What ICD 10 code to use for no diagnosis?
The DSM-5 Steering Committee subsequently approved the inclusion of this category, and its corresponding ICD-10-CM code, Z03. 89 "No diagnosis or condition," is available for immediate use.
What does ICD 10 code R69 mean?
R69 - Illness, unspecified.
What is unspecified diagnosis?
An “unspecified” code means that the condition is unknown at the time of coding. An “unspecified” diagnosis may be coded more specifically later, if more information is obtained about the patient's condition. Example: There are multiple codes for hypothyroidism.
How do you code a suspected diagnosis?
Do not code diagnoses documented as “probable”, “suspected”, “questionable”, “rule out”, or “working diagnosis”. Rather, code the condition(s) to the highest degree of certainty for that encounter/visit, such as symptoms, signs, abnormal test results, or other reason for the visit.
What is diagnosis code Z03 89?
Encounter for observation for other suspected diseases and conditions ruled out. Z03. 89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
What is ICD-10 code R99?
Ill-defined and unknown cause of mortalityICD-10 code R99 for Ill-defined and unknown cause of mortality is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
When do you diagnose other specified and unspecified disorders?
"Other Specified" and "Unspecified" An example of "other specified" might be a depressive episode that does not have the full number of symptoms to meet the formal diagnosis. By contrast, "unspecified" might be used in a situation in which there isn't enough information to make a more specific diagnosis.Feb 24, 2020
When do you use unspecified diagnosis?
According to ICD-10-CM Official Guidelines for Coding and Reporting FY 2018, “unspecified codes are to be used when the information in the medical record is insufficient to assign a more specific code.” In my opinion, this can be the case with testing, when lab work or cultures do not support the more specific code.Apr 27, 2018
What is ICD-10 code Z21?
Asymptomatic human immunodeficiency virus [HIV] infection status. Z21 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
Can you code a clinical diagnosis?
The facility should assign the appropriate code(s) for the conditions documented. This means that if a documented diagnosis does not appear to be clinically supported, the facility is justified in requesting the physician document their rationale via a clinical validation query.Apr 4, 2019
Can I code for possible diagnosis?
In the guidelines, CMS states the following: “Do not code diagnosis documented probable, suspected, questionable, rule out, compatible with, consistent with, or working diagnosis or similar terms indicating uncertainty.Oct 21, 2019
Do you code borderline diagnosis?
Borderline diagnoses A diagnosis that is documented as “borderline” at the time of discharge is coded as a confirmed diagnosis, unless there is a specific index entry in ICD-10-CM for a borderline condition.
What is the code for a primary malignant neoplasm?
A primary malignant neoplasm that overlaps two or more contiguous (next to each other) sites should be classified to the subcategory/code .8 ('overlapping lesion'), unless the combination is specifically indexed elsewhere.
What does "type 1 excludes" mean?
A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition.
What is the ICd 10 code for external cause?
Unspecified external cause status 1 Y99.9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. 2 The 2021 edition of ICD-10-CM Y99.9 became effective on October 1, 2020. 3 This is the American ICD-10-CM version of Y99.9 - other international versions of ICD-10 Y99.9 may differ.
When to use Y99 code?
A single code from category Y99 should be used in conjunction with the external cause code (s) assigned to a record to indicate the status of the person at the time the event occurred.
What is Y99 code?
A single code from category Y99 should be used in conjunction with the external cause code (s) assigned to a record to indicate the status of the person at the time the event occurred . External cause status. Present On Admission. POA Help.
What is a Z00-Z99?
Categories Z00-Z99 are provided for occasions when circumstances other than a disease, injury or external cause classifiable to categories A00 -Y89 are recorded as 'diagnoses' or 'problems'. This can arise in two main ways:
What does "exclude note" mean?
A type 1 excludes note is a pure excludes. It means "not coded here". A type 1 excludes note indicates that the code excluded should never be used at the same time as Z01.84. A type 1 excludes note is for used for when two conditions cannot occur together, such as a congenital form versus an acquired form of the same condition.
What is the 10th revision of the ICD-10?
The International Classification of Diseases, 10th Revision (ICD-10) is the official system to assign health care codes describing diagnoses and procedures in the United States (U.S). The ICD is also used to code and classify mortality data from death certificates.
When was ICD-10-CM implemented?
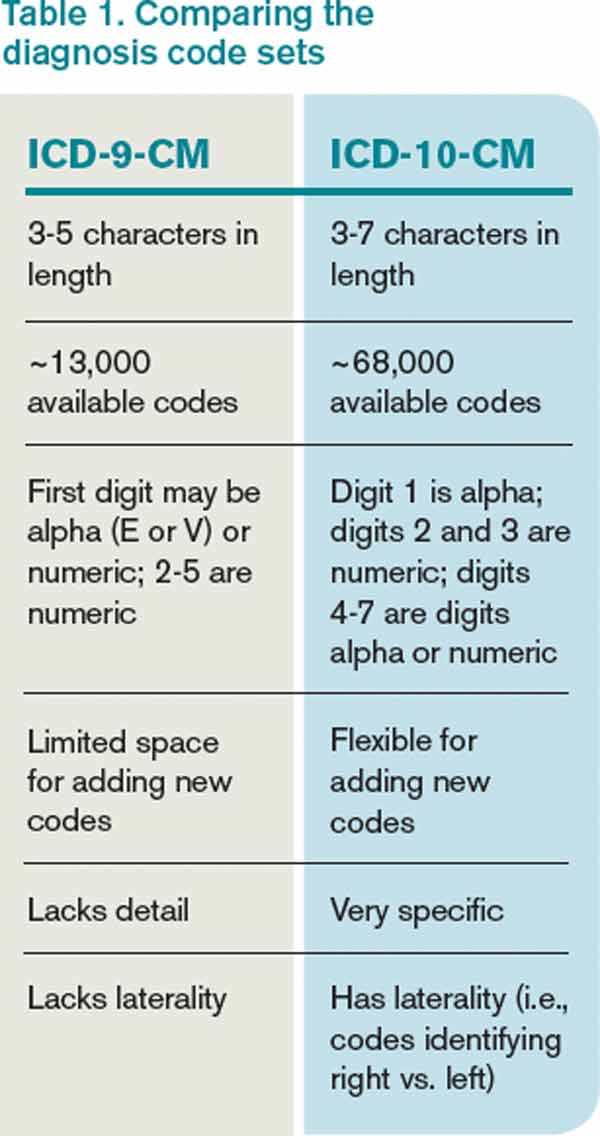
ICD-10 was implemented on October 1, 2015, replacing the 9th revision of ICD (ICD-9).
What is type 1 excludes?
An Excludes1 is used when two conditions cannot occur together , such as a congenital form versus an acquired form of the same condition .
What is the difference between ICD-10 and CM?
The ICD-10-CM has two types of excludes notes. Each note has a different definition for use but they are both similar in that they indicate that codes excluded from each other are independent of each other.
Do SLPs have to report ICD-10 codes?
SLPs practic ing in a health care setting, especially a hospital, may have to code disease s and diagnoses according to the ICD-10. Payers, including Medicare, Medicaid, and commercial insurers, also require SLPs to report ICD-10 codes on health care claims for payment.
What is the code for a primary malignant neoplasm?
A primary malignant neoplasm that overlaps two or more contiguous (next to each other) sites should be classified to the subcategory/code .8 ('overlapping lesion'), unless the combination is specifically indexed elsewhere.
What chapter is neoplasms classified in?
All neoplasms are classified in this chapter, whether they are functionally active or not. An additional code from Chapter 4 may be used, to identify functional activity associated with any neoplasm. Morphology [Histology] Chapter 2 classifies neoplasms primarily by site (topography), with broad groupings for behavior, malignant, in situ, benign, ...
Popular Posts:
- 1. icd-10-pcs code for aneurysm coiling
- 2. icd 10 code for verruca plana
- 3. icd 10 code for thyroid nodule e04.1
- 4. icd 10 code for foraminal stenosis of lumbar region
- 5. icd 10 code for cervical degeneration
- 6. icd 10 code for drug allergy
- 7. icd 10 code for i70.0
- 8. icd 10 code for open stab wound into kidney
- 9. icd 10 code for chronic ptsd
- 10. icd 9 procedure code for family history of dermatitis