What is the ICD 10 code for urgent care center?
Mar 01, 2014 · When using ICD-9, you would use code 816.01, “Closed fracture of middle or proximal phalanx or phalanges of hand.” In ICD-10, you would code S62.622A, “displaced fracture of medial phalanx of right middle finger, initial encounter.” Not only does the code represent the fracture, but it also reports laterality and the type of encounter.
What is the E/M code for urgent care?
Oct 01, 2021 · Y92.532 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. Short description: Urgent care center as place; The 2022 edition of ICD-10-CM Y92.532 became effective on October 1, 2021. This is the American ICD-10-CM version of Y92.532 - other international versions of ICD-10 Y92.532 may differ.
Why are urgent care visits CPT codes s9083 and s9088?
Jan 13, 2021 · These new codes went into effect on January 1, 2021 and replace existing codes that are not specific to COVID-19. Condition. 2020 ICD-10. 2021 ICD-10. Encounter for screening for COVID-19. Z11.59. Z11.52. Contact with and (suspected) exposure to COVID-19. Z20.828.
What is the CPT code for emergency room visit?
Oct 01, 2021 · Z01.89 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM Z01.89 became effective on October 1, 2021. This is the American ICD-10-CM version of Z01.89 - other international versions of ICD-10 Z01.89 may differ.
What is the CPT code for Urgent visit?
When should ICD-10 code Z09 be used?
What is diagnosis code Z71 89?
Can Z76 89 be used as a primary diagnosis?
How do you code for follow-up visits?
What is the ICD-10 for abdominal pain?
What is diagnosis code Z51 81?
What does CPT code 99401 mean?
Is there a ICD 10 code for establishing care?
What is a diagnostic code Z76 9?
What is the ICD-10 code for hyperlipidemia?
What is the ICD-10 code for awaiting placement?
What is the ICd 10 code for urgent care?
Urgent care center as the place of occurrence of the external cause 1 Y92.532 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. 2 Short description: Urgent care center as place 3 The 2021 edition of ICD-10-CM Y92.532 became effective on October 1, 2020. 4 This is the American ICD-10-CM version of Y92.532 - other international versions of ICD-10 Y92.532 may differ.
When will ICd 10 CM Y92.532 be released?
The 2022 edition of ICD-10-CM Y92.532 became effective on October 1, 2021.
When will the new ICd 10 codes be released?
These new codes went into effect on January 1, 2021 and replace existing codes that are not specific to COVID-19. Condition. 2020 ICD-10.
What is the code for MIS?
Two additional codes were also announced: M35.81 (Multisystem inflammatory syndrome (MIS)) and M35.89 (Other specified systemic involvement of connective tissue).
When will the ICd 10-CM Z01.89 be released?
The 2022 edition of ICD-10-CM Z01.89 became effective on October 1, 2021.
What is a Z00-Z99?
Categories Z00-Z99 are provided for occasions when circumstances other than a disease, injury or external cause classifiable to categories A00 -Y89 are recorded as 'diagnoses' or 'problems'. This can arise in two main ways:
What is S9088 in medical billing?
S9088: Services Provided in an Urgent Care Center: This S code allows urgent care centers to code and get reimbursement for the extra expenses involved in providing urgent care services.
What is CPT code for cerumen impaction?
Coding Cerumen Impaction (CPT = 69210 ): How does one code for ear wax impaction?
Is global billing the same as urgent care?
Click to expand... Global billing is the same for urgent care as any other office. You do code the same as a primary physician office with the exception that your place of service code is 20 (urgent care) instead of 11 (office). A.
Is urgent care coding complicated?
Medical coding in urgent care centers can be quite complex. Our coders frequently answer questions about urgent care coding for customers. In order to help you with coding in your urgent care, we have placed some of our answers online for educational purposes. Feel free to click on the links below to see answers about specific issues.
How to handle urgent care billing?
You have two main options when it comes to handling your urgent care billing: hiring in-house coders and billers or outsourcing the process to a professional. Both will require software licenses and other expenses. While some like having full control over the billing process, having in-house billers and coders tends to be more costly. You will have to pay salary and benefits to in-house employees, and an absence or unexpected employment termination can seriously affect your process.
Why do urgent care providers outsource?
Convenience is one of the main reasons that urgent cares choose to outsource. A billing provider handles all the data entries, fixes rejected claims, and sends invoices to the patient. Data transfer is seamless with the help of an EHR interoperability system.
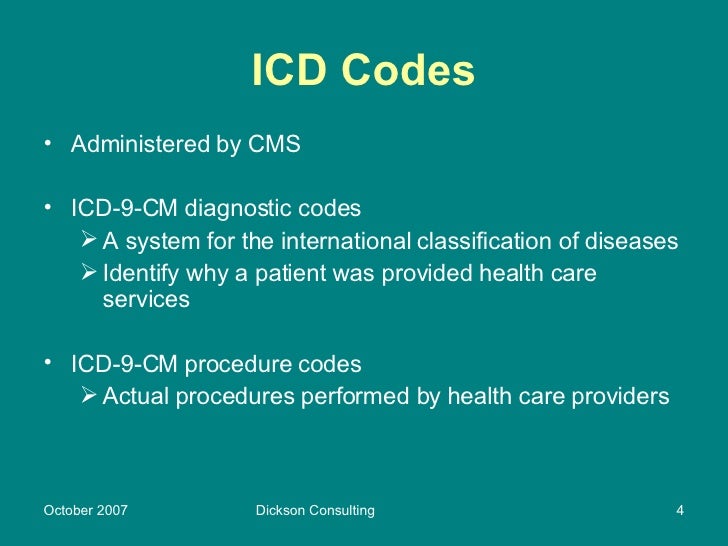
What is the difference between CPT and ICD-10?
Once a patient encounter is complete, a coder typically translates all the diagnoses and procedures into medical code sets universally used by the medical industry (i.e., ICD 10, CPT). ICD-10 codes provide a diagnosis, while current procedural terminology (CPT) codes designate any procedures that a provider used in the process of delivering care. CPT codes are used in conjunction with an ICD (diagnosis) code for the purposes of creating patient bills. CPT codes come in one of three categories:
How much is urgent care worth in 2023?
That’s probably why they’re increasing in popularity and are expected to be worth $26 billion by 2023 . To command your fair share of the market, you have to understand the basics of billing and how you can optimize your workflows for maximum returns.
What is a Category 2 code?
Category 2 codes are supplemental, quality assurance codes that are optional and not a replacement for Category 1 codes.
Can urgent care be reimbursed by Medicare?
Medicare uses a special facility code for urgent care centers (POS-20), but it still processes claims as if it were a primary care office (i.e., using codes POS-10 or POS-11). Medicare will reimburse urgent care for services rendered, but it’s important to note that it may not reimburse facilities for the naturally higher costs of providing walk-in care. As such, health care providers who wish to increase practice revenue should maximize the amount of patients who are privately insured.
Do urgent care clinics have to call insurance?
An urgent care clinic does not always have the time to call insurance companies to obtain pre-authorization for services. Patients should be familiar with their plan information and know what kinds of costs they can expect to incur from a walk-in facility. To avoid potential billing issues, it is important for each patient to sign an affidavit of financial responsibility prior to receiving medical services.
What is the status indicator for CPT codes 99050, 99051, 99053, 99056
The Centers for Medicare and Medicaid Services (CMS) considers reimbursement for CPT codes 99050, 99051, 99053, 99056, 99058 and 99060 to be bundled into payment for other services not specified.These codes have a Status Indicator of “B” in the National Physician Fee Schedule (NPFS). Consistent with CMS, Medica considers these codes not eligible for reimbursement.
What is the after hours and weekend care policy?
A:The After Hours and Weekend Care policy is intended to reimburse participating primary care providers for services that are outside their regular posted business hour as an alternative to more costly emergency room or urgent care center services. Reimbursement for CPT codes 99053, 99056, 99058 or 99060 would not accomplish this purpose and are not reimbursed by CMS.
What is CPT 99050?
CPT 99050 is reported when services are provided in the office at times other than regularly scheduled office hours or days when the office is normally closed. The Health Plan refers to this time as “After Hours,” and defines “After Hours” as services rendered between 5:00 p.m. and 8:00 a.m.
What is 99051 service?
99051 Service (s) provided in the office during regularly scheduled evening, weekend, or holiday office hours, in addition to basic service.
Is CPT code 99051 a separate reimbursement?
CPT code 99050 is not eligible for separate reimbursement when it is reported with a preventive diagnosis and/or a preventive service.CPT code 99051 is reported when services are provided in the office during regularly scheduled evening, weekend, or holiday office hours.
Can RVUs be used for Medicare?
If RVUs are shown, they are not used for Medicare payment. If these services are covered, payment for them is subsumed by the payment for the services to which they are incident. (An example is a telephone call from a hospital nurse regarding care of a patient).
Is CPT code 99050 bundled?
Although CMS considers CPT code 99050 to be bundled into the payment for other services provided on the same day, Oxford will provide additional compensation to participating primary care providers for seeing patients in situations that would otherwise require more costly urgent care or emergency room settings by reimbursing CPT code 99050 in addition to basic service codes.
Popular Posts:
- 1. icd 10 code for glioblastoma multiforme
- 2. icd 10 code for chronic right knee periprosthetic infection
- 3. icd code for ischemic stroke
- 4. icd 9 code for cerebral palsy diplegia
- 5. icd 10 code for admit b12 injection
- 6. what is the icd 10 code for acute appendicitis due to nausea and vomiting\
- 7. icd 10 code for contusion to little finger
- 8. icd 10 code for acute on chronic hypoxemic respiratory failure
- 9. icd 10 code for ankle ulcer left
- 10. what is the icd 10 code for carotid artery stenosis