded here". A type 1 excludes note indicates that the code excluded should never be used at the same time as E10. A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition.
Does diabetes cause high blood glucose?
With type 1 diabetes, your pancreas does not make insulin. Insulin is a hormone that helps glucose get into your cells to give them energy. Without insulin, too much glucose stays in your blood. Over time, high blood glucose can lead to serious problems with your heart, eyes, kidneys, nerves, and gums and teeth.
What causes diabetic foot ulcers?
A “diabetic foot ulcer,” which is caused exclusively by hyperglycemia, in the absence of neuropathy or ischemia, is a rarity. That term almost always refers to an ulcer on the foot of a diabetic that derives from neuro/ischemic etiology, as opposed to being strictly and principally due to pressure injury.
Why do diabetics get ulcers on their feet?
The American Podiatric Medical Association adds that “ (diabetic foot) ulcers form due to a combination of factors, such as lack of feeling in the foot, poor circulation, foot deformities, irritation (such as friction or pressure), and trauma, as well as duration of diabetes.” They go on to note that “vascular disease can complicate a foot ulcer, reducing the body’s ability to heal and increasing the risk for an infection.”
Why do diabetics have neuropathy?
Neuropathy occurs due to damage to the nerves and causes impaired sensation. After 10 years, ~90 percent of Type 1 and Type 2 diabetics have some degree of neuropathy, most commonly affecting the feet and legs, and 90 percent of diabetic foot ulcers have diabetic neuropathy as a contributing factor. If the diabetic doesn’t recognize discomfort due to nerve impairment, they may not adjust their shoes and socks or seek medical attention for minor cuts or blisters.
What is a malum perforans pedis ulcer?
Neuropathy results in malum perforans pedis (a.k.a. bad perforating foot) ulcers. These are painless, non-necrotic, circular lesions circumscribed by hyperkeratosis. They often overlie a metatarsal head. Ischemic wounds manifest local signs of ischemia such as thin, shiny, hairless skin with pallor and coldness. These are often found at areas of friction and may be painful.
Why are pressure ulcers considered a patient safety indicator?
Pressure ulcers are deemed patient safety indicators and hospital acquired conditions because a concerted program for prevention and treatment can prevent them and protect our patients from iatrogenic harm. The diagnosis of a “pressure ulcer” may trigger prevalence and incident reporting.
Why should we specifically carve out pressure ulcers?
Why should we specifically carve out pressure ulcers? Pressure ulcers are deemed patient safety indicators and hospital acquired conditions because a concerted program for prevention and treatment can prevent them and protect our patients from iatrogenic harm. The diagnosis of a “pressure ulcer” may trigger prevalence and incident reporting.
What is non pressure ulcer?
The term “non-pressure ulcer” was coined to designate a primary mechanism other than shear or pressure. If there is poor circulation, such as that caused by venous or arterial insufficiency or excessive moisture or trauma, a patient may develop a non-pressure ulcer.
What is the ICD-10 code for diabetes?
For gestational diabetes (diabetes that occurs during pregnancy) women should be assigned a code under the 024.4 subheading and not any other codes under the 024 category.
What type of diabetes code should be used for long term use?
The code for long-term use of insulin, Z79.4, should also be used in these cases (unless insulin was just given to the patient as a one-time fix to bring blood sugar under control).
What Are ICD-10 Codes?
ICD-10 codes refer to the codes from the 10th Revision of the classification system. ICD-10 officially replaced ICD-9 in the US in October of 2015.
Why did doctors switch to ICd 10?
The switch to ICD-10 was a response to the need for doctors to record more specific and accurate diagnoses based on the most recent advancements in medicine. For this reason, there are five times more ICD-10 codes than there were ICD-9 codes. The ICD-10 codes consist of three to seven characters that may contain both letters and numbers.
When to use unspecified ICD-10?
The “unspecified” codes can be used when not enough information is known to give a more specific diagnosis; in that case, “unspecified” is technically more accurate than a more specific but as yet unconfirmed diagnosis. For more guidelines on using ICD-10 codes for diabetes mellitus, you can consult this document.
Can diabetes be a ICd 9?
Here's a conversion table that translates the old ICD-9 codes for diabetes to ICD-10 codes. There weren’t as many codes to describe different conditions in the ICD-9, so you’ll notice that some of them have more than one possible corresponding ICD-10 code. Some are also translated into a combination of two ICD-10 codes (note the use of the word "and").

Popular Posts:
- 1. icd-10 code for subcutaneous abcess to right thigh
- 2. icd 10 code for high mcv
- 3. icd 10 code for blindness due to injury initial encounter
- 4. icd 10 code for intertrigo of breast
- 5. what's the icd 10 code for inflammatory polyps of colon with intestinal obstruction
- 6. icd-10 code for right hip intramedullary nailing
- 7. icd 10 code for rob cag pain
- 8. icd 10 code for intentional weight loss
- 9. icd 10 code for necrotizing fasciitis of abdominal wall
- 10. icd 10 code for wrist cyst